Social Work Practice with Carers


Case Study 1: Eve
Download the whole case study as a PDF file
Eve is a carer for her father, who has early stage vascular dementia and numerous health problems. She has two children: a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15.
This case study considers issues around being a ‘ sandwich carer’ – that is, caring for both a parent and a child – maintaining employment and working with a whole family including family group conferences, as well as the impact of dementia and the role of assistive technology .
When you have looked at the materials for the case study and considered these topics, you can use the critical reflection tool and the action planning tool to consider your own practice.
- One-page profile
- Support plan
Transcript (.pdf, 61KB)
Name : Eve Davies
Gender : Female
Ethnicity : White British
Download resource as a PDF file
First language : English
Religion : None
Eve lives in a town. She has two children, a son, Matt, who is 17 and has Crohn’s disease, and a daughter, Joanne, who is 15. Eve’s mother died four years ago, and her father, Geoff, lives close by. Geoff has early stage vascular dementia and numerous health problems relating to a heart attack he had two years ago. Eve works part time in an administration role at a local college. She has lost contact with her friends and lost touch with her hobbies (swimming and singing in a choir) because she has prioritised her family.
Matt is at college studying for his A levels. He is frustrated that his illness is interfering with all aspects of his life. Joanne is becoming more withdrawn and resentful as an increasing amount of Eve’s time is taken up with other family members. Geoff has started to neglect himself at home, and is finding it more difficult to carry out daily tasks. Following a social care assessment, he has a befriending service stop by every week and a homecare team each morning to check he’s ok and supervise his medication, which Eve sets up for them. The care agency have reported that there’s a possibility Geoff has been accessing his medication and taking it. Geoff remains adamant that he is fine, and with Eve’s support he can manage.
Eve is feeling stressed and isolated. She wants to increase her working hours for financial reasons, but is unable to as she needs to be available for Geoff. Eve is having problems with sleeping and feels generally run down, and recently has been suffering from stomach pain and nausea. She says that she feels ‘withdrawn from normal life.’ She tried attending a carers’ group but found that listening to other carers’ problems highlighted her own. Instead, she sometimes uses an online forum at night when everyone else is asleep.
Eve was recently referred by her GP for a carer’s assessment. You have been out to see her twice and talked to her children. You have completed the assessment and support plan with her.
Back to Summary
What others like and admire about me
Good mum (mostly!)
I’m very organised
People can count on me
I help people out
I’m a good singer
What is important to me
My kids – I want them to be happy
Family time
Dad staying at home – I promised Mum
My job – people I work with
Health – exercise, sleep!
Just to know I’m not on my own
How best to support me
Listen to me and include me in your network
A bit of ‘me time’ to breathe – see friends, swimming, choir
Be honest about what you can do and do what you say you will
Don’t lumber your problems on me when there’s nothing I can do
Talk to me about me, not just about caring
Let me know who to contact
Don’t give me loads of information
Emails not phone please
Don’t arrange meetings when I’m at work
Help me plan so I can do everything!
Date chronology completed 15 February 2016
Date shared with person 15 February 2016
| 15.02.74 | Evelyn Mary Davies (known as Eve) born in Welsh border town. | |
| 12.04.96 | Married to Eric Sanderson and moved to Moreton. | |
| 26.07.98 | Birth of first child, son, Mathew Eric Sanderson. | |
| 18.09.00 | Birth of second child, daughter, Joanne Rachael Sanderson. | |
| 16.09.03 | Divorced. Reverted to maiden name though children retained their father’s name. | Eve and children remain in the marital home. Eve is proud of how well she has managed, with her part-time post which she enjoys and regular child support from the children’s father. Eve says she was not unduly concerned when initial fortnightly contact between the children and their father began to tail off. The children did not wish to travel to his new location some 50 miles away and he did not make sufficient effort in her view to see them. |
| 03.07.09 | Son, Matt, diagnosed with Crohn’s disease which causes him to frequently need the toilet, and have some faecal incontinence. He has relapses causing dramatic weight loss and frequent hospital admission. | Eve managed the health care and hospital appointments for her son as well as providing reassurance. Eventual diagnosis indicates a need for longer term health service involvement. Eve values the support of school nurse and feels that physically Matt’s illness is under control more now though the stigma and embarrassment of Matt’s illness has begun to take its toll on his emotional wellbeing. |
| 21.01.12 | Eve’s mother, Margaret, died suddenly in her sleep having suffered a heart attack. Eve herself is shocked by her mother’s death and describes her father as struggling to cope with his wife’s sudden death. | Eve now includes her father’s shopping in her weekly shop, prepares his evening meals, helps with laundry and other household chores, juggling this with her own chores and Matt’s health appointments. |
| 19.03.14 | Eve’s father, Geoff, had a heart attack. Hospitalised for two weeks whilst a stent was fitted and his recovery monitored. | His heart attack has left Eve’s father with numerous related health problems. Eve begins to manage of her father’s health appointments alongside management of Matt’s. Over the next year Geoff starts to have memory problems. |
| 16.11.15 | Eve’s father diagnosed with early stage vascular dementia. Social care assessment undertaken. Befriending service and home care provision arranged.
| Mixed service with Eve as main carer for her father, Geoff Davies, and some home care and befriending service provision to Geoff now in place. At this time Eve tried attending a carers’ group but found that listening to other carers’ problems highlighted her own. Instead, she sometimes uses an online forum at night when everyone else is asleep. |
| 29.01.16 | Eve attends her GP surgery as she is regularly feeling nauseous. The GP asked Eve if she is experiencing more stress than usual. Eve expresses concern that her father has started to neglect himself at home, and is finding it more difficult to carry out daily tasks. He gets confused with tasks like making a meal. Eve worries that he doesn’t eat properly. Sometimes he has trouble remembering words and this makes him feel cross. Eve explains that he sometimes now has short bursts of sudden confusion. She finds this frightening and her children do too, which worries her. | Following this discussion with Eve about the pressures on her at the moment and indications of stress causing her physical symptoms, with her agreement the GP has referred Eve for a social care assessment as carer for both her father and her son.
|
| 04.02.16 | Initial visit by social worker. SW sees Eve on her own at home. | SW makes another appointment to continue the assessment at a time when the children are at home to include them in the conversation. |
| 09.02.16 | Second visit to Eve and conversation with her children. | Carer’s assessment and support plan completed. SW arranges with Geoff that he will have an assessment in the next few weeks. |
| 15.02.16 | Paperwork completed. | Sent to Eve. |
Eve’s Ecogram
Name Eve Davies
Address 1 Fir Avenue, Moreton, ZZ1 Z11
Telephone 012345 123456
Email [email protected]
Gender Female
Date of birth 15.2.1974 Age 42
Ethnicity White British
First language English
Religion None
GP Dr Tailor, Parkside Surgery
How would you like us to contact you?
Do you need any support with communication?
About the person/ people I care for
My relationship to this person Daughter
Name Geoff Davies
Address 1 Pine Avenue, Moreton, ZZ1 Z22
Telephone 012345 234567
Gender Male
Date of birth 8.1.1943 Age 73
Religion Baptised C of E
Please tell us about any existing support the person you care for already has in place. This could be home care, visits or support from a community, district or community psychiatric nurse, attending any community groups or day centres, attending any training or adult learning courses, or support from friends and neighbours.
Home care every morning for medication and check up
Befriending service 2 hours a week
My relationship to this person Mother
Name Matt Sanderson
Address 1 Fir Avenue, Moreton, ZZ1 Z22
Date of birth 26.7.1998 Age 17
Goes to college (doing A levels)
GP and nurse at the surgery
Consultant at the hospital
The things I do as a carer to give support
Please use the space below to tell us about the things you do as a carer (including the emotional and practical support you provide such as personal care, preparing meals, supporting the person you care for to stay safe, motivating and re-assuring them, dealing with their medication and / or their finances).
Dad has early stage vascular dementia and numerous health problems relating to a heart attack he had two years ago. He has started to neglect himself at home, and is finding it more and more difficult to carry out daily tasks. He gets confused with cooking or tasks like making a meal. Sometimes Dad has trouble remembering words and this makes him feel cross. On occasion he does experience short bursts of sudden confusion, which can be frightening for other family members.
Following a social care assessment, he has a befriending service stop by every week and a homecare team each morning to check he’s ok and supervise his medication.
This is what I do for Dad:
- Preparing Dad’s medication for the day – setting out in reminder containers
- Greeting care workers in the morning
- Remind Dad about having a wash
- Leave lunch in fridge
- Remind Dad about appointments
- Visit in the evening and cook dinner
- Sort out problems with the care agency
- Do shopping, cleaning, laundry
- Collect medication
- Check for medical appointments/ reviews
- Take Dad to appointments
- Sort out Dad’s mail – pay bills
- Fix things round the house
- Sort out extra care if Matt is in hospital
Matt has Crohn’s disease. He is at college studying for his A levels. He is doing well but his illness does interfere with his life and he can get frustrated about this. He wants good grades to be able to become a journalist and move abroad. It is embarrassing for him that he has to frequently rush to the toilet, and occasionally he is incontinent. Matt has regular relapses. This causes him to lose a lot of weight and he has been in hospital three times in the last year and missed college.
This is what I do for Matt:
- In the morning, make special lunch and ensure that he has his emergency bag (extra clothing, wipes, plastic bag and air freshener)
- Remind him about his weekly blood test appointment.
- Extra washing
- Help with homework
- Transporting Matt to hospital/GP/nurse appointments.
I also look after my daughter Joanne who is 15.
How my caring role impacts on my life
Please use the space below to tell us about the impact your caring role has on your life.
Like all working mums I have a lot on. As I have had to do more for Dad, it has got more difficult to juggle family chores and work.
I want to increase my working hours for financial reasons but I don’t see how I can at the moment, as Dad’s care needs are increasing and I need to be available for him. I’ve had to take some flexible working hours recently to cover last minute changes in arrangements for Dad’s care. I frequently have to take phone calls at work about care arrangements. I am concerned that I won’t be able to keep working and we need the money.
I’m worried that Dad isn’t eating properly. The care agency have reported that the medication audit has shown that Dad might have been taking his medication at the wrong times. Dad doesn’t want to talk about longer term planning and making advanced decisions. He does not want any more social care provision in the house. This really worries me particularly as Dad will need more help as time goes on. Also if Dad suddenly needed a lot more help or I was unwell then I am not sure how we would manage.
I want Matt to be able to manage his illness better so that he is happier and able to do the things he wants. As I have had to spend more time with Dad and Matt, my daughter Joanne has become more distant. She finds it difficult that we need to work around what Matt needs, for example for meals. Joanne has always been helpful but has become more withdrawn and resentful. She has started to hang around with older teenagers, and I’m worried they might be ‘leading her astray’. She has had a few letters from school mentioning poor attendance and a drop in her grades. I feel like I don’t have time at the moment to be a good mum.
I’m having problems with sleeping and feel generally run down, and recently I have had to see the GP about stomach pain and nausea, which she thinks is to do with stress. I feel like I don’t have any time now to just breathe and am withdrawing from normal life. I don’t currently have time to exercise – I used to swim, or to sing in the choir. I’ve also lost contact with friends so I feel quite isolated.
What supports me as a carer?
Please use the space below to tell us about what helps you in your caring role.
I sometimes go on an online carers’ forum at night when everyone else is asleep and that’s quite helpful. I did try attending a carers’ group but it got me down listening to other people’s problems.
Work gives me a bit of a break from caring and my boss has so far been quite supportive with flexible working though I don’t want to push it.
Matt’s nurse at the GP surgery has been really helpful with information and support. Matt gets on with her well.
My feelings and choices about caring
Please use the space below to tell us about how you are feeling and if you would like to change anything about your caring role and your life.
It’s my choice to care for my family and I want to keep on doing that, and be a good mum and a good daughter.
If I knew that Dad was getting the care he needs and that we had a plan for the future then I would manage much better.
At the moment I’m feeling stressed and quite overwhelmed. There’s always something else to sort out. I feel like I don’t have anyone to support me. I miss my Mum and worry about whether I’m looking after my Dad as well as she did.
I want to know my family is ok. I don’t want to stop looking after my kids and my Dad.
I want to be able to manage my different roles at home and at work, and to do things well.
I want to have more time with my children and we want more time as a family.
I would love to increase my hours at work.
I’d like to start swimming and join the choir again. I’d like to see friends sometimes.
I do need more sleep.
Information, advice and support
Let us know what advice or information you feel would help you and what sort of support you think would be beneficial to you in your caring role.
Someone to talk to Dad about getting the care he needs – particularly to ensure he takes the right medication and that he eats enough.
Some help with planning Dad’s care in case there is a crisis, and to plan ahead for what he will need in the future.
Someone to check on Dad when I’m at work.
A break – just to be free without interruptions.
Some back-up so that I am not always on call.
Someone to talk to about how to manage all of this.
Someone for Joanne to talk to if she wants to.
Someone to support Matt to manage his illness so he can achieve his aims.
To be used by social care assessors to consider and record measures which can be taken to assist the carer with their caring role to reduce the significant impact of any needs. This should include networks of support, community services and the persons own strengths. To be eligible the carer must have significant difficulty achieving 1 or more outcomes without support; it is the assessors’ professional judgement that unless this need is met there will be a significant impact on the carer’s wellbeing. Social care funding will only be made available to meet eligible outcomes that cannot be met in any other way, i.e. social care funding is only available to meet unmet eligible needs
Date assessment completed 15 February 2016
Social care assessor conclusion
Eve is providing significant support to her father and her two children, one of whom has Crohn’s disease. Eve also works part-time. Eve’s father has some support from home care and a befriending service. Her son has support from health services. Eve is very organised, and juggles chores and work well. However, she says that she is starting to feel increasingly stressed and this is having an impact on her health. She is also quite isolated and has no time at present to have a break from caring. Eve would like to continue supporting her family and increase her working hours, as well as having some time for her own interests. It is important to Eve that her father remains at home and is safe, and that her children are happy. Eve would benefit from support to enable her to manage the demands on her, and to have some time for herself. She would also benefit from some emotional support for her and for her family. This will enable her to continue as a carer and to improve her health and wellbeing.
Eligibility decision Eligible for support
What’s happening next Create support plan
Carry out assessment for Mr Geoff Davies
Completed by
Organisation
Signing this form (for carer)
Please ensure you read the statement below in bold, then sign and date the form.
I understand that completing this form will lead to a computer record being made which will be treated confidentially. The council will hold this information for the purpose of providing information, advice and support to meet my needs. To be able to do this the information may be shared with relevant NHS Agencies and providers of carers’ services. This will also help reduce the number of times I am asked for the same information.
If I have given details about someone else, I will make sure that they know about this.
I understand that the information I provide on this form will only be shared as allowed by the Data Protection Act.
Date of birth 15.2.1974 Age 42
Support plan completed by
Support Plan
|
| ||
|
|
| |
|
| ||
|
|
| |
|
|
| |
|
| ||
|
| ||
|
|
|
Date of support plan: 15 February 2016
This plan will be reviewed on: 15 February 2017
Signing this form
Eve has given consent to share this support plan with Mr Davies. This support plan will link into his assessment.
Sandwich caring
The Care Act places a duty on local authorities to assess adult carers, including parent carers of disabled and other children in need, before the child they care for turns 18, so that they have the information they need to plan for their future. Guidance, advocating a whole family approach, is available to social workers (LGA 2015, SCIE 2015, ADASS/ADCS 2011).
- Carers UK (2012) Sandwich caring
- Circle (2018) Supporting carers to work and care
- Think Local Act Personal (2017) Supporting working carers
- Mumsnet for the Care Quality Commission August (2014) Care Quality Commission: Sandwich Generation Survey Summary Report
- Institute for Public Policy Research (2013) The sandwich generation: older women balancing work and care
- Carers UK (2014) Carers at breaking point
- Blog: Impact of cuts
Carers’ employment
Research shows that both emotional and practical support from social workers are valuable, for example when looking at what was valued by the mothers of transition-age children with mental illness (Gerten and Hensley 2014) and by men as caregivers to the elderly (Collins 2014).
- Skills for Care (2013) Balancing work and care
- Carers UK (2015) Caring and isolation in the workplace
- Carers UK (2014) The case for care leave
- Carers UK (2014) Supporting employees who are caring for someone with dementia
- Carers UK (2013) Supporting working carers
- NIHR (2014) Improving employment opportunities for carers: identifying and sharing good practice
- Department of Health (2015) Pilots to understand how to support carers to stay in paid employment
- Tool 1: Support for carers in employment
Life course and whole family approaches
The whole family approach is a strong theme in the research (LGA 2015) along with relationship based practice (SCIE 2016, Cooper 2015, Wilson et al 2011, Ruch et al 2010). Family group conferencing, along with mediation as whole family approaches, were found to have particular applicability to adult safeguarding social work. (SCIE 2012).
- Beth Johnson Foundation (2014) A life course approach to promoting positive ageing
- SCIE (2012) At a glance 62: Safeguarding adults: Mediation and family group conferences
- Hobbs A and Alonzi A (2013) Mediation and family group conferences in adult safeguarding, Journal of Adult Protection, 15(2) , pp.69-84
- Carers Trust Whole family approach – practice examples
- Tool 2: Family group conferences
Assistive technology
Evidence points to the need for social work teams are to have good information about the support available to carers. National materials offer a valuable resource to social workers seeking to research how to work with their clients and their carers which can be supplemented locally and from the active contributions of the ‘online’ community (Young Sam Oh 2015).
- SCIE (2010) At a glance 24: Ethical issues in the use of telecare
- Carers UK and Tunstall (2013) Potential for Change: Transforming public awareness and demand for health and care technology
- Carers UK and Tunstall (2012) Carers and telecare
- Carers UK (2012) Future care: Care and technology in the 21st century
- SCIE (2010) Telecare videos
- Tool 3: Ethics of assistive technology
Research suggests an assets or strengths based approach to social work support with the person and their family and/or network of support. The Manual for good social work practice (DH 2015) uses a timeline as a model that can underpin how the social worker supports and intervenes, from early preventative measures through various stages of loss towards end-of-life. Three critical points on the timeline – diagnosis, taking up active caring and the decline of the person’s capacity – are identified. It is important for social workers to assess the carers needs, sustain the carers own identity, develop and maintain their network of support and resources, and access financial and legal advice.
- SCIE Dementia Gateway Department of Health (2015) TCSW (2015) A manual for good social work practice: Supporting adults who have dementia , The College of Social Work
- Carers Trust (2014) The Triangle of Care: Carers Included: A Guide to Best Practice for Dementia Care
- Carers Trust (2013) A Road Less Rocky – Supporting Carers of People with Dementia
- Alzheimer’s Research UK (2015) Dementia in the family: the impact on carers
- Tool 4: Triangle of care – self-assessment for dementia professionals Carers Trust (2014) The Triangle of Care: Carers Included: A Guide to Best Practice for Dementia Care (Page 22 Self-assessment tool for organisations)
Tool 1: Support for Carers in Employment
You can use this tool with carers to think about what would support someone to manage work and caring responsibilities.
|
| ||
| Supportive manager
| ||
| Flexible/ special leave arrangements
| ||
| Flexible working hours
| ||
| Remote working
| ||
| Information and support for carers at work
| ||
| High quality, appropriate care and support
| ||
| Support from relatives and friends
| ||
| Services that are available outside working hours
| ||
| Help with coordinating care and support
| ||
| Advice and information about legal & money issues
|
This tool is based on research about what helps carers who are working (Carers UK (2015) Caring and isolation in the workplace).
Tool 2: Family Group Conference
This tool sets out the process for a Family Group Conference. You can use it to plan and hold a conference.
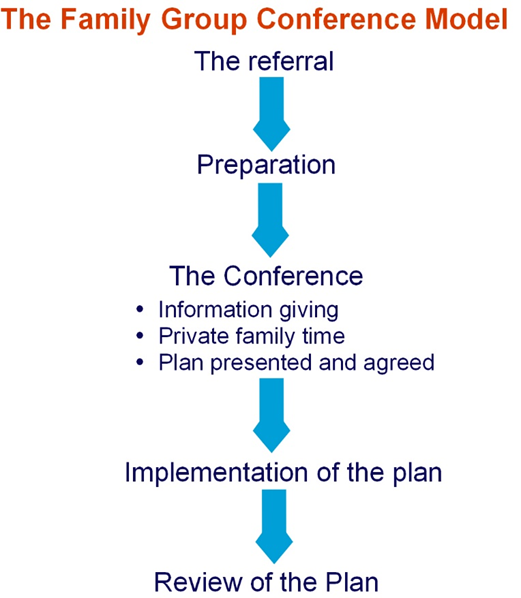
The Family Group Conference process
Stage 1: The referral
Whether or not a family group conference takes place is a decision made by the family. Under no circumstances can a family be made or forced to have a family group conference.
Once a referral for a family group conference is made, there will need to be a co-ordinator to liaise with the family.
The co-ordinator helps the family to plan the meeting and chair the meeting. The co-ordinator is different from the referrer and acts as a neutral person. The co-ordinator will not influence the family to make a particular decision but will help them to think about the decisions that need to be made. Families should be offered the opportunity to request a co-ordinator who suitably reflects their ethnicity, language, religion or gender, and the family’s request should be accommodated wherever possible.
Stage 2: Preparation
The co-ordinator organises the meeting in conjunction with the family members and other members of the network. This can include close friends.
- The co-ordinator discusses with the person with care and support needs how they can be helped to participate in the conference and whether they would like a supporter or advocate at the meeting . The supporter/advocate will then meet with them in preparation for the meeting.
- The co-ordinator meets with members of the family network, discusses worries or concerns, including how the family group conference will be conducted, and encourages them to attend.
- the wellbeing concerns which need to be considered at the family group conference. This includes identifying any bottom line about what can, and, importantly, cannot be agreed as part of the plan from the agency’s perspective.
- services that could help.
- The co-ordinator negotiates the date, time and venue for the conference, sends out invitations and makes the necessary practical arrangements.
Stage 3: The conference
The family group conference follows three distinct stages.
a) Information giving
This part of the meeting is chaired by the co-ordinator. They will make sure that everyone is introduced, that everyone present understands the purpose and process of the family group conference and agrees how the meeting will be conducted including, if felt helpful by those present, explicit ground rules. The service providers give information to the family about:
- the reason for the conference;
- information they hold that will assist the family to make the plan;
- information about resources and support they are able to provide;
- any wellbeing concerns that will affect what can be agreed in the plan; and
- what action will be taken if the family cannot make a plan or the plan is not agreed.
The family members may also provide information, ask for clarification or raise questions.
b) Private family time
Agency staff and the co-ordinator are not present during this part of the conference. Family members have time to talk among themselves and come up with a plan that addresses concerns raised. They will identify resources and support which are required from agencies, as well as within the family, to make the plan work.
c) Plan and agreement
When the family has made their plan, the referrer and the co-ordinator meet with the family to discuss and agree the plan including resources.
It is the referrer’s responsibility to agree the plan of action and it is important that this happens on the day of the conference. It should be presumed that the plan must be agreed unless it puts anyone at risk of significant harm. Any reasons for not accepting the plan must be made clear immediately and the family should be given the opportunity to respond to the concerns and change or add to the plan.
It is important to ensure that everyone involved has a clear understanding of what is decided and that their views are understood.
Resources are discussed and agreed with the agency concerned, and it is important that, at this point, timescales and names of those responsible for any tasks are clarified. Contingency plans, monitoring arrangements and how to review the plan also need to be agreed.
The co-ordinator should distribute the plan to family members involved and to the social worker and other information givers/relevant professionals.
1.3.5 Stage Three: Implementation of the Plan
It is essential that everybody involved implements their parts of the plan within agreed timescales and communicate and addresses any problems that arise.
1.3.6 Stage Four: Review of the plan
There should be a clear process for reviewing the implementation of the plan. A review family group conference or other meeting should be offered to the family so they can consider how the plan is working, and to make adjustments or change the plan if necessary.
This information is based largely on the Family Rights Group’s Family Group Conference Process
Tool 3: Ethics of using assistive technology
This tool highlights the ethical issues of using assistive technology. You can use it to consider when assistive technology would be beneficial for someone, and to reflect on the benefits and drawbacks of it more generally.
What are the ethical issues about using assistive technology (AT) to support carers?
This tool is based on SCIE At a glance 24: Ethical issues in the use of telecare

Download The Triangle of Care as a PDF file
The Triangle of Care Carers Included: A Guide to Best Practice in Mental Health Care in England
The Triangle of Care is a therapeutic alliance between service user, staff member and carer that promotes safety, supports recovery and sustains wellbeing…

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility


- Compare CSWE Accredited Online MSW Programs
- Advanced Standing MSW Programs
- Discover HBCU MSW Programs Online & On-Campus
- On-Campus MSW Programs
- Fast Track MSW Programs
- Hybrid MSW Programs
- Full-time online MSW programs
- Part-Time Online MSW Programs
- Online Clinical Social Work Degree Programs (LCSW)
- Doctorate in Social Work (DSW) Programs Online
- Online Military Social Work Programs
- Considering a Major in Social Work?
- Ph.D. in Social Work Online
- Schools By State
- Sponsored: Fordham University
- Sponsored: University of Denver
- Sponsored: Simmons University
- Sponsored: Case Western Reserve University
- Sponsored: Howard University
- Sponsored: Simmons University – DSW Online
- How Long Does It Take to Become a Social Worker?
- 2022 Study Guide to the Social Work Licensing Exam
- How to Become a Veterinary Social Worker
- How to Become a LCSW
- How to Become a School Social Worker
- Become a Victim Advocate
- Social Worker Interviews
- Is a Master of Social Work (MSW) worth it?
- Social Work Salaries – How Much Do Social Workers Make?
- Bachelor’s in Psychology Programs Online
- Concentrations in Online MSW Programs
- Social Work: Core Values & Code of Ethics
- Introduction to Social Learning Theory
- Introduction to Systems Theory
- Introduction to Psychosocial Development Theory
- Introduction to Psychodynamic Theory
- Introduction to Social Exchange Theory
- Introduction to Rational Choice Theory
- What is Social Justice?
- What is Social Ecology?
Online MSW Programs / Guide to Careers in Social Work / Geriatric Social Work: A Guide to Social Work with Older Adults
Geriatric Social Work: A Guide to Social Work with Older Adults

In this article:
- What is a Geriatric Social Worker?
How to Become a Geriatric Social Worker
What does a geriatric social worker do, where do geriatric social workers work, the challenges and rewards of gerontological social work, what is a geriatric social worker.
Gerontological social workers, also known as geriatric social workers, coordinate the care of older patients in a variety of settings, including hospitals, community health clinics, long-term and residential health care facilities, hospice settings, and outpatient/daytime health care centers.
The American Geriatrics Society projects that about 30% of Americans ages 65 and over will need geriatric care by 2030 (PDF, 500 KB) . As the need for geriatricians grows, so will the role of social workers in elderly care.
In outpatient settings, geriatric social workers are advocates for the older adults, ensuring they receive the mental, emotional, social and familial support they need, while also connecting them to resources in the community that may provide additional support. In inpatient and residential care settings, they conduct intake assessments to determine patients’ mental, emotional and social needs; collaborate with a team of physicians, nurses, psychologists, case managers and other health care staff to develop and regularly update patient treatment plans; discuss treatment plan options with patients and their families; and manage patient discharges.
This guide features interviews with gerontological social workers. All interviewees were compensated to participate.
Role of Social Workers in Elderly Care
Those who work in geriatric social work help their clients manage psychological, emotional and social challenges by providing counseling and therapy, advising clients’ families about how to best support aging loved ones, serving as the bridge of communication between clients and the rest of the care team, and ensuring that clients receive the services they need if or when they move between inpatient and outpatient treatment programs, in-home care, day treatment programs, and the like.
The role of social workers in elderly care leads to unique opportunities, which include making deep and meaningful connections with clients and their families, changing problematic systems at both the personal and community levels, and the knowledge that their work has a direct positive impact on those in need.
Education Requirements
A bachelor’s degree in social work from an accredited university is the minimum education requirement for those seeking credentials in gerontology . Those who want to become a social worker for older adult clients often seek a Master of Social Work (MSW) with a clinical concentration . These programs help prepare students to become licensed clinical social workers (LCSW). In addition to foundation level social work courses, they focus on the skills needed to provide social work services and treatment to individuals (children, youth and adults) and small groups (couples and families).
Students learn about advanced assessment techniques, diagnosing and treating psychosocial problems, and developing, promoting and restoring mental health and social functioning. Students are also taught how to evaluate their own practice and intervention techniques.
According to the Bureau of Labor Statistics (BLS), the 2020 median pay for social workers was $51,760 per year. The highest-paid 10% of social workers earned more than $85,820, while the lowest 10% earned less than $33,020. The annual mean wage of health care social workers was $57,630 in 2020, the BLS reports. This is the average geriatric social worker salary as well, since the BLS considers geriatric social workers as part of the health care social worker group.
Employment of social workers is projected to grow 12% from 2020 to 2030, much faster than the average for all occupations, according to the BLS. Increased demand for health care and social services will drive employment growth, but the prospects of each specialization, such as geriatric social workers, will vary.
Below are six common steps to become a geriatric social worker:
- Earn a bachelor’s in social work or in a related field.
- Pursue an MSW with relevant coursework.
- Seek an internship in an adult health care setting and complete the required fieldwork.
- Take the licensing exam.
- Earn relevant certifications.
- Apply for state social work licensure.
Sponsored Online MSW Program

Simmons University
Simmons school of social work (ssw).
Aspiring direct practitioners can earn their MSW online from Simmons University in as few as 9 months . GRE scores are not required, and the program offers full-time, part-time, accelerated, and advanced standing tracks.
- Prepares students to pursue licensure, including LCSW
- Full-time, part-time, and accelerated tracks
- Minimum completion time: 9 months
info SPONSORED
Due to the medical, social, emotional and mental health challenges that senior citizens face, those interested in entering the field of geriatric social work may need a master’s in social work degree from an institution accredited by the Council on Social Work Education , and to complete graduate-level field internships in settings that serve geriatric patients and older adults in need. Courses that may be helpful in this field include clinical social work modalities, family dynamics and social work in medical settings. Classes that focus on the physical, mental, emotional, financial and social issues associated with aging are also important. Students may wish to find MSW programs that provide a selection of gerontology-focused classes, or an academic concentration in gerontological social work.
“I highly recommend taking whatever gerontology-focused classes your program offers. A basic course in death and dying is a wonderful asset, even just for you personally,” noted Charis Stiles, MSW, who is a Friendship Line manager at the Institute on Aging (IoA) in San Francisco.
Even if a program does not have many gerontology-specific courses, thinking proactively about the therapeutic modalities and social work concepts that might be most useful in your work with geriatric clients, and taking courses that focus on these areas, may help you prepare.
“My favorite class in social work school was motivational interviewing, which is a technique of counseling where you use open-ended questions and don’t provide people with answers to their problems, but rather have them come up with the solutions themselves,” said Laura Burns, MSW, a medical social worker at On Lok Lifeways, a PACE program in San Jose, California. “In motivational Interviewing, the counselor mirrors the clients’ ideas back to them. This is a technique that I have used a lot in the hospital setting as well as my current job.”
Gaining experience working closely with geriatic clients and older adults through one’s graduate field placements and volunteer work and jobs is also an important part of preparing for a career in geriatric social work.
“I think some people really find it fascinating, and for others, it’s just not their cup of tea,” Burns said. “There are tons of ways to gain experience: reading books, watching movies, taking classes or training, and just talking with your own family. If you’re interested in geriatric social work, talk with your grandparents about their lives and their health problems.”
Burns also recommends students advocate for the types of field placements they want during their MSW program. “Field placement is a good way to get a variety of experience, but really if you know the type of work you want to do, be really, really clear about that during your program,” she said. “I knew that I wanted to work in health care, so I went and found internships in health care. I know some schools won’t let you do that, but thankfully, my school did.”
Stiles similarly advises social work students to gain relevant internship experiences during their graduate education, and to engage in extracurricular and volunteer work to interact with aging populations. “If you can find a placement with older adults, I highly recommend it. Adult day health care is a good first placement because you will get to interact with a large variety of older adults,” she said, adding, “Volunteering in settings like hospice, senior centers, or even the library may also be a good introduction to this population.”
Stiles and Burns also explained how the field of gerontological social work requires a degree of emotional preparation and skill in talking about weighty or disconcerting issues such as death and terminal illness.
“One aspect of geriatric social work that may be different than other kinds of social work is that death is a more constant presence in our participants’ lives,” Burns explained. “Everyone has a different level of comfort thinking and talking about death. Some of our participants think more about their deaths than others, yet we discuss it with all of them. We often begin these conversations by asking questions such as, ‘How do you want the end of your life to be?’ and ‘What would your goals be for the last weeks or last days here?’”
Stiles advised social work students to be self-aware and open to evaluating and changing their preconceived notions about older populations and geriatric care. “I recommend reflecting on your own attitudes toward older individuals and being honest with yourself about your assumptions about the later stages of life,” she said. “Many of us have some degree of internalized ageism even if we don’t recognize it, and this exploration will help us in any field we go into. As much as we don’t think about it, we are aging all the time.”
Those who enter geriatric social work need to know about the issues that aging populations encounter and have relevant experience working with aging populations. While working as a social worker for elderly patients, they will employ problem-solving skills, patience and compassion daily and contend with challenges such as the complexity and severity of the conditions, stubborn systemic barriers to care and family conflicts that can interfere with clients’ treatment. Despite these challenges, however, gerontological social workers experience the satisfaction of granting a voice to a marginalized population in need, and also enjoy deep and rewarding connections with clients who have led rich and intriguing lives, and who deeply appreciate the compassionate care that gerontological social workers provide.
Geriatric social workers support clients and their families through a combination of psychosocial assessments, care coordination, counseling and therapeutic work, crisis management and interventions, and discharge planning.
Psychosocial Assessments
Gerontological social workers conduct psychosocial assessments to determine their clients’ mental, emotional and social needs, and to understand how these needs connect with their physical health and medical conditions. Mental and physical health are closely linked, and by gaining a holistic picture of clients’ mental, emotional and social circumstances, social workers help clients’ medical care providers and their families better understand how to develop a care plan as comprehensive and compassionate as possible.
Psychosocial assessments gather information on a client’s:
- Mental and emotional health, including past and present psychological conditions.
- Behavioral health challenges.
- Social, financial, familial, educational and occupational history and current situation.
- Medical and mental health treatment history.
- Current medications and adherence to treatment plans.
Gerontological social workers complete psychosocial assessments at the time of a client’s admission into a given care program (this type of psychosocial assessment is called an intake assessment), and also conduct regular assessments throughout a client’s time in the program.
Burns explained to OnlineMSWPrograms.com how social workers evaluate multiple facets of clients’ cognitive, emotional, and behavioral health. “The social workers’ intake of a candidate is focused on the person as a whole and explores their support systems, psychosocial risks, cognition and mood,” Burns said. “The three main things that we assess for are changes in mood, behavior and cognition. We test for changes in cognition and mood every six months.”
Burns also noted that interacting closely with clients and connecting with them regularly allows her to evaluate their emotional and cognitive health at any point, and to convey any concerning changes to the treatment team. “[E]ach time I’m checking in on someone, even if it seems just like a social visit, I’m also checking in on their emotional well-being,” she said. “As social workers, we don’t just do formal screenings; we also do informal check-ins with the participants all the time. Also, we don’t have to wait until a participant is due for a formal assessment to make an adjustment in their care plan; we are able to modify it at any time.”
In addition to being essential for the development and improvement of a client’s care plan, psychosocial assessments help social workers determine whether a client is at risk of experiencing adverse mental, physical, and/or behavioral health outcomes—for example, if a client shows signs of depression, has suicidal tendencies, or is neglecting his or her medication. These evaluations of risk to clients, also known as risk assessments, help social workers and other members of a client’s care team determine the appropriate courses of action to address factors that may seriously compromise a client’s well-being.
Care Coordination
Another responsibility that gerontological social workers have is care coordination, which is the purposeful organization of different teams and services to effectively address a client’s overall health care needs (physical, cognitive, emotional, and social). Care coordination involves completing psychosocial assessments to inform the larger treatment team of a client’s needs. It also means participating in or facilitating meetings between different providers to discuss patient treatment and health outcomes; conveying the concerns and desires of the patient and his or her family to the teams involved in their care; and connecting clients and their caretakers with resources within the larger community that may provide additional support.
Counseling and Therapy
Gerontological social workers provide counseling and therapy to clients to help them cope with the psychological, emotional, social and financial challenges that come with aging. They also provide therapy and advise clients’ families and loved ones as necessary. During sessions with clients, social workers may employ a variety of psychotherapeutic techniques to help them manage negative emotions, set objectives for life improvement, address behavioral problems or psychological barriers to meeting certain goals, and (where applicable) make end-of-life preparations.
When working with the families of their clients, gerontological social workers may help them manage the difficulties they may encounter caring for an aging loved one, including strains on financial resources and relationships, and processing grief and other emotions around loss.
Specific therapeutic techniques gerontological social workers may use in their work with clients and families may include cognitive behavioral therapy and dialectical behavioral therapy, problem-solving therapy, motivational interviewing and mindfulness-based stress reduction. For more information about these and other therapeutic modalities social workers may use when providing clinical therapy to clients, see our Guide to Clinical Social Work or check out the National Association of Social Workers website .
Crisis Management and Interventions
Depending on their role and work setting, gerontological social workers may encounter a variety of client crises. Some clients may struggle with depression, suicidal desires, acute dementia that renders them unable to care for themselves, family conflicts about treatment decisions, traumatic experiences that require immediate support, or mental or emotional disorders that pose a danger to themselves or others. Clients may also be the victims of neglect, domestic abuse, exploitation and other crimes.
In these instances, gerontological social workers may have to intervene with a number of measures to ensure client safety and well-being. These may include providing emotional support and counseling to clients and their family members; managing difficult conversations among client, family and care providers; contacting relevant organizations and/or authorities in the case of elder abuse; and developing a short- and long-term support plan for clients and their loved ones.
Burns explained some of the crisis intervention services she provides at On Lok Lifeways. “Since we screen for changes in mood, if someone is doing fine emotionally and then all of a sudden they’re severely depressed or suicidal or homicidal, that’s obviously something to communicate immediately to the medical team and the participant’s family,” she said. “We consult with Adult Protective Services to report cases of abuse or neglect. We let their doctor know to see if they need to have a medication adjustment, and we’ll usually also recommend meetings with the chaplain or the mental health counselor who works on site as well.”
Gerontological social workers may also provide crisis support and interventions in non-medical settings. Stiles also helps the older adults during crisis situations by coordinating volunteer services for the IoA’s suicide prevention and grief support hotline.
“The Friendship Line at the Institute on Aging provides suicide prevention and trauma grief support to older adults and adults with disabilities. It’s a 24-hour hotline that operates from 8 a.m. to 8 p.m. in the office and after hours remotely,” she said “Callers are primarily over the age of 60 and are dealing with isolation, loneliness, depression, grief and illness. Many have mental health conditions, some treated and some untreated, and many also have a history of trauma. We have between 50-70 volunteers who are the primary hotline counselors.”
Resource Navigation and Benefits Application Guidance
Gerontological social workers also help clients and their families understand and apply for health care benefits and other financial or social assistance at the federal, state and local community levels. Clients and their loved ones may have a hard time navigating health insurance benefits, social security, and making use of community support systems. Social workers may guide clients through these steps and connect them with local support systems, such as senior centers, discounted or pro bono counseling, free community clinics, and subsidized food and housing if necessary.
Discharge Services
Consistent with their role as care coordinators, gerontological social workers often develop and coordinate a discharge plan for clients when the time comes for them to transition from one care setting to another—for example, from inpatient to outpatient care, or from residential care to home care. When coordinating a client’s discharge from a care setting, social workers typically contact the relevant parties involved in the transition and organize logistics such as transportation, health insurance and medical financial aid, and paperwork and documentation. They may also consult with the client and his or her family to prepare them for the change.
Geriatric social workers work with older populations in many settings. At any organization that serves the physical, mental, emotional and social needs of senior citizens, geriatric social workers may play a crucial role providing direct care (counseling and advising, resource navigation services, etc.), as well as care coordination (contacting different departments, care providers, and organizations to ensure clients get the inpatient or outpatient support they require). Common work environments that employ gerontological social workers include medical settings, adult health programs, programs for all-inclusive care for the, hospices, nursing homes and residential care facilities.
Hospitals and Medical Centers
Hospitals and medical centers typically have inpatient and outpatient divisions to support older patients who suffer from chronic or acute health conditions. For example, hospitals may have geriatric acute and emergency care units, fracture care centers, palliative care, and a geriatric oncology unit. Gerontological social workers may work in the geriatric departments of hospitals and medical centers as part of a specific unit or across multiple units.
Gerontological social workers who work at hospitals and medical centers collaborate with a larger medical team of physicians, nurses, medical assistants, psychologists and other staff. They evaluate patients’ needs, develop a treatment plan, coordinate geriatric patients’ care, and maintain and submit patient records and documentation. They also counsel patients and their families and help them navigate resources.
Some medical centers also have adult day health programs that provide daily activities, counseling and social support services to patients so they may remain at home instead of transitioning to a nursing home. Social workers in these settings may coordinate activities, programs and other services for their clients, provide counseling services and connect clients and their families to resources within or outside the program.
Programs of All-Inclusive Care for the Elderly
Programs of All-Inclusive Care for the Elderly (PACE) provide comprehensive medical, mental health and behavioral health care to people who are eligible for Medicaid or Medicare. These programs employ an interdisciplinary team of medical, mental health, behavioral and social service specialists who provide patients with care in their homes and/or at day treatment centers.
“We have a day health center where participants come to receive different types of activities, socialization and cognitive stimulation including pet therapy and bingo,” Burns said about On Lok Lifeways. “There’s also a clinic on site with three doctors and one nurse practitioner and several nurses. All of our participants are given a full physical exam before they are enrolled and they are evaluated every six months, or as health conditions occur. We also have a rehab team, which includes occupational therapists and physical therapists. We have a home care team of nurses and aides who provide people with showers, assist them with meals, provide medication reminders, and help them with chores and laundry in their home.”
Burns said social workers are an important part of PACE programs’ interdisciplinary team, serving as patient advocates and as the bridge of communication between patients and caregivers, and between different health providers and teams.
“Social workers are connected to all of the aforementioned teams. It is our job to connect our patients with the services that these teams provide, and to connect the teams with one another as necessary to ensure proper emotional, mental and physical care for our participants,” she said. “We also are the primary point of contact for our participants’ family members. Social workers at On Lok also play an important role in the initial assessment of patients, and in the development of their care plan.”
Social workers who work at PACE programs typically have similar work settings and responsibilities as social workers who work in geriatric departments of hospitals and medical centers. However, PACE programs provide more comprehensive services, combining medical, mental and behavioral health care, and serve clients who are eligible for Medicare or Medicaid. Therefore, social workers at such programs may connect with more organizations, provide a wider range of care coordination services and travel across different settings. For example, they may also conduct home visits, help patients and their families navigate the process of applying for medical benefits, and communicate with medical, mental health and behavioral, and social services departments within their program.
Specialized Senior Assistance Programs
Gerontological social workers may work for specialized programs that support senior citizens in a certain area of their life, such as financial literacy, community engagement, housing coordination and low-income support services. For example, social workers may work for a community service organization that serves low-income older adults and helps them find stable housing, health care or disability assistance, or they might work for an organization that provides financial advice, subsidized nutrition programs or home care services.
Some larger organizations, such as San Francisco’s Institute on Aging , fund a wide range of programs and conduct research on how society and local, state and federal governments may better support older populations. Social workers may work for these larger organizations, within one or more programs.
Hospices provide palliative and end-of-life care to people suffering from terminal illnesses or conditions. Gerontological social workers in hospice settings work with patients and their families, providing emotional support, grief and bereavement counseling, resource navigation and care coordination. Hospices typically provide patients with symptom and pain management (palliative care) and assistance in end-of-life planning. Hospice social workers engage in all the non-medical aspects of a patient’s care, including coordinating community resources, answering patients’ and family members’ questions, helping family members cope with the loss of a loved one, and assisting clients in managing their family and social relationships during their time in hospice care.
Nursing Homes and Residential Care Facilities
Nursing homes provide residential support to people who cannot live independently due to mental or physical conditions such as dementia or disability. The transition to a nursing home or a residential care facility may be psychologically, emotionally and financially challenging. Gerontological social workers in these settings help clients and their families during this transition and ensure they receive the services they require both during their admission and throughout their stay. They may also help develop and review nursing home policies and procedures to ensure that residents receive the care and attention they need.
Gerontological social work provides the opportunity to connect deeply with those in need who are often appreciative of the support, and who have a wealth of life experiences and perspectives to share. Serving as an advocate for clients who would not otherwise have a voice in their care may also be gratifying and empowering. In addition, this field of social work involves working with clients’ families and loved ones, which may form unique and rewarding connections.
“One of the most rewarding experiences are the long-term relationships I have with my participants and knowing that I am able to make a difference in their lives,” Burns said. “I find it very rewarding to build relationships with my participants and know that part of my treatment plan is to check in with them. I feel really blessed that I get paid to do this work, to connect and learn about people who have lived very interesting lives—very different, often, from the life that I have led.”
She also noted how her role as a geriatric social worker enables her to share more about herself with her patients, relative to other types of medical settings, which at times allows for deeper and more rewarding connections.
“I think one thing that I’ve noticed in geriatric social work is because I have such long-term relationships with people, I’m able to share a little bit more of myself,” she explained, “In hospitals you’re working with someone for a short amount of time, and you just need to focus on them, and they don’t get as much of an opportunity to also learn a little about you.”
In addition to her work at the Institute on Aging, Stiles worked as a medical social worker, bereavement coordinator, and bereavement and volunteer manager at Odyssey Healthcare, a hospice setting in which she served geriatric patients and their families. She said it has been very fulfilling to have a positive impact on patients’ well-being and relationships, and helping them preserve their comfort and dignity as they manage difficult health conditions.
“I have had so many rewarding experiences with clients—so many frail, dying individuals I’ve had the honor of working with and being present for, so many people I’ve been privileged to advocate for when they were not able to speak for themselves, so many grieving families I’ve been able to comfort and counsel,” she said. “It’s been really incredible how many clients have really touched me.”
Some of the primary challenges of gerontological social work include the complexity and severity of some clients’ challenges (which at times necessitate difficult conversations about end-of-life care and planning), instances of elder abuse or neglect, age-based discrimination, family conflicts that interfere with appropriate or sufficient care, and the challenges and limitations within the health care system that may prevent older patients from receiving the medical attention and resources they need.
Stiles said older clients can often face a combination of challenges, including prejudice against people who are aging, senior citizens’ changing occupational and/or financial status, and the physical and mental declines that tend to come with aging.
“Older adults face many of the same concerns and issues as any adult-limited resources, mental health issues, substance abuse, history of trauma, systemic racism, homophobia, classism, etc.,” she said. “What makes older adults ‘unique’ is that they are dealing with these concerns with the added pressure of ageism (discrimination against people based on their age) and ableism (discrimination against those with disabilities), as well as potential physical health changes and accumulated losses.”
Managing family members’ concerns—or their lack of concern—can also prove challenging. “While many families are wonderful to work with, other families are very difficult to work with,” Burns noted. “Families often are at one end or the other of the spectrum, very, very involved and high maintenance, and then there are other families that you call and call and cannot get them to call you back. It is important to have strong relationships and build trust with all families that you work with.”
Encountering systemic injustices that particularly hurt elders can also be a challenge that gerontological social workers encounter on the job. “Many of the challenges I’ve faced with clients are primarily due to longstanding, often untreated mental illness that clients have been dealing with for decades,” Stiles noted. “Often, there are systematic issues like generational poverty, lack of services in the community and a general lack of concern for older adults unless in a medicalized setting.”
To manage the challenges of the work, social workers suggested that students manage their expectations about what they are able to do to help clients, and appreciate their successes while learning from their mistakes.
“For new social workers, I recommend keeping perspective and understanding the limitations placed on people in this profession,” Stiles said. “Many issues an older client is dealing with are issues they’ve been dealing with for decades. We cannot solve family discord, we cannot solve poverty, we cannot solve regrets or mental illness or a lack of services. This is incredibly difficult and takes years of practice and self-reflection.”
Burns said she remains optimistic and turns the challenges she encounters into opportunities to connect with her clients and their families, and to better meet their needs and concerns. “It’s very rewarding when you are able to build trust with a family that is hard to reach or get them to agree to provide care that they have been resistant to provide,” she noted.
Find out how to become an LCSW today.
When should a geriatric social worker be consulted?
A geriatric social worker may be brought into a case if a patient has physical or emotional needs, conflicts or resistance, or unresolved safety concerns. Geratric social workers may also assist with discharge and follow-up after a hospital visit. They may even help make sure the details of patients’ end-of-life decisions are in order.
Why are geriatric social workers needed?
Geriatric social workers are a patient’s advocate and may help them receive the care they need. They distinguish between normal and abnormal aging and help connect clients to community resources available in the area. For example, a geriatric social worker refers older adults for home care services if safety oversight or assistance with personal care is needed.
How much do gerontology social workers make?
The median annual wage of social workers was $51,760 in 2020, the BLS reports. The BLS categorizes social workers who specialize in a geriatric setting as health care social workers. So, to find the average geriatric social worker salary, analyze BLS data for health care social workers. According to BLS data, the 2020 mean wage of health care social workers was $57,630.
What type of social worker gets paid the most?
According to 2020 annual mean wage data for social workers from the BLS , “social workers, all other” earn the most, an average of $63,670. Gerontological social workers may fit within healthcare social workers, who earn a median annual wage of $54,310. Here are the mean wages of other types of social workers, as reported by the BLS:
- Child, family and school social workers: $51,650
- Mental health and substance abuse social workers: $48,570
What is the difference between a geriatric social worker and other social workers?
All social workers are committed to the well-being of individuals, families and groups. Geriatric social workers focus on the health of older patients and those who are most vulnerable. They are specially trained in the issues commonly facing older people, including anxiety, dementia, depression, financial instability, isolation, and other emotional and social challenges. They are also trained in providing clients with access to other care and support programs they need.
Last updated: February 2022
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A Role for Social Workers in Improving Care Setting Transitions: A Case Study
Ruth d. barber.
Davis School of Gerontology, University of Southern California, Los Angeles, California, USA
ALEXIS COULOURIDES KOGAN
Anne riffenburgh.
Huntington Memorial Hospital, Pasadena, California, USA
SUSAN ENGUIDANOS
High 30-day readmission rates are a major burden to the American medical system. Much attention is on transitional care to decrease financial costs and improve patient outcomes. Social workers may be uniquely qualified to improve care transitions and have not previously been used in this role. We present a case study of an older, dually eligible Latina woman who received a social work–driven transition intervention that included in-home and telephone contacts. The patient was not readmitted during the six-month study period, mitigated her high pain levels, and engaged in social outings once again. These findings suggest the value of a social worker in a transitional care role.
INTRODUCTION
High rates of readmissions among American hospitals have an enormous impact on quality of life and costs of care of the American health care system ( Bjorvatn, 2013 ; Coleman, Parry, Chalmers, & Min, 2006 ; Hansen, Young, Hinami, Leung, & Williams, 2011 ; Hernandez et al., 2010 ; Williams, 2013 ). Thirty-day readmission rates are an accepted marker of discharge success and a reflection of quality of care ( Allaudeen, Vidyarthi, Maselli, & Auerbach, 2011 ; Bjorvatn, 2013 ; Jha, Orav, & Epstein, 2009 ; Vashi et al., 2013 ). It appears that American hospitals are not performing as well as desired: it is estimated that 20–25% of Medicare beneficiaries are readmitted within 30 days of hospital discharge and that these readmissions cost $26 billion annually ( Allaudeen, Schnipper, Oray, Wachter, & Vidyarthi, 2011 ; Centers for Medicare and Medicaid Services, 2012 ; Graham, Leff, & Arbaje, 2013 ; Hansen et al., 2011 ; Hernandez et al., 2010 ; Jencks, Williams, & Coleman, 2009 ; Voss et al., 2011 ). This amount accounts for 17–24% of overall Medicare hospital expenditures, ( Jencks et al., 2009 ), which is especially concerning considering that 75% of readmissions are thought to be avoidable ( Hansen et al., 2011 ).
Poor transitions that lack care continuity have been found to lead to adverse outcomes and greater risk of readmission, especially for older adults ( Arbaje et al., 2008 ; Coleman, Parry, Chalmers, & Min, 2006 ; Jencks et al., 2009 ). In fact, the Institute of Medicine has explicitly identified transitional care as a high-priority area for performance measurement ( Institute of Medicine Staff, 2006 ). Recent studies have found that lack of primary care follow-up within seven days of discharge increases risk of 30-day readmission tenfold ( Hernandez et al., 2010 ; Takahashi et al., 2013 ). Other issues at discharge include lack of communication with the primary care physician (PCP) at discharge, a decreasing number of available PCPs ( Williams, 2013 ), inadequate or nonexistent medication reconciliation ( Boling, 2009 ), incomplete or inaccurate information transfer to the next provider ( Boling, 2009 ; Williams, 2013 ), and patient non-compliance with prescribed medications ( Boling, 2009 ). These issues can lead to inadequate patient and caregiver preparation for quality care at the next health location ( Coleman et al., 2004 ; Coleman, Parry, Chalmers, Chugh, & Mahoney, 2007 ) lack of preparation for self-management role, lack of access to a health care practitioner to address direct concerns, and minimal input in patient care plans ( Institute of Medicine Staff, 2006 ). Additionally, multiple transitions that lead to readmissions are common. It is estimated that over 30% of patients undergo more than one post-hospital transfer after discharge ( Coleman, Min, Chomiak, & Kramer, 2004 ) and one out of seven patients discharged from hospitals have four to six transitions within three months, increasing the potential for mismanagement ( Boling, 2009 ; Coleman et al. 2006 ; Hernandez et al., 2010 ; Kocher & Adashi, 2011 ). These shortcomings ultimately lead to greater use of hospital and emergency services ( Coleman et al. 2004 , 2006 ). As a result, national attention has been given to streamlining and improving care coordination during the discharge process to reduce avoidable readmissions, especially since the mere documentation of providing discharge instructions to patients has failed to significantly reduce readmission ( Allaudeen et al., 2011 ; Hernandez et al., 2010 ; Jha et al., 2009 ).
Prior to the Affordable Care Act (ACA) ( Patient Protection and Affordable Care Act, 2010 ), the fee-for-service system provided hospitals incentive for a short hospital stay, without penalty for unfavorable outcomes, such as high readmission or mortality rates ( Bueno et al., 2010 ; Johnson & McCarthy, 2013 ; Kamerow, 2013 ). For common diseases like chronic heart failure, readmission rates increased, yet mean length of stay in hospital decreased by 26% ( Bjorvatn, 2013 ; Bueno et al., 2010 ). Discharge disposition also changed significantly in recent years, with a 53% relative increase in proportion of discharges to skilled nursing facilities (SNFs) and a 10% reduction in discharges to home ( Bueno et al., 2010 ). Among those discharged to home, greater percentages of patients are unstable, making post-discharge home care an important target for improvement ( Kosecoff et al., 1990 ).
Now, due to the ACA, incentives for reducing readmission have changed. Hospitals are being penalized for excessive readmissions, defined as the ratio of a hospital’s readmission performance compared with the national average for the set of patients with an applicable condition, among other criteria ( Allaudeen et al., 2011 ; Fontanarosa & McNutt, 2013 ; Lacker, 2011 ). Penalties for readmissions are currently incurred among patients diagnosed with acute myocardial infarction, heart failure, and pneumonia, with more conditions to be added in 2015 ( Kocher & Adashi, 2011 ). Penalties currently entail a 2% reduction in Medicare Inpatient Prospective Payment System reimbursements for all expenses during readmissions for pneumonia, acute myocardial infarction, and heart failure. This figure will increase to 3% in 2015 and is expected to also include chronic obstructive pulmonary disease, coronary artery bypass graft surgery, percutaneous coronary interventions, and other vascular procedures. These penalties cost hospitals—and save Medicare—an estimated $300 million per year ( Fontanarosa & McNutt, 2013 ; Jencks et al., 2009 ; Kamerow, 2013 ).
The need to reduce hospital readmission among older adults has never been more pressing. The national population of adults over 65 years old is projected to rise from 14% to 20% by 2030, and then peak at 25% by 2050. Additionally, adults over 85 are expected to increase by 400% by 2050, and their cost of care has been found to be eight times that of the average adult ( Allaudeen et al., 2011 ; Bjorvatn, 2013 ; Hackstaff, 2009 ). This puts quite a burden on an already indebted health care system, which is projected to cost 30% of Gross Domestic Product (GDP) by 2035 and 50% by 2085 ( Hackstaff, 2009 ). In addition to reduced health care costs, improved transitions from hospital to home will result in better quality of life for patients and better health outcomes for the general public ( Allaudeen et al., 2011 ). Low-cost interventions focused on education, medication management, and peer support have demonstrated reductions in 30-day hospitalizations ( Boling, 2009 ; Brock et al., 2013 ; Coleman et al., 2004 ; Jack et al., 2009 ). Interventions, especially those that utilize “transition coaches” that guide patients toward activation and self-care, have a significant association to reductions in rehospitalizations and emergency department visits for at least six months following discharge ( Brock et al., 2013 ; Coleman et al., 2004 ; Dharmarajan et al., 2013 ; Johnson & McCarthy, 2013 ; McCarthy et al., 2013 ) A recent review of 14 hospital-to-home transition interventions showed a mean reduction of 5.7% in rehospitalizations ( Brock et al., 2013 ). Interdisciplinary interventions have also resulted in fewer emergency departments visits and better health outcomes ( Brock et al., 2013 ; Johnson & McCarthy, 2013 ). Interventions that provide home-visits also have shown significant positive effects on mortality, admission, readmission, and nursing home placements ( Elkan et al., 2001 ). Discharge planners and home health services that focus on the home transition are now positioned to play a more active role in care transitions, due to their simplicity and relatively low cost of implementation ( Coleman et al., 2004 ).
Social workers, in contrast to more medically focused nurses or advanced practice nurses, are potentially better suited to fill an intervention role within hospitals ( Health Resources and Services Administration, 2004 ) since they are trained to link patients with community and home-based services, reduce fragmented health and social service systems, and address both the medical and psychosocial needs of the patient ( Atkinson & Nelson, 1995 ; Coley, Williams, DaPos, Chen, & Smith, 2002 ; Geron, Andrews, & Kuhn, 2005 ; Rosen & Teeson, 2001 ; Scharlach, Simon, & Dal Santo, 2002 ; Vourlekis, Gelfand, & Greene, 1992 ). This is especially important considering that 40–50% of hospital readmissions are linked to psychosocial problems and lack of community resources and that 80% of older adults experience unaddressed social needs post-discharge ( Altfeld, Pavle, Rosenberg, & Shure, 2012–2013 ). Social workers focus on incorporating both the patients’ and caregivers’ needs along with the needs of institutions or social services to provide an optimal care plan, according to the ecological model ( Fabbre, Buffington, Altfeld, Shier, & Golden, 2011 ). Also, the social worker’s emphasis on both tangible support, like connecting patients with resources, and emotional support, like reflective listening or giving encouragement, is important for better health outcomes for older adults ( Fabbre et al., 2011 ; Parry, Mahoney, Chalmers, & Coleman, 2008 ). Thus, social work–driven interventions—social workers facilitating access to multidisciplinary care and interventions—may potentially reduce readmission rates and medical service use, as well as facilitate linkage to community-based social services to increase the quality of transitional care. Yet little is known about the social work role in improving care transitions.
We present a case study of a social work–driven care transitions intervention. This case study provides insight into how a social worker can potentially improve the transition experience and health outcomes for at-risk older adults.
A single-case, case study methodology was used to investigate the social work role in providing care transition support for an at-risk older adult. Case studies provide an opportunity for in-depth investigation of a phenomenon to develop a greater understanding within a real-world context ( Yin, 1989 ). Case studies also represent the preliminary stage of research, spark interest, and suggest possibilities for deeper and more detailed investigation of novel concepts in the future ( Rowley, 2002 ). This case provides insights into the specific social work tasks that may support older adults transitioning from hospital to home.
Subject Eligibility and Recruitment
The case was selected from a larger study of a social work intervention. Participants were recruited from a large, non-profit, urban community hospital in Los Angeles County. Eligibility criteria included adults aged 65 years or more, currently hospitalized, cognitively intact (five or more correct on Short Portable Mental Status Questionnaire), English-speaking, residing within a study-designated geographical area, and identified as at high risk for readmission. High risk was determined by meeting at least one of the following criteria: aged 75 or older, prescribed five or more medications, or having one or more hospitalization or emergency department visit in the previous six months. Patients were screened and consented at bedside.
Social Work Intervention Focused on Transitions (SWIFT) Intervention
Those assigned to the SWIFT intervention group received transition care that included a home safety review, psychosocial assessment, medication reconciliation, review of discharge orders, and assistance with scheduling follow-up appointments with the primary care physician and/or specialists, as needed. In addition, they received the following assessments: home safety, depression, and self-management of chronic conditions needs. The goals of the intervention were to ensure comprehension and adherence to discharge instructions, ensure medication accuracy and compliance, ensure physician follow-up within 10 days of discharge, and assess the patient’s ability to manage chronic conditions.
The intervention also employed problem-solving therapy (PST) ( Nezu, 2004 ) to assist the patient with prioritizing needs and identifying possible solutions. The aim of PST is not to solve problems for the patient; rather, to teach patients to address their problems and challenges by breaking them down into smaller goals and identifying actions that can be taken to solve them, with the ultimate goal of providing long-term and sustainable self-sufficiency ( Enguidanos, Coulourides Kogan, Keefe, Geron, & Katz, 2011 ; Malouff, Thorsteinsson, & Schutte, 2007 ; Nezu, 2004 ). The social worker worked with the patient to identify problems or issues and to develop a plan to address them.
Those assigned to the SWIFT group received an in-home assessment (at least one visit conducted within 48-hours of discharge and a maximum of two visits to address unresolved issues identified during the first home visit, as determined by the social worker) and telephone follow-up (up to a maximum of four phone contacts).
Data Measures
Social worker chart notes, baseline documents taken in-hospital by a clinical research assistant, and all assessments completed over the phone and during home visits were sources of data for this study.
Demographics
Patient demographics and other characteristics including age, gender, marital status, and presence of advance directive were collected from patient surveys conducted at bedside.
Medications
A complete medication review was completed based on the Medication Management Improvement System program that focuses on medication duplication and psychotropic effects associated with falls and confusion ( Alkema, Wilber, Frey, Enguidanos, & Simmons, 2008 ). Current medications were entered into the Medications Management Improvement System database ( Partners in Care Foundation, 2013 ) and electronically screened for errors and potential problems using the home health criteria developed by a panel of experts ( Meredith et al., 2001 ). Any problems were reported to the primary care physician and discussed with the patient.

Social Service Needs
A Home Safety Evaluation developed by the University of Southern California’s Falls Prevention Center was used to assess the risk of falls at home ( Fall Prevention Center of Excellence, 2014 ) The Lorig Chronic Care Self Management scale ( Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001 ) was used to assess the patient’s ability to manage his chronic conditions by monitoring symptom control, physician communication, and role function.
Numeric rating scale (0–10), where zero indicates no pain and 10 corresponds to the worst pain imaginable.
Service Utilization
Self-reported health service use was measured at six months following study enrollment. These self-reports were confirmed via electronic medical rewards at the clinical study site.
Case Description
Mrs. S was a 90-year-old widowed Latina woman with a second-grade education level. She resided with her granddaughter, who was her primary caregiver, and had both Medicare and Medicaid health care insurance. At the time of her index hospitalization, she was taking seven prescription medications for six health conditions and had been admitted for nausea and gastrointestinal bleeding via the hospital emergency department. Her chronic conditions included hypertension, asthma, arthritis, anemia, diabetes, and heart disease. She also reported a high pain level (10/10), since her prescribed pain medication had limited effect. The patient reported minimal depression with a score of 3 on the PHQ-9 Depression Scale, and reported moderate physical limitations in lifting and carrying groceries and climbing stairs. The patient ambulated with a cane, had no fear of falling, and had transportation to medical appointments from her granddaughter.
First Home Visit
During the SWIFT home assessment (first study contact), the patient reported a continued high level of pain (8/10) and had partially filled prescriptions following her hospital visit, including Tramadol, Metroprolol Tartrate, and Q-pap for pain. As part of the intervention, the social worker conducted a medication reconciliation using the HomeMeds medication software program. She found the medication regimen was clear of duplication, interactions, and medications contraindicated for older adults. The social worker also conducted a home safety check resulting in recommendation for installation of grab bars in her bathroom. The patient’s greatest concern was her intractable pain resulting from arthritis and other health conditions. Using a problem-solving approach, Mrs. S, her granddaughter (caregiver), and the social worker worked together to identify ways to better manage her pain. Mrs. S established goals including getting a heating pad to ease discomfort and making a follow-up appointment with her primary care physician to obtain improved pain management interventions.
Second Home Visit
Due to the extreme pain experienced by Mrs. S, the social worker made a second home visit four days later. During this visit, the social worker discovered that Mrs. S had not scheduled her follow-up physician appointment and continued to experience sustained high levels of pain. Additionally, her existing pain medication was running low and the doctor’s office was closed, preventing Mrs. S from obtaining a refill. With the help of the social worker, Mrs. S set goals to immediately schedule a physician visit, request that her physician provide improved pain management, and coordinate with her physical therapist to get a hospital bed for increased comfort at home.
Telephone follow-up #1
The social worker conducted a follow-up by phone four days after her second home visit with Mrs. S. The patient reported that she had made and attended an appointment with her primary care physician; however, the visit had focused on her anemia diagnosis, and her pain issues were not discussed or addressed. As a result, Mrs. S continued to experience high levels of pain and only had a few pain pills remaining. The social worker attempted to contact the physician’s office directly; however, the physician’s office was closed for a three-day holiday weekend. The patient agreed to call the physician after the holiday to request Tylenol 500 (Acetominophen 500 mg), a pain medication that had previously proven effective in alleviating her pain, or another alternative prescription medication to control her pain.
Telephone follow-up #2
Twelve days following hospital discharge and three days following the previous telephone call, the social worker conducted a second follow-up telephone call (fourth contact overall). Mrs. S reported that she had received a prescription for Tylenol 500 to treat her pain. However, her pain level remained high at 7 on a scale from 0 (no pain) to 10 (worst pain possible). The social worker subsequently contacted Mrs. S’s granddaughter, who expressed a desire to switch Mrs. S’s physician to one more responsive to her pain management needs.
Telephone follow-up #3
Three days later, the social worker conducted a third follow-up call and discovered that Mrs. S felt continued high levels of pain, but had scheduled an appointment with a new physician. The social worker coached the granddaughter on how to strongly advocate on her grandmother’s behalf and advised the family to contact both the previous and current physician regarding pain management to receive the most prompt pain management possible. Additionally, Mrs. S’s eligibility for both Medicaid and Medicare along with her physical functioning challenges qualified her for a Medicaid-waiver program for ongoing case management. The social worker placed her on the wait list to ensure ongoing access to needed social services and case management.
Telephone follow-up #4
On the 26th day after her discharge from the hospital, Mrs. S received her fourth and final telephone contact from the SWIFT social worker (a summary of all contacts can be seen in Table 1 ). The social worker learned that the family successfully advocated with the original primary care physician to obtain stronger pain medications. Additionally, the hospital bed was delivered, and Mrs. S stated she was feeling more comfortable at home. Mrs. S also reported increased socialization, significant reduction in pain, and subsequent ability to resume basic functions and simple errands, such as grocery shopping. Significantly, the patient was not readmitted to either the emergency department or the hospital in the six months following her hospital discharge.
Summary of all Home and Telephone Contacts
| Contact Number | Day | Type | Medication management | Discharge Planning | Psychosocial Assessment | Patient Training | Follow-Up Referrals | Result | Action Items |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | Home Visit | X | X | X | X | X | Home assessment, medication reconciliation, problem-solving pain management | Schedule a physician visit for pain |
| 2 | 5 | Home Visit | X | X | X | X | Increased pain, Mrs. S had not scheduled physician appointment yet, low on pain meds | Schedule physician visit ASAP, ask for pain medication prescription, get hospital bed | |
| 3 | 9 | Phone | X | X | X | Mrs. S had seen physician, but not received pain meds | Call physician to ask about alternative to prescription pain medication | ||
| 4 | 12 | Phone | X | X | Taking Tylenol, but high pain; wanted to switch physicians | Call new physician | |||
| 5 | 15 | Phone | X | X | X | Reported increased pain, but had scheduled appointment | Contact both physician re: pain management; put on wait-list for case manager | ||
| 6 | 26 | Phone | X | Received hospital bed, received pain medication | – |
Case Analysis
Our case study highlights potential patient needs during transition from hospital to home and the role of a social worker in improving care and maximizing health outcomes. The social worker focused on traditional transition issues, such as ensuring follow-up with primary care physician and performing medication reconciliation, and also worked with Mrs. S to identify and address other health-related needs, such as improved pain management and increased access to supportive services.
The social worker provided important coaching that enabled Mrs. S’s granddaughter to effectively negotiate improved pain management with the primary care physician. This coaching was perhaps one of the most essential aspects of this case study: coaching in negotiation skills can give patients self-control and self-efficacy and reduce feelings of helplessness or victimization, leading to better health outcomes ( Choi, Marti, Bruce, & Hegel, 2013 ). Interventions like SWIFT that encourage person-centered self-advocacy, self-management, and problem solving ( Coleman et al. 2006 ; Naylor et al., 1999 ) leads to long-lasting benefits that have proven to reduce rehospitalization, reduce health costs, and improve patient and provider satisfaction ( Arbaje et al., 2008 ; Boling, 2009 ; Enguidanos et al., 2011 ; Naylor et al., 1999 ; Voss et al., 2011 ). Mrs. S had numerous factors that placed her at high risk for readmission including her ethnicity ( Joynt, Orav, & Jha, 2011 ; McHugh, Carthon, & Kang, 2010 ); advanced age ( Bjorvatn, 2013 ; Goldfield et al., 2008 ; Krumholz et al., 1997 ; Silverstein, Qin, Mercer, Fong, & Haydar, 2008 ); limited education ( Arbaje et al., 2008 ); Medicare and Medicaid status ( Coleman et al., 2004 ; Hasan et al., 2009 ); single (widowed) marital status ( Arbaje et al., 2008 ; Garrison, Mansukhani, & Bohn, 2013 ); and multiple chronic conditions including hypertension, diabetes, and arthritis that caused her to experience severe pain ( Bjorvatn, 2013 ; Coleman et al., 2004 ; Silverstein et al., 2008 ). In particular, studies have suggested that pain may worsen executive functions that lead to decreased compliance in older adults ( Karp et al., 2006 ). With coaching and an emphasis on social solutions to positively impact physical conditions, Mrs. S’s pain was reduced, and she was not subsequently readmitted to the hospital during the six months following initial hospital discharge. The patient also received referrals to community-based resources, such as a Medicaid-waiver program.
IMPLICATIONS
This study provides a detailed case study of a patient enrolled in a social work-driven intervention to improve transition from hospital to home.
The National Association for Social Workers ( Herman, 2009 ) identifies key social work values and practice standards that bring strength to their role in transitional care for older adults. These include their focus on person-centered care, the ecological framework that includes assessment of personal and environmental factors, and their practice approach that includes collaboration with informal and formal caregivers and providers. Additionally, social workers often have more experience in geriatrics and community-based practice and may better address social-service issues (e.g., lack of access to community services like transportation or social support services) than a medical-based intervention ( Altfeld et al., 2012 ). Social workers are knowledgeable in successfully utilizing mechanisms to overcome disciplinary boundaries, such as the electronic medication system used in this study ( Fabbre et al., 2011 ). They are also trained to relieve caregiver burden, to help patients cope with changes in health status, and to connect patients with services ordered at discharge, which is oftentimes a challenge ( Altfeld et al., 2012 ).
Rush University developed and tested another social work driven transition intervention. The Bridge Model ( Altfeld et al., 2012 ; Fabbre et al., 2011 ) provided social work transition care beginning at bedside in the hospital and arranged services prior to hospital discharge. Telephone follow-up was provided two days post-discharge to identify new problems, to determine patient understanding of discharge instructions and medication regimens, and to schedule follow-up medical appointments. Although not effective in reducing 30-day readmissions, perhaps due to the lack of intense intervention post-discharge and the reliance on telephone follow-up, The Bridge Model was effective in increasing access to follow-up care and services ( Altfeld et al., 2012 ).
A traditional nurse-driven transition intervention providing purely medical follow-up may fail to address psychosocial problems and thus does not fully empower patients and caregivers to improve their health. Moreover, it is crucial that interventions address both psychosocial and health issues, linking patients to community resources as well as collaborating with the health care team ( Altfeld et al., 2012 ). Including social workers in transitional care interventions may provide improved linkages to health care and community-based services as well as greater psychosocial support that lead to sustainable positive health outcomes. Indeed, studies have shown increased social work support services are associated with lower total hospital costs and increased probability of physician follow-up after discharge ( Altfeld et al., 2012–2013 ; Hine, Howell, & Yonkers, 2008 ; Rizzo, 2006 ). Our case study provides a concrete example of how social workers can empower patients to improve their health status and provide critical linkages to health providers, community-based resources, and services that will provide ongoing support for community-dwelling older adults.
Contributor Information
RUTH D. BARBER, Davis School of Gerontology, University of Southern California, Los Angeles, California, USA.
ALEXIS COULOURIDES KOGAN, Davis School of Gerontology, University of Southern California, Los Angeles, California, USA.
ANNE RIFFENBURGH, Huntington Memorial Hospital, Pasadena, California, USA.
SUSAN ENGUIDANOS, Davis School of Gerontology, University of Southern California, Los Angeles, California, USA.
- Alkema GE, Wilber KH, Frey D, Enguidanos SM, Simmons WJ. Characteristics associated with four potential medication problems among older adults in Medicaid waiver services. The Consultant Pharmacist. 2008; 23 (5):396–403. [ PubMed ] [ Google Scholar ]
- Allaudeen N, Schnipper JL, Oray EJ, Wachter RM, Vidyarthi AR. Inability of providers to predict unplanned readmissions. Journal of General Internal Medicine. 2011; 26 (7):771–776. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Allaudeen N, Vidyarthi A, Maselli J, Auerbach A. Redefining readmission risk factors for general medicine patients. Journal of Hospital Medicine. 2011; 6 :54–60. [ PubMed ] [ Google Scholar ]
- Altfeld SJ, Shier GE, Rooney M, Johnson TJ, Golden RL, Karavolos K, Perry AJ, et al. Effects of an enhanced discharge planning intervention for hospitalized older adults: A randomized trial. The Gerontologist. 2012; 53 (3):430–440. [ PubMed ] [ Google Scholar ]
- Altfeld S, Pavle K, Rosenberg W, Shure I. Integrating care across settings: The Illinois transitional care consortium’s bridge model. Journal of the American Society on Aging. 2012–2013 Winter; 36 (4):98–101. [ Google Scholar ]
- Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. The Gerontologist. 2008; 48 (4):495–504. [ PubMed ] [ Google Scholar ]
- Atkinson V, Nelson G. Adult protective services. In: Nelson G, Eller A, Streets D, Morse M, editors. The Field of Adult Services: Social Work Practice and Administration. Washington, DC: NASW Press; 1995. pp. 215–230. [ Google Scholar ]
- Bjorvatn A. Hospital readmission among the elderly. European Journal of Health Economics. 2013; 14 :809–820. [ PubMed ] [ Google Scholar ]
- Boling PA. Care transitions and home health care. Clinics in Geriatric Medicine. 2009; 25 (1):135–148. [ PubMed ] [ Google Scholar ]
- Brock J, Mitchell J, Irby K, Stevens B, Archibald T, Goroski A, Lynn J. Association between quality improvement for care transitions in communities and rehospitalizations among Medicare beneficiaries. JAMA. 2013; 309 (4):381–391. [ PubMed ] [ Google Scholar ]
- Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, Normand ST, Krumholz HM, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993–2006. JAMA. 2010; 303 (21):2141–2147. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centers for Medicare and Medicaid Services. Community-based care transitions program. 2012 Retrieved from http://innovation.cms.gov/initiatives/CCTP/?itemID=CMS1239313 .
- Choi NG, Marti CN, Bruce ML, Hegel MT. Depression in homebound older adults: Problem-solving therapy and personal and social resourcefulness. Behavior Therapy. 2013; 44 :489–500. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Coleman EA, Parry C, Chalmers S, Min S. The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine. 2006; 166 (17):1822–1828. [ PubMed ] [ Google Scholar ]
- Coleman EA, Min S, Chomiak A, Kramer AM. Posthospital care transitions: Patterns, complications, and risk identification. Health Services Research. 2004; 39 (5):1449–1466. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Coleman EA, Parry C, Chalmers SA, Chugh A, Mahoney E. The central role of performance measurement in improving the quality of transitional care. Home Health Care Services Quarterly. 2007; 26 (4):93–104. [ PubMed ] [ Google Scholar ]
- Coleman EA, Smith JD, Frank JC, Min S, Parry C, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: The care transitions intervention. Journal of the American Geriatrics Society. 2004; 52 (11):1817–1825. [ PubMed ] [ Google Scholar ]
- Coley KC, Williams BA, DaPos SV, Chen C, Smith RB. Retrospective evaluation of unanticipated admissions and readmissions after same day surgery and associated costs. Journal of Clinical Anesthesia. 2002; 14 (5):349–353. [ PubMed ] [ Google Scholar ]
- Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Krumholz HM, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. Journal of American Medical Association. 2013; 309 (4):355–363. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, Brummell K, et al. Effectiveness of home based support for older people: Systematic review and meta-analysis. British Medical Journal. 2001; 323 :1–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Enguidanos S, Coulourides Kogan A, Keefe B, Geron SM, Katz L. Patient-centered approach to building problem solving skills among older primary care patients: Problems identified and resolved. Journal of Gerontological Social Work. 2011; 54 :276–291. [ PubMed ] [ Google Scholar ]
- Fabbre VD, Buffington AS, Altfeld SJ, Shier GE, Golden RL. Social work and transitions of care: Observations from an intervention for older adults. Journal of Gerontological Social Work. 2011; 54 (6):615–626. [ PubMed ] [ Google Scholar ]
- Fall Prevention Center of Excellence. Information for researchers and educators. 2014 Retrieved from http://stopfalls.org/wp-content/uploads/2013/09/ProgramExpansion-HomeAssessmentTool1.pdf .
- Fontanarosa PB, McNutt RA. Revisiting hospital readmissions. Journal of American Medical Association. 2013; 309 (4):398–400. [ PubMed ] [ Google Scholar ]
- Garrison GM, Mansukhani MP, Bohn B. Predictors of thirty-day readmission among hospitalized family medicine patients. Journal of the American Board of Family Medicine. 2013; 26 (1):71–77. [ PubMed ] [ Google Scholar ]
- Geron S, Andrews C, Kuhn K. Infusing aging skills into the social work practice community: A new look at strategies for continuing professional education. Families in Society: The Journal of Contemporary Social Services. 2005; 86 (3):431–440. [ Google Scholar ]
- Goldfield NI, McCullough EC, Hughes JS, Tang AM, Eastman B, Rawlins LK, Averill RF. Identifying potentially preventable readmissions. Health Care Financing Review. 2008; 30 (1):75–91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Graham LE, Leff B, Arbaje AI. Risk of hospital readmission for older adults discharged on friday. Journal of the American Geriatrics Society. 2013; 61 (2):300–301. [ PubMed ] [ Google Scholar ]
- Hackstaff L. Factors associated with frailty in chronically ill older adults. Social Work in Health Care. 2009; 48 (8):798–811. [ PubMed ] [ Google Scholar ]
- Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: A systematic review. Annals of Internal Medicine. 2011; 155 (8):520–528. [ PubMed ] [ Google Scholar ]
- Hasan O, Schnipper JL, Meltzer DO, Shaykevich SA, Bell CM, Kaboli PJ, Zhang J, et al. Hospital readmission in general medicine patients: A prediction model. Journal of General Internal Medicine. 2009; 25 (3):211–219. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Herman C. Social work and transitions of care. National Association of Social Workers, 1–4. 2009 Retrieved from http://www.socialworkers.org/practice/aging/2009/Social%20Work%20and%20Transitions%20of%20Care.pdf .
- Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Curtis LH, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010; 303 (17):1716–1722. [ PubMed ] [ Google Scholar ]
- Hine CE, Howell HB, Yonkers KA. Integration of medical and psychological treatment within the primary health care setting. Social Work in Health Care. 2008; 47 (2):122–134. [ PubMed ] [ Google Scholar ]
- Health Resources and Services Administration. Preliminary Findings 2004 National Sample Survey of Registered Nurses. Washington, DC: Author; 2004. [ Google Scholar ]
- Institute of Medicine. Committee on Redesigning Health Insurance Performance Measures, Payment, and Performance Improvement Programs; Board on Health Care Services. Washington, DC: National Academies Press; 2006. Performance measurement: Accelerating improvement. Retrieved from http://www.nap.edu/catalog/11517.html . [ Google Scholar ]
- Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Culpepper L, et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Annals of Internal Medicine. 2009; 150 (3):178–187. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England Journal of Medicine. 2009; 360 (14):1418–1428. [ PubMed ] [ Google Scholar ]
- Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. The New England Journal of Medicine. 2009; 361 (27):2637–2645. [ PubMed ] [ Google Scholar ]
- Johnson MB, McCarthy D. The visiting nurse service of New York’s choice health plans: Continuous care management for dually eligible Medicare and Medicaid beneficiaries. The Commonwealth Fund. 2013; 6 :1–16. [ Google Scholar ]
- Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011; 305 (7):675–681. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kamerow D. Reassessing hospital readmission penalties. BMJ. 2013 http://dx.doi.org/10.1136/bmj.f1043 . [ PubMed ]
- Karp JF, Reynolds CF, III, Butters MA, Dew MA, Mazumdar S, Begley AE, Weiner DK, et al. The relationship between pain and mental flexibility in older adult pain clinic patients. Pain Medicine. 2006; 7 (5):444–452. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kocher RP, Adashi EY. Hospital readmissions and the affordable care act: Paying for coordinated quality care. JAMA. 2011; 306 (16):1794–1795. [ PubMed ] [ Google Scholar ]
- Kosecoff J, Kahn KL, Rogers WH, Reinisch EJ, Sherwood MJ, Rubenstein LV, Brook RH, et al. Prospective payment system and impairment at discharge: The “quicker-and-sicker” story revisited. JAMA. 1990; 264 (15):1980–1983. [ PubMed ] [ Google Scholar ]
- Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Radford MJ, Hennen J. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Archives of Internal Medicine. 1997; 157 (1):99–104. [ PubMed ] [ Google Scholar ]
- Lacker C. Decreasing 30-day readmission rates. The American Journal of Nursing. 2011; 111 (11):65–69. [ PubMed ] [ Google Scholar ]
- Lorig KR, Sobel DS, Ritter PL, Laurent DD, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice. 2001; 4 (6):256–262. [ PubMed ] [ Google Scholar ]
- Malouff JM, Thorsteinsson EB, Schutte NS. The efficacy of problem solving therapy in reducing mental and physical health problems: A meta-analysis. Clinical Psychology Review. 2007; 27 :46–57. [ PubMed ] [ Google Scholar ]
- McCarthy D, Johnson M, Audet A. Recasting readmissions by placing the hospital role in community context. JAMA. 2013; 309 (4):351–352. [ PubMed ] [ Google Scholar ]
- McHugh MD, Carthon JMB, Kang XL. Medicare readmissions policies and racial and ethnic health disparities: A cautionary tale. Policy, Politics, & Nursing Practice. 2010; 11 (4):309–316. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meredith S, Feldman P, Frey D, Hall K, Arnold K, Brown N, Ray WA. Possible medication errors in home healthcare patients. Journal of the American Geriatric Society. 2001; 49 (6):719–724. [ PubMed ] [ Google Scholar ]
- Naylor MD, Brooten D, Campbell R, Jacobsen BS, Mezey MD, Pauly MV, Schwartz JS. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA. 1999; 281 (7):613–620. [ PubMed ] [ Google Scholar ]
- Nezu AM. Problem solving and behavior therapy revisited. Behavioral Therapy. 2004; 35 :1–33. [ Google Scholar ]
- Parry C, Mahoney E, Chalmers SA, Coleman EA. Assessing the quality of transitional care: Further applications of the care transitions measure. Medical Care. 2008; 46 (3):317–322. [ PubMed ] [ Google Scholar ]
- Partners in Care Foundation. Community-based medications management. 2013 Retrieved from https://www.picf.org/landing_pages/23,3.html ; https://homemeds.homemeds.org/
- Patient Protection and Affordable Care Act, 42 USC § 18001 et seq. 2010 [ Google Scholar ]
- Rizzo VM. Social work support services for stroke patients. Social Work in Health Care. 2006; 43 (1):33–56. [ PubMed ] [ Google Scholar ]
- Rosen A, Teeson M. Does case management work? The evidence and the abuse of evidence-based medicine. The Australian and New Zealand Journal of Psychiatry. 2001; 35 (6):731–746. [ PubMed ] [ Google Scholar ]
- Rowley J. Using case studies in research. Management Research News. 2002; 25 (1):16–27. [ Google Scholar ]
- Scharlach A, Simon J, Dal Santo T. Aging of California’s Baby Boomers: Implications for State Policies, Programs, and Personnel (CPRC Report) Berkeley, CA: Center for Advanced Services; 2002. [ Google Scholar ]
- Silverstein MD, Qin H, Mercer SQ, Fong J, Haydar Z. Risk factors for 30-day hospital readmission in patients ≥65 years of age. Proceedings (Baylor University Medical Center) 2008; 21 (4):363–372. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Takahashi PY, Haas LR, Quigg SM, Croghan IT, Naessens JM, Shah ND, Hanson GJ. 30-day hospital readmission of older adults using care transitions after hospitalization: A pilot prospective cohort study. Clinical Interventions in Aging. 2013; 8 :729–736. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vashi AA, Fox JP, Carr BG, D’Onofrio G, Pines JM, Ross JS, Gross CP. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013; 309 (4):364–371. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Voss R, Gardner R, Baier R, Butterfield K, Lehrman S, Gravenstein S. The care transitions intervention: Translating from efficacy to effectiveness. Archives of Internal Medicine. 2011; 171 (14):1232–1237. [ PubMed ] [ Google Scholar ]
- Vourlekis BS, Gelfand DE, Greene RR. Psychosocial needs and care in nursing homes: Comparison of views of social workers and home administrators. Gerontologist. 1992; 32 (1):113–119. [ PubMed ] [ Google Scholar ]
- Williams MV. A requirement to reduce readmissions: Take care of the patient, not just the disease. JAMA. 2013; 309 (4):394–396. [ PubMed ] [ Google Scholar ]
- Yin RK. Case Study Research: Design and Methods. Newbury Park, CA: Sage; 1989. [ Google Scholar ]

Aging in Place and Urban Social Work: A Case Study of a NORC
By: Man Wai Alice Lun, PhD
Currently, there are about 47 million people aged 60 and over in the U.S., which comprises 16.6 percent of the total population. It is believed this number will increase drastically as baby boomers age. As is the case nationally, in New York City there were about 1.3 million (16.1%) aged 60 and over of the city’s total population in 2005. Indeed, the older population of New York City has been increasing at a steady rate of 2.6%, from 1,252,206 in 2000 to 1,284,946 in 2005, according to the New York City Department for the Aging.
Looking at the racial distribution of the older population in New York City, statistics show that older whites as a group have slightly decreased at the rate of 20% between the 1990 and 2000 census data sets, whereas all other racial groups as a whole have increased 31.8% (NYCDFTA, 2003). A racial transition is happening in New York City, with all older racial minority groups growing in all five boroughs, concurrent with a decreasing older white population. New York City is like other urban areas nationwide in facing a rapidly growing aging population.
The majority of older people are dwelling in communities and neighborhoods (cited by Hooyman and Kiyak, 2008, p. 444). Providing home- and community-based health and social services to large groups, also known as “cluster care,” is believed to be a more cost-effective way, as compared with medical nursing homes, in long term care policy. It is necessary to explore whether the present urban area social service systems are able to provide health and social services to meet the needs of an older old population and whether these services are culturally competent.
Aging in Place and Naturally Occurring Retirement Community (NORC)
Although Americans move about and resettle more than people from any other country, the trend for current elders and baby boomers is to reside in their original communities as they age. In fact, the trend of “aging in place” has raised more and more discussions about criteria for healthy aging. One trend of aging in place is called “Naturally Occurring Retirement Community (NORC),” defined in New York as communities in which at least 45% of heads of households, and other residents, in apartments and population-dense neighborhoods have grown older. Nationwide, NORCs are considered to exist when a disproportionate number of older people live in a building or neighborhood (Lanspery, 1995). NORCs vary by location, physical dimensions, population size, demographic characteristics, reasons for existence, and ownership characteristics. According to Lanspery (1995), NORCs are the most dominant, and yet overlooked, form of senior housing. Generally, the official term “NORC” is used when 50% of the residents in a given geographic area are age 60 or over. In addition to vital case management and health services, a variety of social, recreational, and healthy support services are provided within a NORC, and mobility is usually not an issue for seniors to access on-site services. NORC-based senior programs are believed to help reduce isolation and postpone elders’ institutionalization (Lanspery, 1995), increasing a senior’s overall functioning in his or her community.
The provision of social- and health-related services through a NORC with the collaboration of the senior residents and various social, health, and housing providers not only provides an ideal setting for human services and social work practice, but more importantly, also meets the needs of the diverse aging population in urban areas.
Needs of Home and Community-Based Services and Older Minorities
Whether or not older adults are living in NORCs, there is no doubt that many older adults are living in the community. According to DFTA, the majority of older adults age 65 or over resided in a community, and only about 4% were institutionalized in 2000. In addition, the Federal Interagency Forum on Aging-Related Statistics showed that about 30% of older people lived in areas considered “central cities” (cited by McInnis-Dittrich, 2005, page 5).
Urban social work needs to be fluid and timely in its response to the needs of older people. Community-dwelling older adults might not be frail or have physical limitations. Indeed, their health status can be varied. In 2005, about 36% of older adults in New York City had mobility and self-care limitations (NYCDFTA, 2008). They might need certain home- and community-based services, such as supportive social services and nutrition services, to help them continue to live independently, semi-independently, or interdependently and reduce institutionalization.
Another critical urban concern has the tendency to be ignored: poverty among older adults. There is no denying that Social Security and other benefits have reduced the rate of poverty since the enacting of critical welfare policies developed in our country since the Great Depression. In the U.S., there was a 10% poverty rate in the group 65 and older in 2005 (DFTA, 2008). But in New York City, about 20% of older adults were living in poverty. In the Bronx, about 33% of the older population are living at 150% of the poverty level, and 43% are at 200%. And the rate has unfortunately increased 14% between 2000 and 2005. And with our current fiscal recession, this number will increase. To add to the financial woes of an aging society, older minority people aging in their communities will have additional difficulties. Poverty is a critical issue, and we need to make certain that our elder citizens do not face financial problems. As such, it is our duty as citizens to ensure our representative government continues and improves benefits, entitlements, and other financial assistance to build a safety net for this at-risk population. If our government can use our taxpayer resources to build an economic safety net for some big businesses, we have to make sure our government uses our resources to provide a safety net for “the least.”
Implications
How do present and future human services and social workers identify and meet these needs in both direct practice and policy? The implications address the specific challenges for urban social work: rising needs for specialized professional training—the curricula of gerontologist and geriatric social work must be re-tooled across the social work spectrum. Are programs addressing enough of the uniqueness of older persons of color? National data do not give us a lot of information about older persons of color, from demographic distribution to their specific needs. This makes it difficult for the curricula to provide up-to-date, proper and précis knowledge about the aging population. For instance, the research on racial minority senior citizens having greater rates of depression needs to enrich curricula, alter practice, and improve policy addressing mental health issues.
To equip students with important knowledge of aging, the gerontology programs should also make more interdisciplinary efforts. To increase the readiness of all professions and provide multidisciplinary perspectives, educators and students need practical sessions or training to understand physical, psychological, and social changes as we all age. Some departmental collaborative efforts can fulfill this purpose.
Another implication is to ensure that social work plays the role of advocate in seeking additional funding for new programs and restoring funding for previous successful programs for the older populations. Most of the U.S. national social and welfare policies were established within the past 75 years to improve older people’s lives. Social Security was first started in 1935, when seeing the grave effects of a macro economic downturn on the lives of the aged. But it was not until the 1960s that federal spending for programs for older adults expanded rapidly.
In addition to economic climate, our societal values will affect social policy development. Hooyman and Kiyak (2008) state that there is no doubt that our current social policy is shortsighted and fails to deal with social trends and long term planning (p. 678). We all need to take a part of the role of social work as advocate to negotiate long-term benefits for older adults. Particularly, older ethnic minority citizens are less likely to seek formal services because of their language barrier and lack of knowledge. Developing programs that match older minorities’ culture and language can increase and improve the quality of their lives.
Last but not least, providing culturally competent practice is not only a culture and language adjustment, but also a must-have attitude. This is and will always be a challenge to urban social work in our time. As we know, the increasing percentage of older minority people as part of the total population will be high, and the services should increase to match their numbers and needs. As service providers, human services and social workers should move forward in understanding and providing culturally competent practice. A profession that has a foundational principle of working with vulnerable populations like minorities of color should do research to identify the uniqueness of the ethnic groups that they are working with and develop cultural sensitivity toward these groups.
Although language and cultural barriers can prevent older immigrants from seeking health care and other formal services from mainstream society, they also provide the opportunity for more skilled elders to volunteer in helping their diverse neighbors hurdle such barriers.
NYCDFTA. (2003). The older population in New York City: Changes in race, Hispanic origin, and age, 1990 to 2000 an analysis of census data. (pdf file)(Spring 2003). New York: New York City Department for the Aging.
NYCDFTA. (2008). Quick facts. New York City Department for the Aging.
Lanspery, S. (1995). AAAs and NORCs. Retrieved October 9, 2003, from http://www.homemods.org/library/pages/aaa.htm.
Hooyman, N.R., & Kiyak, H. A(2008). Social gerontology: A multidisciplinary perspective (Eighth ed.). Boston: Allyn and Bacon.
McInnis-Dittrich, K. (2005). Social work with elders: A biopsychosocial approach to assessment and intervention (Second ed.). Boston: Allyn and Bacon.
Novak, M. (2006). Issues in aging. Boston: Allyn and Bacon.
Man Wai Alice Lun, Ph.D., is Assistant Professor of Human Services at Borough of Mahattan Community College of CUNY in New York City. Her research interests include educational gerontology, long-term care services, and spirituality issues. She has contributed a chapter entitled, “A Day in the Life of a Naturally Occurring Retirement Community” in the book DAYS IN THE LIVES OF GERONTOLOGICAL SOCIAL WORKERS.
This article is from the Spring 2010 issue of THE NEW SOCIAL WORKER. Copyright 2010 White Hat Communications. All rights reserved.
All material published on this website Copyright 1994-2023 White Hat Communications. All rights reserved. Please contact the publisher for permission to reproduce or reprint any materials on this site. Opinions expressed on this site are the opinions of the writer and do not necessarily represent the views of the publisher. As an Amazon Associate, we earn from qualifying purchases.

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
9 Social Work with Older Adults
Learning Objectives
In this chapter the student will be reviewing:
- Overview of gerontology and health complications
- Common issues: health complications, costs, caregivers
- The place of assisted living and nursing facilities for older adults
- Common issues for geriatric social workers
In this chapter, the student will focus on social work practice: social work with older adults. We will consider some important considerations in the study of gerontology, common health complications for the older adult, and some of the more common concerns for the geriatric social worker.
Gerontology
One of the fastest-growing populations that social workers provide services to is the aging population. For social workers, older adults offer unique challenges that are not present in other populations. There are many challenges that aging adults face in our society which range from medical and mental health to financial concerns. Below are some usual challenges that they face in this country that social workers will have to be familiar with.
Important Health Complications
Among the most shared challenges facing older adults are medical conditions that attack cognition. Dementia and Alzheimer’s Disease are the most common medical conditions that older adults suffer from; both directly impair cognition to various levels. Dementia is a general term for loss of memory and other mental abilities severe enough to interfere with daily life. The most common form of Dementia is Alzheimer’s disease. In 2023, there are roughly 4.7 million Americans over 65 have dementia from Alzheimer’s disease (Alzheimer’s Association, 2023). Each form of dementia has different symptoms and physical impact on the brain. Social workers will need to be versed in several types of dementia and the interventions available to best address their clients’ needs.
Along with medical conditions that impact cognition, there are also many illnesses and diseases that impact physical health. As we age, our body begins to break down over time. Our immune systems are no longer able to fight off infections and illnesses that could occur earlier in the lifespan. There are a multitude of illnesses and diseases that the elderly population are more susceptible to. All too often, physical health deterioration leads to elderly individuals to be placed in nursing facilities, as they can no longer care for themselves without medical professionals available around the clock.
Not only are older adults more prone to diseases that impact physical health and cognition, but the population has its own unique set of mental health concerns. As we age, there are also mental health concerns that are a direct result of growing older. Depression is common among the aging population due to a variety of reasons. Grief and loss are two contributing factors to elder depression. Isolation is also a contributing factor for depression. Isolation rates for older adults are high due to physical immobility and lack of transportation. Social workers working with this population must address grief, loss, and isolation with their clients to provide better mental health care.
Managing the Cost of Aging: Another major challenge of aging is the simple cost of aging. Most older adults are unemployed due to advanced age and physical health. Many live off Social Security and retirement benefits and many utilize Medicare and Medicaid for insurance. Those who live in assisted living communities or nursing facilities have a clear majority of their income allocated for their care. The cost of medications, general living expenses, and food often monopolizes the fixed income of older adults.
The Role of Caregivers for Older Adults
Caregivers can be medical professionals, family members, or everyday individuals that provide care for the aging population in the home. Caregivers often come in the form of family such as adult children taking care of their elderly parents. Caregiving can play a demanding and strenuous role.
Many caregivers are often faced with the challenges of working outside the home while still trying to provide care. However, caregivers play a key role in enabling older adults to remain in the community for as long as possible.
The Role of Assisted Living and Nursing Facilities for Older Adults:
Assisted living facilities are small communities or facilities that provide limited assistance for older adults. Most often, elderly couples and individuals who are still in good health will reside in these forms of care. Assisted living options offer more independence for those who reside in them. Assisted living facilities often do not employ social services, for the elders who need these services, they must be sought outside of assisted living services. Larger assisted living communities may contract with outside social service agencies to provide services.
Nursing facilities provide a wide range of services for residents. All meals and domestic services are covered by staff. There are a variety of medical professionals that are employed by these facilities. They provide 24-hour medical care for those who can no longer remain in the community and need extra support than assisted living facilities provide. Many nursing facilities also provide rehabilitation services such as physical therapy, for those recovering from surgery or serious illness.
Along with nursing staff, nursing facilities employ a broad range of professions to best provide services. Social workers, dietitians, physical therapists, maintenance staff, and environmental services are just some professions outside of nursing that are employed in these types of facilities. Social workers in nursing facilities are tasked with the residents’ mental health and emotional well-being. Social workers in these facilities most commonly work with residents who are experiencing depression, anxiety, grief and loss, and dementia. Social workers often play a significant role in nursing facilities as they may also help with admissions, day-to-day activities, and discharge planning.
Being a Geriatric Social Worker:
The aging population faces many unique challenges. Finances, health, mental health, and political considerations must all be considered when social workers provide services to the aging population. Growing older is inevitable, however, social workers can make the process smoother than those who have entered the later stages of life.
Competencies for the social worker with older adults:
- The social worker must be aware of age-related personal and professional values. Such understanding is elicited with self-reflection and study.
- As with all other populations, the social worker must be able to practice in a culturally competent manner (as is stated in the NASW (National Association of Social Workers) Code of Ethics).
- Practice with a willingness to advocate for the aging population with health and social service agencies and as members of interdisciplinary teams on behalf of older adults and their families.
- Assist older adults and their families in learning about their rights to available resources, and their right to be informed about any decisions and actions that will impact the older adult.
- To conduct a biopsychosocial assessment that is certainly inclusive of biological, psychological, and social factors, as well as attention to family, cultural, and spiritual factors.
- Be aware of community resources (the role of the broker) and link such resources to the older adult and their family.
- As alluded to in the cultural competency noted above, the social worker must be knowledgeable of the physical, language, and cognitive strengths and limitations of older adults.
With the various and sometimes limited resources offered, social workers must know how to navigate a system to better provide for their clients. With the rising cost of health care and an ever-changing political environment, social workers are tasked with advocating and serving those in the population who may not be able to do so themselves. People of advanced age are valuable contributing members of our world and as social workers, we must stand to make a better future for all.
Alzheimer’s Association. (2023) 2023 Alzheimer’s Disease Facts and Figures. Alzheimers Dement 19(4). DOI 10.1002/alz.13016.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American Psychiatric Association.
Mullin, E. (2013, Feb 26). How to pay for nursing home costs: Medicare, Medicaid, and other resources can help minimize the cost of long-term care. U.S. News and World Report. Retrieved from https://health.usnews.com/best-nursing-homes/articles/how-to-pay-for-nursing-home-costs
National Center on Elder Abuse. (2005). Elder abuse prevalence and incidence. Washington, DC: National Center on Elder Abuse.
National Council on Aging. (2022). Get the facts on fall prevention. Retrieved from https://www.ncoa.org/article/get-the-facts-on-falls-prevention
Nursing Home Alert: Abuse and Neglect Lawsuit Resource. (2017). State Surveys. Retrieved from http://www.nursinghomealert.com/state-nursing-home-surveys
Sollitto, M. (2016). Urinary tract infections in the elderly. Retrieved from https:// www.agingcare.com/articles/urinary-tract-infections-elderly-146026.htm
Introduction to Social Work: A Look Across the Profession Copyright © 2022 by James Langford, LCSW and Craig Keaton, PhD, LMSW is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

Case studies
These three case studies help you to consider different situations that people with dementia face. They are:
- Raj , a 52 year old with a job and family, who has early onset dementia
- Bob and Edith , an older married couple who both have dementia and are struggling to cope, along with their family
- Joan , an older woman, who lives alone and has just been diagnosed with dementia
Each case study contains:
- A vignette setting out the situation
- An ecogram showing who is involved
- An assessment which gives essential information about what is happening and the social worker’s conclusion
- A care and support plan which says what actions will be taken to achieve outcomes
You can use the practice guidance to think about how you would respond in these situations.

- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

Social Work Practice with Older People

Also viewable online via Adobe Connect
Select from the buttons on the right to move through the case study resources.
Resources to support social work with older people.
This website provides resources to support social work with older people.
Social work with older people is also called Gerontological Social Work. It is a specialist area of practice that is concerned with maintaining and enhancing the quality of life and wellbeing of older people and their families and with promoting independence, autonomy, and dignity.
How to use the website
The website centres on the case study of Don and Madge, a retired couple dealing with the consequences of ageing. The case study moves through seven time periods as their circumstances change and the responsibilities for caring develop.
The case study is designed to explore some of the complex issues associated with increasing frailty and escalating care and support needs in late life. It does not look at safeguarding or capacity as these topics are well covered in existing guidance. Instead the focus is on vital but neglected aspects of practice: the psycho-social and physical processes that underlie many of the experiences and challenges of late life; and the relational skills needed for practice that promotes prevention and well-being as required by the Care Act 2014.
Each stage of the case study highlights important Values and Ethics; Law and Policy; Knowledge, Evidence and Good Practice; Skills; Activities and Additional Resources. These relate to what is happening in the case study. Go to the Professional Development section to find out more about how this website can be used to improve your practice.
Acknowledgements
The case study was developed and written in 2016 by Gero (G)8 , a group of social work academics engaged in research and teaching in gerontology and gerontological social work in UK universities. Members of G8 are all qualified social workers with a strong commitment to promoting and enhancing professional practice with older people and their families, primarily through developing research and resources to support social work practitioners and students working in this area.
The website was updated with additional resources in 2019. These are added to the end of each of the Additional Resources sections in the different stages of the case study.
- Equal opportunities
- Complaints procedure
- Terms and conditions
- Privacy policy
- Cookie policy
- Accessibility

Case Study 5 – Older Adults
The following case vignette provides key concepts that could be considered when developing a plan of care for a patient who may require a controlled substance to manage their health concerns. As with any clinical situation, there are many patient variables that must be considered, including comorbid conditions, social determinants of health and their personal choices. You may choose to include different or additional health history and physical examination points, diagnostic tests, differential diagnoses and treatments depending on your patient’s context however this case vignette focuses on the aspects relevant to controlled substances.
June is a 73 year old woman who is a new patient recently referred to the primary care clinic and seeing Matt, the NP. She is seeking a refill for her lorazepam, which she has been taking for anxiety/poor sleep since her husband’s death 10 years ago. Her prescribed dose is 1 mg at bedtime, but she has been taking 2 mg at bedtime for the last 2 to 3 months due to poor sleep. She also takes a tablet during the day with glass of scotch for anxiety. Her other medications include candesartan and paroxetine for depression. June is a patient in the clinic so Matt has her health history available on the EMR. Matt takes a full health history. Pertinent findings in relation to this CDS use vignette is reported here.
She tells Matt that she had an ED visit 2 months ago after a motor vehicle accident where she crashed car into a parked car while driving home from the grocery store. She received a refill for her lorazepam at that time. Finally, she fell at home 3 weeks ago after tripping while taking out the garbage. She did not present for assessment but thinks she sprained her wrist. She has been taking ibuprofen 2 to 3 times daily for pain and wants Tylenol with codeine (T3). Matt attempts to open discussion of benzodiazepine use and falls/accidents. She is surprised and says “this has never been an issue, no one ever told me this before”.
Clinical office – including a desk, two chairs, an exam table, an EMR on computer, a BP cuff/machine, and a stethoscope.
Matt is wearing shirt and slacks, with a lab coat. Brown short hair.
Matt: So I understand you need a refill on your medication today June. June: Yes…I am almost out of my lorazepam prescription because I’ve needed to take an extra one at night for the last couple of months to help me sleep. Sometimes I need one through the day too because I get anxious. I tried having a shot of Scotch but that doesn’t help at all. I also want a few of those Tylenol with Codeine to help with the pain in my wrist. I fell a couple of weeks ago and the ibuprofen isn’t helping. My daughter gave me a couple of T3’s and they really worked! Matt: OK…let’s talk about the wrist injury first. How did it happen? June: I tripped on a mat while I was taking out the garbage. I was feeling a little dizzy that day like I get sometimes. I didn’t think it was anything so I didn’t get it checked. I don’t want people to think I’m sick all the time. I was in the ED a couple of months ago after a little car accident but everything was OK.
Matt is thinking about history questions for the wrist injury:
| – for wrist pain |
Matt: Now that you mention it, I do see a report here about the ED visit. So you weren’t hurt. What can you tell me about the accident? Were you feeling dizzy that day? June: As a matter of fact, I think I was feeling a little dizzy that morning. I figured it’s because I haven’t been sleeping all that great…the anniversary of my husband’s death always makes me unsettled. Matt: Do you remember if you took any extra lorazepam that day or the night before? June: I’m not sure but I probably did because I hadn’t been sleeping well for a while before that. Matt: What about any alcohol…did you have anything to drink that day before you went out? June: Oh no…I’d never to that! I only have a drink if I know I don’t have to drive anywhere…usually in the afternoon while I’m watching my shows. Matt: OK…what about the day that you fell and hurt your wrist…do you remember if you’d taken any extra pills or if you had anything to drink?” June: Wow…that’s hard to remember…I’m not sure.
Matt thinks about the additional assessments for the wrist injury, falls risk and use of alcohol along with her benzodiazepines.
Matt: I have to tell you that I’m a little worried about a couple of things June. You tell me that you are taking more lorazepam than what was initially prescribed and that you are also using alcohol. When you use this medication and along with your blood pressure medicine and the pill for your depression, they can work together to make you dizzy and disoriented. That could be the reason for your fall and even the car accident. Do you remember any other falls?” June: I trip every once in a while but I figure that’s because I’m getting old and I’m not in shape like I used to be when I exercised a lot. Wow…this has never been an issue…no one ever told me this before!
Matt thinking about other tools her could use to assess June today. As Matt is discussing this with June he is thinking about the other tools he would use to confirm his diagnosis.
| – a tool that screens for alcohol misuse. could be used as it also covers drug use. – Falls Risk for Older People in the Community is an evidence-informed tool that can classify risk for falls among community-based older adults. – a self-administered questionnaire that allows patients to rate their pain and the impact it is having on their daily functioning. (Generalized Anxiety Disorder -7 question scale) – a self-administered tool that allows patients to rate their anxiety. – (Geriatric Depression Scale) – a 9-item questionnaire to screen and diagnose patients with symptoms of depression. (See the resources area for further information about these tools) |
Matt: From what you’ve told me, your depression score hasn’t changed since the last time it was recorded on your health record and you tell me you’re feeling anxious but your score only shows this as mild right now. I’m not saying that this isn’t something that we need to talk about but I think your paroxetine is still at a good dose for you. I am concerned that you are drinking alcohol while taking the lorazepam.
| Select lab tests you could order for June: | – dizziness (rule out anemia). – dizziness (rule out diabetes). – could order due to alcohol use (provider discretion). – dizziness (rule out hypothyroidism). – (no chest pain). – (kidney function due to medications and dizziness). |
| The BEST answers today are: .
| |
Matt: OK June, here’s the plan I propose. I will give you a 30-day supply of your lorazepam as it was originally prescribed which is once daily at bedtime. I’m going to order an X-ray of your wrist to see if there are any broken bones. I’d like to suggest that you get some counseling to help with the anxiety because taking extra lorazepam is not safe when added to the other medications you take and I’m really worried about you getting hurt from a fall. Finally, I’d like to book an appointment to see you again in a week to look at the X-ray and talk some more about your symptoms. June: You mean you aren’t going to give me something for this pain in my wrist? Matt: No June…not until we see if there are any broken bones. I think we’d be better getting you in to see the clinic physiotherapist who can help you with some treatments for the pain and exercises to get it strong again. In the meantime, you can keep using your wrist support and take plain Tylenol for pain.
| Complete a treatment agreement for June using the . |
Matt: Do you have any other questions? June: No…I’m not happy that I can’t have any T3s but at least I might be able to sleep now that I’ll have enough of my other pills. I guess I have to come back in a week then. Matt: I’d like to see you again after you’ve had your X-ray…yes but you can always call back if anything changes.
Learning Outcome
By the end of this learning outcome, the participant should be able to:
- Recognize misuse of prescription controlled substances through history, physical and diagnostic tests in an older adult.
- Predict risk for falls, depression, anxiety and substance misuse in an older adult.
- Manage safe prescribing of benzodiazepines in the older adult
- Examine the use of treatment agreements in the older adult.
- Recognize the impact of prescribed control drug substances on patient safety in the elderly population.
Resources and Links
- FROP-com screen
- Benzodiazepine Use and Taper
- Geriatric Depression Scale
- Brief Pain Inventory
- CAGE questionnaire
- CAGE-AID questionnaire
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Case Report of a 63-Year-Old Patient With Alzheimer Disease and a Novel Presenilin 2 Mutation
Wells, Jennie L. BSc, MSc, MD, FACP, FRCPC, CCRP *,† ; Pasternak, Stephen H. MD, PhD, FRCPC †,‡,§
* Department of Medicine, Division of Geriatric Medicine, Schulich School of Medicine and Dentistry, Western University
† St. Joseph’s Health Care London—Parkwood Institute
‡ Molecular Medicine Research Group, Robarts Research Institute
§ Department of Clinical Neurological Sciences, Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON, Canada
The authors declare no conflicts of interest.
Reprints: Jennie L. Wells, BSc, MSc, MD, FACP, FRCPC, CCRP, Department of Medicine, Division of Geriatric Medicine, St. Joseph’s Health Care London—Parkwood Institute, Room A2-129, P.O. Box 5777 STN B, London, ON, Canada N6A 4V2 (e-mail: [email protected] ).
This is an open access article distributed under the Creative Commons Attribution License 4.0 (CCBY), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. http://creativecommons.org/licenses/by/4.0/
Early onset Alzheimer disease (EOAD) is a neurodegenerative dementing disorder that is relatively rare (<1% of all Alzheimer cases). Various genetic mutations of the presenilin 1 ( PSEN1 ) and presenilin 2 ( PSEN2 ) as well as the amyloid precursor protein (APP) gene have been implicated. Mutations of PSEN1 and PSEN2 alter γ-secretase enzyme that cleaves APP resulting in increase in the relative amount of the more amyloidogenic Aβ42 that is produced. 1
PSEN2 has been less studied than PSEN1 and fewer mutations are known. Here, we report a case of a 63-year-old woman (at the time of death) with the clinical history consistent with Alzheimer D, an autopsy with brain histopathology supporting Alzheimer disease (AD), congophylic angiopathy, and Lewy Body pathology, and whose medical genetic testing reveals a novel PSEN2 mutation of adenosine replacing cytosine at codon 222, nucleotide position 665 (lysine replacing threonine) that has never been previously reported. This suggests that genetic testing may be useful in older patients with mixed pathology.
CASE REPORT
The patient was referred to our specialty memory clinic at the age of 58 with a 2-year history of repetitiveness, memory loss, and executive function loss. Magnetic resonance imaging scan at age 58 revealed mild generalized cortical atrophy. She is white with 2 years of postsecondary education. Retirement at age 48 from employment as a manager in telecommunications company was because family finances allowed and not because of cognitive challenges with work. Progressive cognitive decline was evident by the report of deficits in instrumental activities of daily living performance over the past 9 months before her initial consultation in the memory clinic. Word finding and literacy skills were noted to have deteriorated in the preceding 6 months according to her spouse. Examples of functional losses were being slower in processing and carrying out instructions, not knowing how to turn off the stove, and becoming unable to assist in boat docking which was the couple’s pastime. She stopped driving a motor vehicle about 6 months before her memory clinic consultation. Her past medical history was relevant for hypercholesterolemia and vitamin D deficiency. She had no surgical history. She had no history of smoking, alcohol, or other drug misuse. Laboratory screening was normal. There was no first-degree family history of presenile dementia. Neurocognitive assessment at the first clinic visit revealed a Mini Mental State Examination (MMSE) score of 14/30; poor verbal fluency (patient was able to produce only 5 animal names and 1 F-word in 1 min) as well as poor visuospatial and executive skills ( Fig. 1 ). She had fluent speech without semantic deficits. Her neurological examination was pertinent for normal muscle tone and power, mild ideomotor apraxia on performing commands for motor tasks with no suggestion of cerebellar dysfunction, normal gait, no frontal release signs. Her speech was fluent with obvious word finding difficulties but with no phonemic or semantic paraphrasic errors. Her general physical examination was unremarkable without evidence of presenile cataracts. She had normal hearing. There was no evidence of depression or psychotic symptoms.

At the time of the initial assessment, her mother was deceased at age 79 after a hip fracture with a history long-term smoking and idiopathic pulmonary fibrosis. Her family believes that there is possible German and Danish descent on her father’s side. Her father was alive and well at age 80 at the time of her presentation with a history coronary artery disease. He is still alive and well with no functional or cognitive concerns at age 87 at the time of writing this report. Her paternal grandfather died at approximately age 33 of appendicitis with her paternal grandmother living with mild memory loss but without known dementia or motor symptoms until age 76, dying after complications of abdominal surgery. Her paternal uncle was diagnosed with Parkinson disease in his 40s and died at age 58. Her maternal grandmother was reported to be functionally intact, but mildly forgetful at the time of her death at age 89. The maternal grandfather had multiple myocardial infarctions and died of congestive heart failure at age 75. She was the eldest of 4 siblings (ages 44 to 56 at the time of presentation); none had cognitive problems. She had no children.
Because of her young age and clinical presentation with no personality changes, language or motor change, nor fluctuations, EOAD was the most likely clinical diagnosis. As visuospatial challenges were marked at her first visit and poor depth perception developing over time, posterior cortical variant of AD was also on the differential as was atypical presentation of frontotemporal dementias. Without fluctuations, Parkinsonism, falls, hallucinations, or altered attention, Lewy Body dementia was deemed unlikely. After treatment with a cholinesterase inhibitor, her MMSE improved to 18/30, tested 15 months later with stability in function. Verbal fluency improved marginally with 7 animals and 3 F-words. After an additional 18 months, function and cognition declined (MMSE=13/30) so memantine was added. The stabilizing response to the cholinesterase inhibitor added some degree of confidence to the EOAD diagnosis. In the subsequent 4 years, she continued to decline in cognition and function such that admission to a care facility was required with associated total dependence for basic activities of daily living. Noted by family before transfer to the long-term care facility were episodic possible hallucinations. It was challenging to know if what was described was misinterpretation of objects in view or a true hallucination. During this time, she developed muscle rigidity, motor apraxias, worsening perceptual, and language skills and became dependent for all activities of daily livings. At the fourth year of treatment, occasional myoclonus was noted. She was a 1 person assist for walking because of increased risk of falls. After 1 year in the care home, she was admitted to the acute care hospital in respiratory distress. CT brain imaging during that admission revealed marked generalized global cortical atrophy and marked hippocampal atrophy ( Fig. 2 ). She died at age 63 of pneumonia. An autopsy was performed confirming the cause of death and her diagnosis of AD, showing numerous plaques and tangles with congophilic amyloid angiopathy. In addition, there was prominent Lewy Body pathology noted in the amygdala.

Three years before her death informed consent was obtained from the patient and family to perform medical genetic testing for EOAD. The standard panel offered by the laboratory was selected and included PSEN1 , PSEN2 , APP, and apoE analysis. Tests related to genes related to frontotemporal dementia were not requested based on clinical presentation and clinical judgement. This was carried out with blood samples and not cerebrospinal fluid because of patient, family, and health provider preference. The results revealed a novel PSEN2 mutation with an adenosine replacing cytosine at nucleotide position 665, codon 222 [amino acid substation of lysine for threonine at position 221 (L221T)]. This PSEN2 variant was noted to be novel to the laboratory’s database, noting that models predicted that this variant is likely pathogenic. The other notable potentially significant genetic finding is the apoliprotein E genotype was Є 3/4 .
β-amyloid (Aβ) is a 38 to 43 amino acid peptide that aggregates in AD forming toxic soluble oligomers and insoluble amyloid fibrils which form plaques. Aβ is produced by the cleavage of the APP first by an α-secretase, which produces a 99 amino acid C-terminal fragment of APP, and then at a variable “gamma” position by the γ-secretase which releases the Aβ peptide itself. It is this second γ-cleavage which determines the length and therefore the pathogenicity of the Aβ peptides, with 42 amino acid form of Aβ having a high propensity to aggregate and being more toxic.
The γ-secretase is composed of at least 4 proteins, mAph1, PEN2, nicastrin, and presenilin . Of these proteins, presenilin has 2 distinct isoforms ( PSEN1 and PSEN2 ), which contain the catalytic site responsible for the γ-cleavage. PSEN mutants are the most common genetic cause of AD with 247 mutations described in PSEN1 and 48 mutations described in PSEN2 (Alzgene database; www.alzforum.org/mutations ). PSEN2 mutations are reported to be associated with AD of both early onset and variable age onset as well as with other neurodegenerative disorders such as Lewy Body dementia, frontotemporal dementia, Parkinson dementia, and posterior cortical atrophy. 2–4 In addition, PSEN2 has associations with breast cancer and dilated cardiomyopathy. 3
PSEN2 mutants are believed to alter the γ-secretase cleavage of APP increasing the relative amount of the more toxic Aβ42. The mean age of onset in PSEN2 mutations, is 55.3 years but the range of onset is surprisingly wide, spanning 39 to 83 years. Over 52% of cases are over 60 years. All cases have extensive amyloid plaque and neurofibrillary tangles, and many have extensive alpha-synuclein pathology as well. 5
In considering the novelty of this reported PSEN2 mutation, a literature search of Medline, the Alzgene genetic database of PSEN2 and the Alzheimer Disease and Frontotemporal Dementia Mutation Databases (AD&FTMD) were completed ( www.molgen.vib-ua.be/ADMutations ). The mutation presented here (L221T) has never been described before.
Although this mutation has not been described, we believe that it is highly likely to be pathogenic. This mutation is not conservative, as it replaces a lysine residue which is positively charged with threonine which is an uncharged polar, hydrophilic amino acid. The mutation itself occurs in a small cytoplasmic loop between transmembrane domain 4 and 5, which is conserved in the PSEN1 gene, and in PSEN2 is highly conserved across vertebrates, including birds and zebrafish all the way to Caenorhabditis elegans , but differs in Drosophila melanogaster (fruit fly) ( Fig. 3 ). We examined this mutation using several computer algorithms which examine the likelihood that a mutation will not be tolerated. Both SIFT ( http://sift.bii.a-star.edu.sg ) and PolyPhen-2.2.2 (HumVar) ( www.bork.embl-heidelberg.de/PolyPhen ) predicts that this variant is pathogenic. Interestingly, it is noted that PSEN1 mutations after amino acid 200 develop amyloid angiopathy. 5,7

This patient also had an additional risk factor for AD, being a heterozygote for the apoЄ4 allele. Among other mechanisms, its presence reduces clearance of Aβ42 from the brain and increases glial activation. 8 Although the apoЄ4 allele is known to lower the age of onset of dementia in late onset AD, it has not been clearly shown to influence age of onset of EOAD in a limited case series. 9 It should be noted that heterozygote state may have contributed to an acceleration of her course given the known metabolism of apoЄ4 and its association with accelerated cerebral amyloid and known reduction in age of onset. 10
Given that there is no definite family history of autosomal dominant early onset dementia, it is likely that her PSEN2 mutation was a new random event. With the unusually wide age of onset it is conceivable that one of her parents could still harbor this PSEN2 mutation. The patient’s father, however, is currently 87 and living independently at the time of writing this manuscript, making him highly unlikely to be an EOAD carrier. Nonpaternity is an alternate explanation for the lack of known first-degree relative with EOAD; however, this is deemed unlikely by the family member who provided the supplemental history. Her mother died at age 79, so she could conceivably carry our mutation but we do not have access to this genetic material. Without extensive testing of many family members it would be impossible to speculate about autosomal recessive form of gene expression. In addition, the genetic testing requested was limited to presenilins , APP, and apoE mutations. Danish heritage may add Familial Danish dementia as a remote consideration; however, Familial Danish dementia has a much different clinical presentation with long tract signs, cerebellar dysfunction, onset in the fourth decade as well as hearing loss and cataracts at a young age. 11 This disease has high autosomal dominant penetration which also makes it less likely in the patient’s context. This specific gene (chromosome 13) was not tested. The autopsy findings do not support this possibility. There are reports of Familial AD pedigrees in Germany, including a Volga pedigree with PSEN141I mutation in exon 5, but this is clearly separate from our mutation which is in exon 7. Our mutation was also not observed in a recent cohort of 23 German individuals with EOAD which underwent whole genome sequencing, but did find 2 carriers of the Volga pedigree. It is also possible that both the PSEN2 mutation and the ApoE genotype contributed to her disease and early onset presentation. This case illustrates the multiple pathology types which occur in individuals bearing PSEN2 mutations, and highlights the later ages in which patients can present with PSEN2 mutations. 12
ACKNOWLEDGMENT
The authors acknowledge Gwyneth Duhn, RN, BNSc, MSc, for her support of this paper.
- Cited Here |
- View Full Text | PubMed | CrossRef |
- Google Scholar
- PubMed | CrossRef |
Alzheimer disease; presenilin ; mutation
- + Favorites
- View in Gallery
Readers Of this Article Also Read
18</sup>f-florbetapir pet/ct findings in an early-onset alzheimer disease patient carrying presenilin-1 <em xmlns:mrws=\"http://webservices.ovid.com/mrws/1.0\">g378e</em> mutation', 'cistaro angelina md; quartuccio, natale md; cassalia, laura md; vai, daniela md; guerra, ugo paolo md; atzori, cristiana md; rainero, innocenzo phd; imperiale, daniele md', 'alzheimer disease & associated disorders', 'october-december 2022', '36', '4' , 'p 347-349');" onmouseout="javascript:tooltip_mouseout()" class="ejp-uc__article-title-link">brain 18 f-florbetapir pet/ct findings in an early-onset alzheimer disease..., frontotemporal dementia knowledge scale: development and preliminary..., epileptic seizures in alzheimer disease: a review, quality of life in alzheimer disease: a comparison of patients’ and caregivers’ ....
- Skip to primary navigation
- Skip to main content
- Skip to primary sidebar

Healthy Aging and Ethnogeriatrics
Case Study 4
Mrs. Evangelista is a 92-year-old cachectic frail-looking Filipino female who was diagnosed with dementia 7 years ago. Her oral intake has decreased over the past 6 months and she has occasional choking spells when being fed. She has lost a significant amount of weight (20 lb.) over the past year despite complete nursing care provided at home by her 2 unmarried daughters, who are now in their 60’s. She spends most of her time sitting in a chair or lying in bed, is dependent in all of her activities of daily living (ADL’s), and had falling incidents twice in the past year. She cannot carry on an intelligible conversation and can only express herself by uttering a few incomprehensible words and by using non-verbal gestures. She is incontinent with bowel and bladder function, and has developed multiple small stage 2 pressure ulcers in her buttocks.
When the health care provider made a home visit, one of the daughters expressed concern regarding her mother’s progressive weight loss due to feeding difficulties, and requested that a PEG tube be inserted. Through her knowledge of other people’s experience she believed that this intervention would improve the patient’s nutritional status. The health care provider maintained that it was not an appropriate intervention for this setting and explained the risks and benefits of the procedure to the family member. The daughter was not quite satisfied or convinced, and continued to insist on having it placed.
Discussion Topics
1. What cultural values and beliefs could explain the family member’s behavior and her concern regarding the patient’s declining condition?
2. As the healthcare provider, how can you develop the trust of the family members, and be able to formulate culturally meaningful and appropriate patient-centered goals that would be acceptable to family members as well?


IMAGES
VIDEO
COMMENTS
Case Studies The following case studies were included to highlight different ways that social workers can assess and intervene with issues of social isolation. These cases are free to you to use, modify, and incorporate into your teaching.
This case study examines the impact of going into a care home on the caring relationship, and the need to support transitions and respond to family conflict, including through mediation. It also considers issues of identity and sexuality.
This case study considers issues around being a ' sandwich carer' - that is, caring for both a parent and a child - maintaining employment and working with a whole family including family group conferences, as well as the impact of dementia and the role of assistive technology.
The case study is about Don and Madge, a retired couple dealing with the consequences of ageing. The case study moves through seven time periods as their circumstances change and the responsibilities for caring develop. The case study is designed to explore some of the complex issues associated with increasing frailty and escalating care and ...
Learn what a geriatric social worker is, how to become one, what career opportunities are available and much more in our comprehensive guide.
Much attention is on transitional care to decrease financial costs and improve patient outcomes. Social workers may be uniquely qualified to improve care transitions and have not previously been used in this role. We present a case study of an older, dually eligible Latina woman who received a social work-driven transition intervention that ...
The implications address the specific challenges for urban social work: rising needs for specialized professional training—the curricula of gerontologist and geriatric social work must be re-tooled across the social work spectrum. Are programs addressing enough of the uniqueness of older persons of color?
Section 3 provides case studies in which older adults find themselves in need of health promotion activities and successfully engage in them. Contained within this section are cases discussing older adults challenged with primary prevention interventions, such as immunizations, smoking cessation, and good sleep hygiene devel-opment.
Common issues for geriatric social workers. In this chapter, the student will focus on social work practice: social work with older adults. We will consider some important considerations in the study of gerontology, common health complications for the older adult, and some of the more common concerns for the geriatric social worker.
Case studies. These three case studies help you to consider different situations that people with dementia face. They are: Raj, a 52 year old with a job and family, who has early onset dementia. Bob and Edith, an older married couple who both have dementia and are struggling to cope, along with their family.
The aging of our society, both in the United States and globally, demands an increased focus on aging within the social work profession and the preparation of more social workers skilled in working with older people and their families. This page highlights aging research across many domains, identifies gaps in knowledge, and makes ...
The case study was developed and written in 2016 by Gero (G)8, a group of social work academics engaged in research and teaching in gerontology and gerontological social work in UK universities. Members of G8 are all qualified social workers with a strong commitment to promoting and enhancing professional practice with older people and their families, primarily through developing research and ...
Case Study 5. Case Study 5 - Older Adults. The following case vignette provides key concepts that could be considered when developing a plan of care for a patient who may require a controlled substance to manage their health concerns. As with any clinical situation, there are many patient variables that must be considered, including comorbid ...
This study explored social worker's perspectives on the challenges and. rewards of working with the aging population. The study used 23 social worker. participants completed a questionnaire focused on the work of gerontological. social work. The participants gave their perspective on the need for more social.
The following case study includes a short story from multiple viewpoints and a set of questions designed to facilitate discussion about respecting and caring for the elderly and the importance of maintaining commitments and volunteering for selfless reasons.
Social Work Case Study: A 75-Year-Old Patient. 767 Words4 Pages. Case study: A 75-year-old woman who lives in an apartment building designed for senior living. Recently her neighbors have lodged complaints with the social worker in the building. They state that there are bad odors and roaches migrating to their apartments from her apartment.
Were these drives and created remaining or institutional backings? INSTITUTIONAL-government is mindful projects for tending to for those out of luck Geriatric Social Work BSW's give case the board and care coordination to advance autonomy, work with advances, secure wellbeing. ; can do things MSW's do
fits the elderly clients seeking assistance. This study investigated the experiences of geriatric case officers working with grieving elderly clients who are ither in hospitals or in their private homes. A qualitative methodology was employed and, interviews were conducted with four geriatric case officers working within elderly care dep
This compilation of case studies is of direct relevance in Singapore although the issues and themes about human responses, moral philosophy and ethical codes of practice makes it relevant to many contexts in which social work is practised.
Here, we report a case of a 63-year-old woman (at the time of death) with the clinical history consistent with Alzheimer D, an autopsy with brain histopathology supporting Alzheimer disease (AD), congophylic angiopathy, and Lewy Body pathology, and whose medical genetic testing reveals a novel PSEN2 mutation of adenosine replacing cytosine at ...
The core principles of early geriatric models of care include CGA (which identifies geriatric syndromes and psychosocial problems in addition to medical conditions, especially among frail older adults), ( Stuck et al., 1993) a geriatric-focused interdisciplinary team (for example, nurses, therapists, and social workers with special interest or ...
Case Studies in Geriatric Medicine This case-based approach to geriatric medicine is suitable for all health professionals and trainees who provide care for the elderly, including interns, residents, geriatric fellows, physicians in practice, and nurse practitioners. Illustrated with more than 40 cases based on the authors' experienceinclinicalpractice ...
Case Study 4. Mrs. Evangelista is a 92-year-old cachectic frail-looking Filipino female who was diagnosed with dementia 7 years ago. Her oral intake has decreased over the past 6 months and she has occasional choking spells when being fed. She has lost a significant amount of weight (20 lb.) over the past year despite complete nursing care ...
The Effect of Geriatric Intervention in Frail Elderly Patients Receiving Chemotherapy for Colorectal Cancer (GERICO) study (ClinicalTrials.gov identifier NCT02748811) was a single-center, randomized, phase 3 study evaluating the benefit of GA with targeted interventions in adults aged 70 and older (N = 142) receiving adjuvant or first-line ...