- Success stories
- Spine and back
- Pelvis and perineum
- Head and neck
- Neuroanatomy
- Cross sections
- Radiological anatomy
- Types of tissues
- Body systems
Register now and grab your free ultimate anatomy study guide!

Circulatory (cardiovascular) system
Author: Niamh Gorman, MSc • Reviewer: Francesca Salvador, MSc Last reviewed: September 12, 2023 Reading time: 34 minutes
/images/vimeo_thumbnails/258779944/Ynw0qC4YypuucQulRKAbNg_overlay.jpg)
:background_color(FFFFFF):format(jpeg)/images/library/13981/T946_cardiovascular_system_full_view_of_arteries_anterior_view.png)
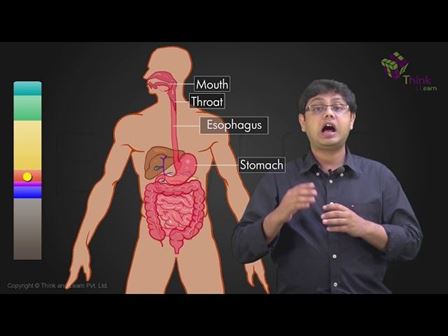
The circulatory system, also called cardiovascular system , is a vital organ system that delivers essential substances to all cells for basic functions to occur. Also commonly known as the cardiovascular system, is a network composed of the heart as a centralised pump, blood vessels that distribute blood throughout the body, and the blood itself, for transportation of different substances.
The circulatory system is divided into two separate loops: The shorter pulmonary circuit that exchanges blood between the heart and the lungs for oxygenation; and the longer systemic circuit that distributes blood throughout all other systems and tissues of the body. Both of these circuits begin and end in the heart.
| Functions | Transport of gases, nutrients, electrolytes, wastes, hormones |
| Heart | - myocardium, endocardium, epicardium - left and right atria, left and right ventricles - arteries (oxygenated blood), veins (deoxygenated blood) |
| Blood vessels | Arteries, veins, capillaries Hierarchy: Heart -> arteries -> arterioles -> capillaries [gas exchange - oxygenated blood becomes deoxygenated] -> venules -> veins -> heart |
| Circulations | - superior and inferior vena cava (with deoxygenated blood) -> right atrium -> right ventricle -> right and left pulmonary artery -> capillaries of each lung (oxygenation of the blood) -> pulmonary veins -> left atrium -> systemic circulation - left atrium -> left ventricle -> aorta and all of its branches -> capillaries -> veins -> superior and inferior vena cava -> pulmonary circulation - ascending aorta -> right coronary artery -> right marginal branch, posterior interventricular artery, left coronary artery -> anterior interventricular branch (anastomoses with the posterior branch), circumflex artery |
| Blood | with (red blood cells) - contain hemoglobine and carry oxygen throughout the blood vessels (white blood cells) - immune system cells (platelets) - coagulation cells |
| Clinical relations | Arteriosclerosis, cerebrovascular disease, peripheral artery disease, aneurysm, varices, arrhytmia, heart failure |
This article will explain everything that is important about the circulatory system, as well as the clinical relations to it.
Pulmonary circulation
Systemic circulation, coronary circulation, portal system, shunts and anastamoses, erythrocytes (red blood cells), leukocytes (white blood cells), thrombocytes (platelets), vascular diseases, cardiac diseases, blood disorders.
The main function of the circulatory (or cardiovascular) system is to deliver oxygen to the body tissues, whilst simultaneously removing carbon dioxide produced by metabolism. Oxygen is bound to molecules called haemoglobin that are on the surface of the red blood cells in the blood.
Beginning in the heart , deoxygenated blood (containing carbon dioxide) is returned from systemic circulation to the right side of the heart . It is pumped into pulmonary circulation and is delivered to the lungs , where gas exchange occurs. The carbon dioxide is removed from the blood and replaced with oxygen. The blood is now oxygenated, and returns to the left side of the heart .
Have you already learned the basic anatomy of the heart? Test your knowledge with our heart diagrams, quizzes and worksheets.
From there, it is pumped into the systemic circuit, delivers oxygen to the tissues , and returns again to the right side of the heart . The blood also acts as an excellent transport medium for nutrients, such as electrolytes, as well as hormones. The blood also transports waste products, that are filtered from the blood in the liver.
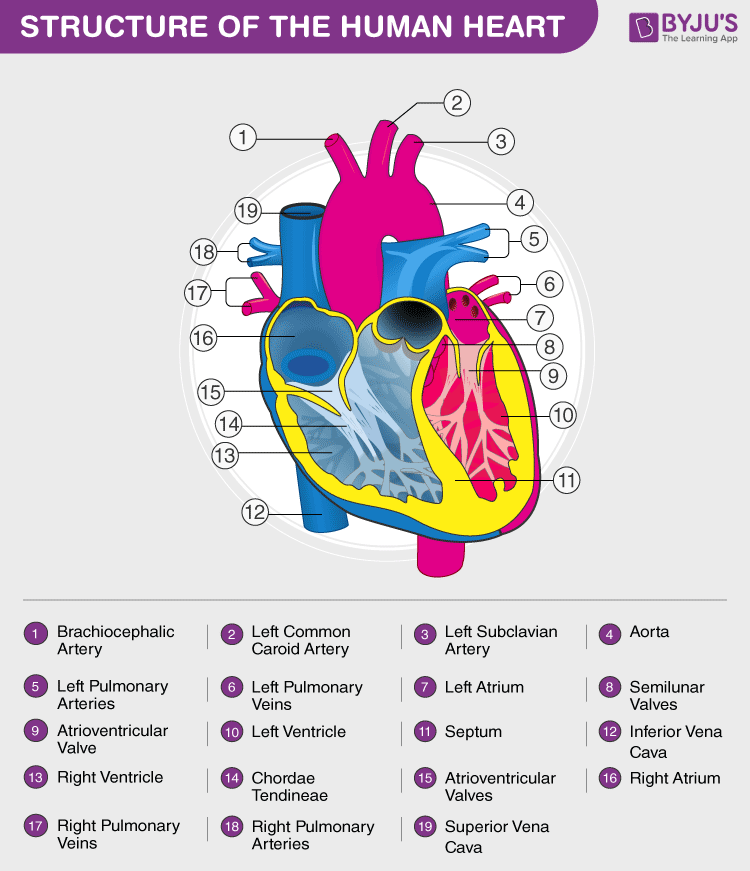
The heart is a muscular pump that is the central component of the circulatory system. It is divided into a right and left side by a muscular septum . The muscular component of the heart, the myocardium , is composed of involuntary cardiac muscle . It is lined by a membrane called the endocardium internally, as well as an external epicardium . Contraction of the cardiac muscle cells is stimulated by electrical impulses that are sporadically fired from the regulatory centres of the heart: the sinuatrial node in the roof of the right atrium , and the atrioventricular node in the septum between the atria and the ventricles . The sinuatrial node is widely regarded as the natural pacemaker of the heart.
:watermark(/images/watermark_5000_10percent.png,0,0,0):watermark(/images/logo_url.png,-10,-10,0):format(jpeg)/images/overview_image/468/1IxWFpQK2LNWsfTZew10w_heart-in-situ-1_english.jpg)
The heart is continuously going through a series of contractions and relaxations. Systole refers to when the ventricles of the heart simultaneously contract, diastole is when the ventricles relax. During systole, blood is forcibly pumped out of the ventricles into the outflow tracts of their corresponding circulation. The atria are filling with blood at the same time. During diastole, the ventricles are relaxed, and blood flows from the atria into the corresponding ventricles.
:watermark(/images/watermark_only_413.png,0,0,0):watermark(/images/logo_url_sm.png,-10,-10,0):format(jpeg)/images/anatomy_term/superior-vena-cava-4/Cz2rOQ20R7bi8cjScR4w_V._cava_superior_02.png)
Deoxygenated blood from systemic circulation returns to the right atrium via the superior and inferior vena cava . The coronary sinus , returning blood from the coronary circulation, also opens into the right atrium. The blood in the right atrium flows into the right ventricle through the right atrioventricular valve ( tricuspid valve ) during diastole. During systole, the right ventricle contracts, directing the blood into the conus arteriosus at the base of the pulmonary trunk . Contraction of the ventricle causes the tricuspid valve to shut, preventing backflow of blood into the right atrium. Between the conus arteriosus and the pulmonary trunk is a valve; the pulmonary valve . In diastole, the valve closes to prevent backflow of blood into the right ventricle.
:watermark(/images/watermark_only_413.png,0,0,0):watermark(/images/logo_url_sm.png,-10,-10,0):format(jpeg)/images/anatomy_term/ventriculus-dexter/VmlfiM0Kkbtm6ZR3PhPa2A_Ventriculus_dexter_01.png)
The pulmonary trunk splits into a right and a left pulmonary artery , serving the right and left lung respectively. Deoxygenated blood flows into the capillaries of each lung, where it is then oxygenated. The pulmonary veins collect the newly oxygenated blood from the lung, and return it to the left atrium, where it will be passed into systemic circulation.
Oxygenated blood enters the left atrium from the pulmonary circulation via the pulmonary veins . During diastole, blood passes from the left atrium to the left ventricle through the left atrioventricular valve ( bicuspid valve ). In systole, the left ventricle contracts, forcing blood into the aorta . The blood passes through the false into the ascending aorta .
The ascending aorta becomes the arch of the aorta , where three large arteries branch from it: the brachiocephalic trunk , the left common carotid artery and the left subclavian artery. These arteries supply oxygenated blood to the head and neck , and to the upper limbs .
The descending aorta is the continuation of the arch of the aorta inferiorly. In the thorax it is referred to as the descending or thoracic aorta , and gives off numerous branches in the thorax.
The latter passes into the abdominal cavity through the diaphragm through the aortic hiatus at the level of T12. From there, it is referred to as the abdominal aorta . The abdominal aorta gives branches to the structures in and surrounding the abdominal cavity, and terminates by bifurcating into the common iliac arteries , which will supply the pelvic cavity and lower limbs .
:watermark(/images/watermark_only_413.png,0,0,0):watermark(/images/logo_url_sm.png,-10,-10,0):format(jpeg)/images/anatomy_term/arcus-aortae-2/BWWzWSigXmPksiNsf2NA_Aortic_arch_wo_nerves.png)
The branches of the aorta passes towards their intended structures, with branching occurring along their length. The terminal branches enter the tissues, and pass towards the capillary beds of the tissues in vessels called arterioles . Gas exchange occurs between the blood and the tissues. The blood is collected from the capillaries by venules , which unite to form the veins of the systemic circulation. These veins ultimately drain to the right atrium via the superior and inferior venae cavae.
The coronary circulation refers to the blood supply to the heart itself. It is a component of the systemic circulation . The right and left coronary arteries branch directly from the ascending aorta, immediately above the aortic valve. The right coronary artery passes to the right and gives off two main branches: the right marginal branch along the right border of the heart and the posterior interventricular ( posterior descending ) artery, which descends along the interventricular septum on the base of the heart.
Learn everything about the coronary arteries and veins with the following study unit and quiz.
:format(jpeg)/images/study_unit/coronary-arteries-and-cardiac-veins/WPXMtQtGZlik50VQJfSEQ_Coronary_vessels.png)
The left coronary artery passes to the left, and gives off the anterior interventricular ( Ieft anterior descending ) artery which descends on the anterior aspect of the interventricular septum to anastamose with the posterior interventricular artery at the apex of the heart. It also gives off the circumflex artery .
:watermark(/images/watermark_5000_10percent.png,0,0,0):watermark(/images/logo_url.png,-10,-10,0):format(jpeg)/images/overview_image/265/PynvUfMRtYgKF9AjA2YvKw_coronary-arteries-and-cardiac-veins-anterior-OV_english.jpg)
The venous drainage of the heart is achieved by the coronary sinus , which drains the main veins of the heart:
- the great cardiac vein ,
- the middle cardiac vein , and
- the small cardiac vein , which drains directly into the right atrium.
:background_color(FFFFFF):format(jpeg)/images/library/12591/Heart.png)
The portal system is the system of veins that drain the blood from the intestines and directs it to the liver to be filtered. The superior and inferior mesenteric veins , draining the jejunum down as far as the upper rectum , along with the splenic vein draining the spleen, pancreas , and stomach , unite to form the hepatic portal vein , which empties blood into the liver. Toxins are filtered out by the liver, and the filtered blood is returned to the inferior vena cava via the hepatic veins.
Types of blood vessels
Arteries carry blood away from the heart. They have thick walls and a narrow lumen , to resist the high pressure from the blood being forced out of the heart. As the arteries travel toward the more peripheral tissues, they begin a process of segmentation, decreasing in diameter and wall thickness with each division. The major arterial outflow tracts of the heart are the aorta (systemic), and the pulmonary trunk (pulmonary). The coronary arteries are the arteries that supply oxygenated blood to the tissues of the heart itself.
Arteries are typically divided into three types:
:background_color(FFFFFF):format(jpeg)/images/library/8687/aCakVCMk7M8xtaJDDC6A4w_Artery.png)
- distributing arteries that transport blood to specific organ systems, with a high muscular component in their walls;
- the small and muscular resistance vessels or arterioles
Pressure in these arteries decrease from its highest level in the conducting arteries to the lowest in the arterioles. The walls of the arteries are divided into 3 layers: the tunica intima (internal), the tunica media (middle) and the tunica externa (external).
:watermark(/images/watermark_5000_10percent.png,0,0,0):watermark(/images/logo_url.png,-10,-10,0):format(jpeg)/images/overview_image/1105/NcvJJwiQAgqPHmrvJjlMvg_histology-blood-vessels-artery_english.jpg)
For descriptive purposes, it is easiest to describe the types of blood vessels in the sequence that they occur as they pass from the heart to the peripheral tissues, and form the peripheral tissue back to the heart.
How's your knowledge of the major arteries of the cardiovascular system? Our cardiovascular system diagrams, quizzes and free worksheets are the best way to find out.
Types of arteries
:background_color(FFFFFF):format(jpeg)/images/library/8688/qqhmVxIKd7pxeygeKSM3xw_Muscular_artery_-_Coronary_artery__1___1_.png)
Large elastic arteries : are the conducting arteries and examples include the aorta and its main branches; the brachiocephalic trunk, the left common carotid artery, the left subclavian artery and the terminal common iliac arteries. These carry blood from the heart to the smaller conducting arteries. The pressure in the these arteries is at the highest level of the entire circulatory system. The tunica intima is lined by endothelium and the tunica media has a large elastic component . Muscular arteries : are the distributing arteries and contain a large proportion of smooth muscle in their tunica media. They are lined internally by endothelium. The tunica externa is composed of fibromuscular connective tissue , with a larger proportion of elastic fibres than collagen contributing to the elasticity of this layer in the muscular arteries.
Arterioles : are the connecting vessels between the muscular arteries and capillary beds of the organs. They have small endothelial cells with nuclei projecting into the lumen of the vessel, a thin muscular wall about two layers thick, and a thin tunica externa. They control the flow of blood into the capillaries by contraction of the smooth muscle in the tunica media, which acts as a sphincter. Capillaries : are the closest vessels to the organs. Their walls measure one large endothelial cell in thickness and provide the only barrier between the blood and the interstitial fluid of the tissues. They have a narrow lumen which is just thick enough to allow the passage of the largest blood cells. The permeability of capillaries varies depending on the surrounding tissues and the type of junctions between the adjacent endothelial cells in the vessels wall.
Types of veins
:background_color(FFFFFF):format(jpeg)/images/library/8690/BAAXvRC08x4u6lTHGG3L4w_Vein.png)
Venules : are formed when two or more capillaries converge. They are lined by flat endothelial cells and a thin tunica externa. These are called postcapillary venules. The muscular component appears in venules as their lumen increases, producing muscular venules. Veins : are formed with the union of muscular venules. In comparison to arteries, veins have a relatively thin wall and a larger lumen . The structure of the walls is similar to that of arteries, but a considerably smaller amount of muscle is present in the tunica media of veins. Veins are capacitance vessels , meaning they have a distensible wall and can expand to accommodate large volumes of blood.
Most peripheral veins have structures called valves , which are projections of the tunica interna into the lumen of the vessel. Valves prevent the backflow of blood through the veins, by passively closing when the direction of flow of the blood reverses. Valves are absent in the veins of the thorax and abdomen . The overall hierarchy of blood vessels follows this order: arteries → arterioles → capillaries → venules → veins.
So now you know the types of blood vessels - but what about their histological features? Learn and test your knowledge at the same time using our blood vessels diagrams and artery and vein quizzes.
Arteries form connections between each other called anastomoses, which creates a continuous supply of blood throughout different areas. In the event of occlusion of an artery to a specific area, blood supply can be maintained to the tissue via the anastomosis with an artery of an adjacent area.
:background_color(FFFFFF):format(jpeg)/images/library/8691/ftHyvFFkmI50nVN4IWvGQg_Anastamosis_between_superior_mesenteric_artery_and_inferior_pancreatic_artery_02.png)
A direct anastomosis occurs where two arteries are joined directly to each other, such as in the radial and ulnar arteries via the palmar arches. Convergence anastomoses occur where two arteries unite to form a single artery, as in when the vertebral arteries join to form the basilar artery . A transverse anastomosis is where a small artery connects two larger arteries, for example, the anterior communicating artery connecting the right and left anterior cerebral arteries .
Connections between the arterial and venous systems are present throughout the body. For example, in the mesentery , metarterioles can connect the arterioles to venules, and blood can either flow into or bypass the capillary beds. Control of this flow is by local demand of the individual tissues.
Arteriovenous anastomoses are a direct connection between small arteries and small veins. These occur in regions such as the skin of the nose, lips and ears , in the mucosa of the alimentary canal, and nasal and oral cavities .
A portocaval anastomosis occurs where there is a connection between the systemic and portal system of veins. These occur at venous plexuses, such as around the oesophagus , the umbilicus , and the rectum.
The blood is the mobile component of the circulatory system. Blood is bright red when oxygenated and dark red/purple when deoxygenated. Blood consists of a cellular component suspended in a liquid called plasma.
Plasma is a clear fluid that accounts for approximately 55% of blood, and is composed of over 90% water. Plasma contains a high concentration of electrolytes , such as sodium, potassium and calcium. Also dissolved in plasma are plasma proteins . These include clotting factors, mainly prothrombin, immunoglobulin, polypeptides and other protein molecules, and hormones.
:watermark(/images/watermark_only_413.png,0,0,0):watermark(/images/logo_url_sm.png,-10,-10,0):format(jpeg)/images/anatomy_term/erythrocyte/1jmYAWXa8oYVdAFE85dM5Q_Erythrocytes.png)
Erythrocytes are the most abundant of blood cells, accounting for approximately 99% of all blood cells. They are biconcave disc shaped cells that lack a nucleus. Erythrocytes have a globulin protein called haemoglobin on their surface for oxygen to bind to. The proportion of red blood cells to plasma is called the haematocrit . Measured as a percentage, it is used as a reference point for the oxygen carrying capacity of a person; when there is a higher percentage of red blood cells present, more haemoglobin is present to carry oxygen.
Aged erythrocytes are ingested by macrophages in the liver and spleen . The iron released in the breakdown of the erythrocytes is used to synthesise new erythrocytes, or is stored in the liver as ferritin .
Blood Grouping
Antigens are present on the surface of erythrocytes, and can react with antibodies causing agglutination of the red blood cells. This is the basis of the ABO blood grouping system . Individuals inherit two alleles, one from each parent, that code for a specific blood group. Blood groups can be homozygous , where the alleles are the same, or heterozygous where alleles are different:
| Allele | |
| AA | A |
| BB | B |
| OO | O |
| AB | AB |
| AO | A |
| BO | B |
Specific blood groups have antibodies that are sensitive to the alleles absent from their erythrocytes. For example, blood group A will carry the A antigen and the anti-B antibodies.
These are divided in 5 groups: monocytes, lymphocytes , neutrophils , basophils and eosinophils . These groups are distinguishable from each other by cell size, shape of nucleus and cytoplasm composition. These groups can themselves be grouped into 2 groups: granulocytes and agranulocytes . This classification is based on the presence or lack of granules in the cytoplasm of the cell. Collectively, white blood cells form part of the immune response .
Granulocytes
Neutrophils, eosinophils and basophils fall into this category of white blood cells. Leukocytes are classified into this group based on the presence of vesicles, called granules, in their cytoplasm. Granulocytes are largely involved in inflammatory and allergic responses .
Neutrophils : are the most abundant white blood cells, accounting for about 40-75% of all leukocytes. The number of neutrophils varies, and increases in response to acute bacterial infections. They have an irregular, segmented nucleus. They mainly function in the defence of the body against microorganisms, and can ingest foreign substances by phagocytosis . They are also involved in inflammation. Neutrophils have a short life span, spending 4-7 hours in circulation and a few days in connective tissue.
Eosinophils : are similar to neutrophils, but are far fewer in number. Their nucleus is prominently bilobed, and the granules in the cytoplasm are large. Their motility mirrors that of other leukocytes, and they migrate from the circulation into the tissues. They increase in number in allergic reactions, and play a prominent role in the defense against parasites . They are only weakly phagocytotic, involved more so in the breakdown of particles too large for phagocytosis. The circulate for approximately 10 hours, and spend a few days in the tissues.
Basophils : are the smallest of the granulocytes. They are small in number, accounting for 0.5-1% of all leukocytes. They are distinguishable by the large, clearly visible granules in their cytoplasm. Their nucleus is irregular shaped, and sometimes bilobed, but is often obscured by the granules. The granules are membrane bound vesicles containing a variety of inflammatory agents. These vesicles herniate, dumping their contents and triggering immediate allergic hypersensitivity , such as seen in reactions like hay fever. The dumping of these agents also triggers the migration of other granulocytes to the area.
Agranulocytes
Monocytes and lymphocytes fall into this category due to the absence of granules in their cytoplasm. They are also referred to as mononuclear leukocytes, referring to the presence of a single lobed nucleus.
Monocytes : are the largest leukocytes in relation to physical size. They account for 2-8% of all leukocytes. They typically have large uni-lobed nuclei with a characteristic indentation on one side. Monocytes are phagocytic cells . Circulating monocytes transition into macrophages when they migrate from the circulation to the tissues.
Lymphocytes : are the second most abundant leukocyte, accounting for 20-30%. They are the only white blood cell that can re-enter circulation having migrated to the tissues. They are variable in size and lifespan: some live merely days, others are long-lived, and are involved in immunological memory . Lymphocytes are divided into two types: B-lymphocytes and T-lymphocytes.
B-lymphocytes synthesize and secrete antibodies specific to foreign molecules. They also stimulate other non-lymphocytic leukocytes to phagocytose. B-lymphocytes are involved in adaptive immunity , and produce memory B cells, which remain in the body and are activated in response to a specific antigen.
T-lymphocytes develop and mature in the thymus , then migrate to and are stored in secondary lymphoid organs. They are involved in the ongoing immunity of the cell, with their function not solely dependent on the response to an antigen. T-lymphocytes are divided into three subgroups. Cytotoxic T cells directly target infected cells; Helper T cells direct destruction by recruitment of other immune cells; and Regulatory T cells are involved in developing the tolerance of cells to an antigen.
Platelets are small, irregular shaped cells that lack a nucleus. They are present in large numbers and have highly adhesive properties. Platelets are highly involved in haemostasis . They are activated in the event of damage to a blood vessel. They accumulate at the site of injury and essentially plug the wound. Following adherence at the site of injury, platelets and the surrounding tissues release factors that trigger a complex sequence of events. A clot is formed to close the wound. The clot is then retracted and the edges of the wound are pulled together to close it and repair the vessel. Platelets circulate in the blood for approximately 10 days, before they are removed from the blood by macrophages .
Want some practice identifying blood cells? Then try the quiz below!
Clinical notes
Diseases affecting the cardiovascular system are collectively referred to as cardiovascular diseases. Vascular diseases relate to the blood vessels. Cardiac diseases affect the heart itself. Hematologic diseases are those of the blood. Diseases of the cardiovascular system can be congenital (present since birth) or acquired (related to age, diet, lifestyle and predisposition).
Arteriosclerosis is the thickening of the walls of arteries, reducing function. Atherosclerosis is a specific form of arteriosclerosis, where plaque builds up on the endothelium of arteries, causing them to narrow and reducing oxygen delivery to the tissues.
Coronary artery disease occurs in the arteries supplying the heart itself, with narrowing of the coronary arteries causing reduced oxygen delivery to the heart tissue. This can result in a condition called angina , which is essentially spasming of the coronary arteries due to reduced blood flow. Myocardial Infarction (heart attack) is also caused by the narrowing of the coronary arteries due to atherosclerosis. A myocardial infarction occurs when the artery becomes completely occluded due to dislodged plaque or development of a thrombus (blood clot).
Cerebrovascular disease affects the arteries supplying the brain . One of the most common presentations is ischemic stroke , which is also caused by atherosclerosis. Ischemic stroke results in a reduced blood flow to brain regions, leading to impaired brain function. It can be caused by the development of a thrombus or the passing of an embolus (blockage causing substance) from another region of the body to the cerebral circulation.
Peripheral artery disease is reduced blood flow to the limbs due to atherosclerosis.
An aneurysm is a localised weakening in the wall of a blood vessel. It can result in bulging of the vessel wall. Thrombus formation and embolisation can also occur. Aneurysms can rupture, leading to significant blood loss depending on where they occur. Particularly lethal sites of aneurysm formation are in the abdominal aorta, the circle of Willis in cerebral circulation, and in the renal vessels.
Varices occur where blood vessels become enlarged and twisted. They can occur at multiple sites in the body. One of the most prominent sites of varices is in the veins of legs, termed varicose veins. Other common sites of varices are at sites of portocaval anastamoses, such as esophageal varices, umbilical varices (caput medusae) and anorectal varices (hemorrhoids or piles).
Cardiovascular diseases can also solely affect the heart. Cardiomyopathy is a collection of diseases that affects the heart muscle. The muscle can become enlarged (hypertrophic) and rigid, causing decreased heart function, arrhythmias (irregular heart rate), and sometimes even heart failure .
The valves of the heart can also be affected by disease. There are two main types: valve incompetence , in which the valve is unable to function sufficiently; and valve stenosis , where the orifice between the valve narrows as the valve is unable to open fully. Mitral valve disease affects the mitral valve that lies between the left atrium and ventricle. It is normally caused by a combination of valve incompetence and stenosis. Aortic valve disease affects the aortic valve, and is largely caused by stenosis of the valve with contribution from regurgitation, which is backflow through the valve.
Inflammation of the heart tissues can also occur. It includes inflammation of the inner endocardium ( endocarditis ) and the middle muscular layer ( myocarditis ). Pericarditis is the inflammation of the pericardium , which comprises the outer layer of the heart itself and the pericardial sac which encloses the heart in the thoracic cavity.
Congenital heart diseases
Congenital heart diseases are those which have been present since birth. They are largely present as left to right shunts , where blood is shunted from areas of higher pressure to areas of lower pressure. Oxygenated blood is passed back to the right side of the heart and mixed with deoxygenated blood. Such shunts can go unnoticed in a number of patients, while others may require surgical intervention.
An atrial septal defect occurs when blood is shunted from the left atrium (higher pressure) to the right atrium (lower pressure) through an opening in the interatrial septum . This opening usually results from the failure of an embryological shunt, the foramen ovale, to close after birth. This defect is specifically referred to as a patent foramen ovale . A ventriculoseptal defect is when an opening in the interventricular septum allows blood to pass from the left ventricle into the right ventricle.
Another embryological shunt exists near the heart in the embryo, shunting blood from the pulmonary trunk into the aorta. This is called the ductus arteriosus , and pressure changes after birth usually force this opening to shut. A patent ductus arteriosus occurs when the ductus does not close after birth, and allows blood to flow from the higher pressure arch of the aorta into the lower pressure pulmonary trunk.
These are disorders affecting the components of the blood. They can largely be divided depending on which of the blood cells they affect.
Anemia is a blood disorder affecting red blood cells . Patients suffering with anemia have a decreased oxygen carrying capacity due to a decrease in the number of red blood cells, or a reduced amount of haemoglobin in the blood. There are multiple different types of anemia, some of which are the following:
- Iron deficient anemia is the most common form of anemia. It is the result of insufficient intake of iron, an increase in the amount of iron lost, or inadequate absorption of iron. Women are more likely to be affected by this from of anemia due to menstruation and the higher demands of iron placed on their body during pregnancy.
- Megaloblastic anemia is caused by a decrease in the intake or absorption of vitamin B12 or folic acid. This results in the production of large, insufficient red blood cells.
- Perniciou s anemia is the result of insufficient hemopoiesis, or production of red blood cells by bone marrow.
- Hemorrhagi c anemia is caused by loss of red blood cells through excessive bleeding.
- Aplasti c anemia occurs due to the destruction of red bone marrow , which leads to a reduction in the number of red blood cells being produced.
- Sickl e cell anemia is a condition in which the shape of the red blood cells is altered into a sickle shape. These cells cannot easily pass through capillaries and tend to clump together, blocking the blood vessel. They are also prone to rupturing, with their rapid break down resulting in a reduced oxygen carrying capacity.
Leukemia refers to a group of cancers affecting the red bone marrow . Theses cancers cause abnormal white blood cells to multiply uncontrollably, which interferes with normal red blood cell, white blood cell and platelet production. This results in a decrease in oxygen carrying capacity, susceptibility to infection, and abnormal clotting. Leukemia spreads easily from the bone marrow to the lymph nodes , liver and spleen, causing them to enlarge. Symptoms are caused mainly by disruption to the production of other blood cells, including fatigue, pale skin and cold intolerance that is usually observed in anemia.
There are two methods of classification of leukemia. The first is based on the presentation of the disease: Acute leukemia refers to those that have developed rapidly; Chronic leukemia develops over an extended period of time. The second classification is based on the type of cells affected: Lymphoblastic affects lymphoid stem cells; Myelogenous affects myeloid stem cells. Thus, there are four types of leukemia:
- Acute lymphoblastic leukemia is the most common form of the disease occurring in children, though it can also affect adults as well.
- Acute myelogenous leukemia is found in both adults and children.
- Chroni c lymphoblastic leukemia is usually present in adults, especially those over the age of 55.
- Chronic myelogenous leukemia usually affects adults.
Treatment of leukemia involves methods such as chemotherapy, radiation therapy, stem cell transplantation and blood transfusion among others.
Thrombocytopenia
This is a disorder of the thrombocytes , or platelets. It results in a low number of platelets in the blood. Patients with this disorder are prone to excessive bleeding and may experience frequent nose bleeds or bleeding gums, as well as excessive bruising.
This is an inherited blood disorder that causes spontaneous bleeding or bleeding where only minor trauma has occurred. It is caused by deficiencies of different clotting factors and can vary significantly in severity.
Reference List:
- F. Netter: Atlas of Human Anatomy, 6th Edition, Elsevier Saunders (2014).
- G.J. Tortora, B. Derrickson: Principles of Anatomy & Physiology, 13th Edition, Wiley (2012).
- J.A. Gosling, P.F. Harris, J.R. Humpherson et al.: Human Anatomy, Colour Atlas and Textbook, 5th Edition, Mosby Elsevier (2008).
- M.H Ross, W. Pawlina: Histology: A Text and Atlas, Wolters Kluwer, 7th Edition (2016).
- R. Drake, A.W. Vogl, A.W.M. Mitchell: Gray’s Anatomy for Students, 3rd Edition, Churchill Livingston Elsevier (2015).
Illustrators:
- Overview of the heart in situ (ventral view) - Yousun Koh
- Aortic arch (ventral view) - Yousun Koh
- Overview of coronary arteries and cardiac veins - Yousun Koh
- Anastamosis between superior mesenteric artery and inferior pancreatic artery (ventral view) - Esther Gollan
- Coronary circulation in a cadaver - Prof. Carlos Suárez-Quian
Circulatory (cardiovascular) system: want to learn more about it?
Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster.
What do you prefer to learn with?
“I would honestly say that Kenhub cut my study time in half.” – Read more.

Learning anatomy isn't impossible. We're here to help.
Learning anatomy is a massive undertaking, and we're here to help you pass with flying colours.
Want access to this video?
- Curated learning paths created by our anatomy experts
- 1000s of high quality anatomy illustrations and articles
- Free 60 minute trial of Kenhub Premium!
...it takes less than 60 seconds!
Want access to this quiz?
Want access to this gallery.
- Biology Article
- Human Circulatory System Transportation
Human Circulatory System
The human body is a complex machine, requiring many processes to function efficiently. To keep these crucial processes running without any hitches, vital elements and components need to be delivered to the various parts of the body.
This role of transportation is undertaken by the human circulatory system, moving essential nutrients and minerals throughout the body and metabolic waste products away from the body. Below is a neat labelled Circulatory system diagram.
Read more: Human Body Anatomy
Read on to explore intricate about the human circulatory system and its components in greater detail.
Table of Contents
Double Circulation
- Blood Cells
Blood Vessels
Lymphatic system, human circulatory system diagram.
The human circulatory system consists of a network of arteries, veins, and capillaries, with the heart pumping blood through it. Its primary role is to provide essential nutrients, minerals, and hormones to various parts of the body. Alternatively, the circulatory system is also responsible for collecting metabolic waste and toxins from the cells and tissues to be purified or expelled from the body.
Features of Circulatory System
The crucial features of the human circulatory system are as follows:
- The human circulatory system consists of blood, heart, blood vessels, and lymph.
- The human circulatory system circulates blood through two loops (double circulation) – One for oxygenated blood, another for deoxygenated blood.
- The human heart consists of four chambers – two ventricles and two auricles.
- The human circulatory system possesses a body-wide network of blood vessels. These comprise arteries, veins, and capillaries.
- The primary function of blood vessels is to transport oxygenated blood and nutrients to all parts of the body. It is also tasked with collecting metabolic wastes to be expelled from the body.
- Most circulatory system diagrams do not visually represent its sheer length. Theoretically, if the veins, arteries, and capillaries of a human were laid out, end to end, it would span a total distance of 1,00,000 kilometres (or roughly eight times the diameter of the Earth).
Organs of Circulatory System
The human circulatory system comprises 4 main organs that have specific roles and functions. The vital circulatory system organs include:
- Blood (technically, blood is considered a tissue and not an organ)
- Lymphatic system
The heart is a muscular organ located in the chest cavity, right between the lungs. It is positioned slightly towards the left in the thoracic region and is enveloped by the pericardium. The human heart is separated into four chambers; namely, two upper chambers called atria ( singular: atrium ), and two lower chambers called ventricles.
Heart, a major part of the human circulatory system
Though other animals possess a heart, the way their circulatory system functions is quite different from humans. Moreover, in some cases, the human circulatory system is much more evolved when compared to insects or molluscs.
Read More: Human Heart
The way blood flows in the human body is unique, and it is quite efficient too. The blood circulates through the heart twice, hence, it is called double circulation. Other animals like fish have single circulation, where blood completes a circuit through the entire animal only once.
The main advantage of double circulation is that every tissue in the body has a steady supply of oxygenated blood, and it does not get mixed with the deoxygenated blood.
Further Reading: Double circulation

Circulation of blood in humans – Double circulation
Blood is the body’s fluid connective tissue, and it forms a vital part of the human circulatory system. Its main function is to circulate nutrients, hormones, minerals and other essential components to different parts of the body. Blood flows through a specified set of pathways called blood vessels. The organ which is involved in pumping blood to different body parts is the heart. Blood cells, blood plasma, proteins, and other mineral components (such as sodium, potassium and calcium) constitute human blood.
Blood is composed of:
- Plasma – the fluid part of the blood and is composed of 90% of water.
- Red blood cells, white blood cells and platelets constitute the solid part of blood.
Types of Blood Cells
The human body consists of three types of blood cells, namely:
- Red blood cells (RBC) / Erythrocytes
Red blood cells are mainly involved in transporting oxygen, nutrients, and other substances to various parts of the body. These blood cells also remove waste from the body.
- White blood cells (WBC) / Leukocytes
White blood cells are specialized cells, which function as a body’s defence system. They provide immunity by fending off pathogens and harmful microorganisms.
- Platelets / Thrombocytes
Platelets are cells that help to form clots and stop bleeding. They act on the site of an injury or a wound.
Blood vessels are a network of pathways through which blood travels throughout the body. Arteries and veins are the two primary types of blood vessels in the circulatory system of the body.
Arteries are blood vessels that transport oxygenated blood from the heart to various parts of the body. They are thick, elastic and are divided into a small network of blood vessels called capillaries. The only exception to this is the pulmonary arteries, which carries deoxygenated blood to the lungs.
Veins are blood vessels that carry deoxygenated blood towards the heart from various parts of the body. They are thin, elastic and are present closer to the surface of the skin. However, pulmonary and umbilical veins are the only veins that carry oxygenated blood in the entire body.
Also Read: Blood
The human circulatory system consists of another body fluid called lymph. It is also known as tissue fluid. It is produced by the lymphatic system which comprises a network of interconnected organs, nodes and ducts.
Lymph is a colourless fluid consisting of salts, proteins, water, which transport and circulates digested food and absorbed fat to intercellular spaces in the tissues. Unlike the circulatory system, lymph is not pumped; instead, it passively flows through a network of vessels.
Functions of Circulatory System
The most important function of the circulatory system is transporting oxygen throughout the body. The other vital functions of the human circulatory system are as follows:
- It helps in sustaining all the organ systems.
- It transports blood, nutrients, oxygen, carbon dioxide and hormones throughout the body.
- It protects cells from pathogens.
- It acts as an interface for cell-to-cell interaction.
- The substances present in the blood help repair the damaged tissue.
Explore More: Circulatory System
Recommended Videos:
Discover more about the circulatory system by registering at BYJU’S Biology . Find more concepts and important questions about human circulatory system Class 11 by downloading BYJU’S – The Learning App.

Frequently Asked Questions
1. how does the human circulatory system work, 2. what are the three types of circulation.
- Pulmonary Circulation
- Systemic Circulation
- Coronary Circulation
3. Is the human circulatory system open or closed?
4. what is the advantage of a closed circulatory system, 5. what is double circulation, 6. what are the dangers of high blood pressure, 7. what is a stroke, 8. what is hypertension, 9. what is hypo-tension, 10. what was the earliest circulatory system like.
Put your understanding of this concept to test by answering a few MCQs. Click ‘Start Quiz’ to begin!
Select the correct answer and click on the “Finish” button Check your score and answers at the end of the quiz
Visit BYJU’S for all Biology related queries and study materials
Your result is as below
Request OTP on Voice Call
| BIOLOGY Related Links | |
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Post My Comment
It was indeed a good blog. The concept was much clear.
nice project
I think it would help me in my studies
VERY CLEAR AND INTERSTED TO LEARN THANKS FOR CLEAR DETAILS
That was really helpful .Thank you so much
nice explanation
Very nice, it is amazing.
Thanks, That was really helpful
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 8: The Cardiovascular System
Jonathon W. Homeister; Karen L. Kelly
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Introduction, normal anatomy of blood vessels.
- DISEASES OF THE VASCULAR SYSTEM
- CONGENITAL HEART DISEASE
- CARDIOMYOPATHIES
- VALVULAR HEART DISEASE
- CARDIAC TUMORS
- PERICARDIAL DISEASES
- Full Chapter
- Supplementary Content
The heart is at the center of the cardiovascular system. The left side of the heart pumps blood oxygenated in the lungs through the aorta, arteries, arterioles, and capillaries, to the organs of the body. The organ tissues extract oxygen and nutrients from the blood in the capillaries, in exchange for carbon dioxide and waste products. The deoxygenated blood is returned to the right side of the heart through venules, veins, and the venae cavae. The right side of the heart pumps the blood through the lungs where it is again oxygenated, and back to the left side of the heart. Blood moves through this system due to pressure gradients and unidirectional valves, similar to a household plumbing system. However, unlike the static household system, the living components of our cardiovascular system are dynamic, adjusting pressure and flow to regulate blood flow and delivery to the organs of the body as dictated by physiologic need to maintain organ function and homeostasis.
This chapter covers the pathology of the tissues and organs of the cardiovascular system. The first part of the chapter discusses vascular diseases, and the second part focuses on diseases of the heart and its structures, although, as you will see, they are sometimes intertwined. Like other organ systems, diseases of this system can be either congenital or acquired. Like all organ systems, the various etiologies of these diseases can be put into general categories that physicians remember by using the mnemonic VINDICATE: vascular, infectious, neoplastic degenerative, iatrogenic/intoxication, congenital, autoimmune, traumatic, and endocrine/metabolic. You will see one or more of these etiologies causing the pathogenesis of the diseases discussed. This chapter focuses primarily on diseases of the heart and arterial system. Diseases of the venous system are not directly discussed, nor are diseases of the lymphatic system. Diseases of the pulmonary vascular system will be discussed in Chapter 9.
Blood vessels consist of arteries and veins that are categorized according to their structure, size, and function (Figure 8-1) . The arterial system carries oxygenated blood away from the heart to provide oxygen and nutrients to the cells of the body. It also modulates peripheral resistance and therefore is responsible for maintaining blood pressure. In the organs, the capillary system is responsible for the exchange of oxygen and nutrients, and waste products. The venous system carries the deoxygenated blood with its waste products back to the heart for transport to the lungs for oxygen replenishment.
Get Free Access Through Your Institution
Pop-up div successfully displayed.
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

The Biology Corner
Biology Teaching Resources

Case Study – A Tiny Heart (old version)
This case study was revised in 2023, get the NEW VERSION !
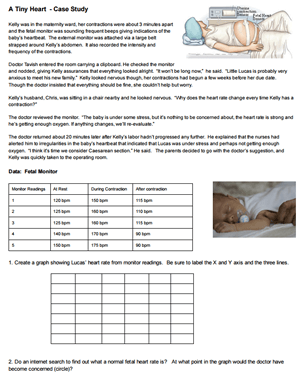
This case study focuses on a baby boy who was born with a problem with his heart. The story is based on a real scenario, though some of the names have been changed, and the parents gave permission to include photos of the infant.
Students will read about symptoms that occur when a baby is born with stenosis, or a narrowing of the artery. Students consider treatment options and compare the circulation of a fetus to that of an adult. Finally, the Ross Procedure is described where a valve from the pulmonary artery is moved to the aorta.
This case study was made for a high school anatomy class, and may not be appropriate for younger audiences. Students should have already completed the chapter on the circulatory system and have a strong foundation in how the circulatory system works. Case studies are designed to be completed in small groups so that students can have discussions and help each other with difficult vocabulary.

HS-LS1-2 Develop and use a model to illustrate the hierarchical organization of interacting systems that provide specific functions within multicellular organisms
Shannan Muskopf
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Arq Bras Cardiol
- v.111(6); 2018 Dec

Case 6 - Woman with Ischemic Heart Disease Admitted due to Chest Pain and Shock
Rafael amorim belo nunes.
Instituto do Coração do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InCor-HC-FMUSP), São Paulo, SP - Brazil
Hilda Sara Montero Ramirez
Vera demarchi aiello.
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction.
The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
During the patient's evolution, after the myocardial infarction, she was submitted to a coronary angiography in, which disclosed the presence of lesions with 70% obstruction in the right coronary, anterior descending and circumflex arteries. A left ventriculography revealed apical akinesia with signs of intracavitary thrombus in that region.
The echocardiogram (May 2009) disclosed ventricular dysfunction accentuated by diffuse hypokinesis, with a 28% left ventricular ejection fraction. Clinical and drug treatment was recommended to the patient.
The patient's evolution was asymptomatic until October 2009, when she had a cerebrovascular accident, with motor sequela.
On December 30, 2009, the patient had an episode of severe chest pain that lasted for one hour and she sought medical care.
At the physical examination, the heart rate (HR) was 100 beats per minute, blood pressure was 100/60 mmHg. Pulmonary assessment was normal. The heart examination disclosed a ++/ 6+ systolic murmur in the mitral area. The remainder of the physical examination was normal. The electrocardiogram (1h 19 min; Dec 30, 2009) showed sinus rhythm, HR of 103 bpm, PR interval of 122 ms, QRS duration of 159 ms, QT interval of 367 ms, and corrected QT of 480 ms.
There was left atrial overload, low voltage of the QRS complex in the frontal plane, probable inferior electrically inactive area, and left bundle branch block ( Figure 1 ). Chest x-ray disclosed the presence of a large pleural effusion in the right hemithorax.

Electrocardiogram - Sinus rhythm, low voltage of the QRS complex in the frontal plane, electrically inactive area in the inferior wall and left bundle branch block.
The laboratory tests showed hemoglobin 13 g/dL, hematocrit 40%, MCV 91 fL, leukocytes 12,400/mm 3 (66% neutrophils, 1% eosinophils, 1% basophils, 19% lymphocytes and 13% monocytes), 421,000/mm 3 , total cholesterol 228 mg/dL, HDL-cholesterol 35 mg / dL, LDL-cholesterol 162 mg/dL, triglycerides 157 mg/dL, CK-MB mass 5.63 ng / mL, Troponin I 0.21 ng/mL, urea 33 mg/dL, creatinine 0.66 mg/dL, sodium 137 mEq/L, and potassium 3.4 mEq/L. Venous blood gasometry showed pH 7.46, pCO 2 39.3 mmHg, pO 2 36.3 mmHg, O 2 saturation 62.7%, bicarbonate 27.7 mEq/L and base excess 4.1 mEq/L.
Approximately two hours after hospital admission, she had seizures and cardiac arrest with pulseless electrical activity, reversed in 5 min.
The electrocardiogram after the cardiac arrest (4:18 am; Dec 30, 2009) showed a HR of 64 bpm, absence of P waves, and left bundle branch block. The QRS complex alteration, in relation to the previous tracing, was a positive QRS complex in the V6 lead ( Figure 2 ).

Electrocardiogram - Sinus rhythm, left bundle branch block and positive T waves on an also positive derivative of the QRS complex.
She had a new cardiac arrest 20 min later, which was also reversed. After half an hour, a new episode of cardiac arrest occurred, which was irreversible, and the patient died (5:45 am; Dec 30, 2009).
Clinical aspects
This patient is a 67-year-old woman with cardiovascular risk factors and ischemic cardiomyopathy, with severe left ventricular systolic dysfunction. Cardiac catheterization disclosed multivessel coronary disease and apical akinesis with an intracavitary thrombus. During outpatient follow-up, clinical treatment was chosen, possibly influenced by the patient's clinical status, as well as the characteristics of the coronary anatomy.
The indication of surgical treatment with myocardial revascularization in patients with coronary heart disease with heart failure and severe left ventricular systolic dysfunction is still debatable, but recent data from the STICH study suggest a long-term survival benefit in patients undergoing myocardial revascularization. 1
During follow-up in October 2009, the patient had a clinical picture suggestive of a cerebrovascular accident that may have been of atherothrombotic origin due to the multiple cardiovascular risk factors or of cardioembolic origin, associated with intracavitary thrombi.
In December 2009 the patient was admitted to the emergency room with acute chest pain. She had mild tachycardia and borderline systolic blood pressure of 100 mmHg. The electrocardiogram showed sinus tachycardia, left atrial overload and left bundle branch block.
In patients with acute chest pain and electrocardiogram with acute or undetermined left bundle branch block, the possibility of acute myocardial infarction should be considered, especially in case of hemodynamic instability. Criteria such as those proposed by Sgarbossa et al., 2 and Smith et al., 3 modified by other authors can contribute to the diagnostic accuracy improvement in this context. 2 , 3 However, one should consider that the occurrence of left bundle branch block is more commonly a marker of previous structural heart disease.
The patient had a cardiorespiratory arrest with pulseless electrical activity (PEA) within a short time after hospital admission. In cases of acute myocardial infarction, PEA can occur in patients with severe ventricular dysfunction and cardiogenic shock and/or mechanical complications such as rupture of the left ventricular free wall with cardiac tamponade, papillary muscle rupture and / or severe dysfunction and acute interventricular septal defect.
Other conditions should be considered in patients with acute chest pain who present with rapid clinical deterioration such as aortic dissection and pulmonary thromboembolism. The chest x-ray showed a massive pleural effusion in the right hemithorax, although this finding was not readily apparent at the physical examination. In this patient, pleural effusion may be due to chronic heart failure decompensation but may also be associated with other conditions, such as rheumatologic diseases, tuberculosis or pleural carcinomatosis due to neoplasias. The last two conditions mentioned here are not uncommon in patients with chronic heart diseases.
Additionally, massive pleural effusions may coexist, in some conditions, with pericardial involvement and consequent cardiac tamponade. 4 Pleural effusion may also be present in patients with acute aortopathies, such as dissection of the aorta and aortic ulcer with associated rupture, but usually the most frequent effusion is located in the left pleural space as a consequence of the aortic anatomy. (Dr. Hilda Sara Montero Ramirez)
Main hypothesis: Acute myocardial infarction complicated by cardiogenic shock. ( Dr. Hilda Sara Montero Ramirez )
Differential diagnoses: Cardiac tamponade, Pulmonary thromboembolism and Dissection of the aorta. ( Dr. Hilda Sara Montero Ramirez )
The heart weighed 422 g and showed increased volume, with cross-sections (short axis of the ventricles) disclosing a healed transmural myocardial infarction in the left ventricular anterior and septal walls. There was wall thinning and fibrosis, with antero-apical aneurysm and thrombus at the apex ( Figure 3 ). Signs of a previous systemic thromboembolism, with previous renal and cerebral infarctions were also found, with the latter being a cavitated infarction affecting the temporal and occipital regions of the left cerebral hemisphere.

Cross-sections of the heart at the level of the ventricles (short axis) showing previous transmural infarctions in the anterior and septal walls (arrows). These same places show thinning of the wall and, localized slight dilatation (aneurysm). There is also a cavitary thrombus in the ventricular apex (asterisk).
The aorta and coronary arteries showed marked atherosclerotic involvement, with ulcerated plaques in the aorta and obstructions > 70% in the initial and middle thirds of the anterior interventricular branch of the left coronary artery and between 50 and 70% in the circumflex branch of the same artery and in the right coronary artery. Signs of congestive heart failure were found in the lungs and liver.
The terminal cause of death was pulmonary thromboembolism on the right, with infarction organization at the pulmonary base ( Figure 4 ). The right pleura showed fibrin deposits and the histological analysis showed acute fibrinous pleuritis ( Figure 5 ). There was also pleural effusion on the right (500mL of citrine-colored fluid) ( Prof. Dr. Vera D. Aiello ).

Right lung cross-section at its long axis showing the presence of thromboembolism in the central branch of the pulmonary artery (arrow). At the base, there are two triangular areas (asterisks) where the parenchyma is homogeneous and reddish in color, corresponding to recent pulmonary infarctions.

Photomicrography of the right pleura showing neutrophilic exudate on the surface (asterisk), characterizing acute pleuritis. Hematoxylin-eosin staining, objective magnification = 10X.
Anatomopathological diagnoses
- - Ischemic heart disease with healed transmural infarctions in the anterior wall and ventricular septum and anteroseptal aneurysm.
- - Apical thrombus in the left ventricle.
- - Systemic and coronary atherosclerosis of moderate to high degree.
- - Previous infarctions in the kidneys and in the temporal and occipital cortex of the left cerebral hemisphere.
- - Pulmonary thromboembolism on the right, with recent pulmonary infarction.
- - Acute fibrinous pleuritis on the right, with pleural effusion (500mL) ( Prof. Dr. Vera D. Aiello )
The patient described herein sought emergency care with chest pain and was known to have ischemic heart disease. The clinical investigation for acute infarction was inconclusive and the patient died less than 24 hours after hospital admission.
Necropsy showed previous infarctions and signs of congestive heart failure. We found no evidence of a recent infarction and attributed the chest pain to the finding of a recent pulmonary thromboembolism on the right, with pulmonary infarction and acute fibrinous pleuritis.
In a study carried out at our institution, which assessed the agreement between clinical diagnoses and necropsy findings, the greatest discrepancy occurred in cases of pulmonary thromboembolism (34.1%). 5 ( Prof. Dr. Vera Demarchi Aiello )
Section Editor: Alfredo José Mansur ( rb.psu.rocni@rusnamja )
Associated Editors: Desidério Favarato ( rb.psu.rocni@otaravaflcd ) Vera Demarchi Aiello ( rb.psu.rocni@arevpna )
Complete Your CE
Course case studies, external link, this link leads outside of the netce site to:.
While we have selected sites that we believe offer good, reliable information, we are not responsible for the content provided. Furthermore, these links do not constitute an endorsement of these organizations or their programs by NetCE, and none should be inferred.
Pathophysiology: The Cardiovascular System
Course #38832 - $90-
#38832: Pathophysiology: The Cardiovascular System
Your certificate(s) of completion have been emailed to
- Back to Course Home
- Review the course material online or in print.
- Complete the course evaluation.
- Review your Transcript to view and print your Certificate of Completion. Your date of completion will be the date (Pacific Time) the course was electronically submitted for credit, with no exceptions. Partial credit is not available.
CASE STUDY 1: ACUTE ANTEROLATERAL MYOCARDIAL INFARCTION
Present illness.
Patient A is white, 60 years of age, and works as a cab driver. While driving home after work, he develops an aching in his chest and slight, regular palpitations. The ache is still present when he goes to bed, when he wakes several times during the night, and when he gets up in the morning, seven hours after retiring. He drinks some soda water, but when the aching does not improve, he decides to go to the emergency department.
At the hospital, Patient A complains of chest pain accompanied by diaphoresis, slight shortness of breath, and nausea. Relief of pain is obtained with IV morphine sulfate. When the patient is admitted to the critical care unit (CCU), his symptoms are generally unremarkable except for recurrent pain.
Medical History
Patient A experienced the usual childhood illnesses without rheumatic fever. As an adult, he has a history of hypertension (documented on discharge from the Army at 45 years of age and when hospitalized two years ago) that has not been treated. Past surgery includes tonsillectomy and adenoidectomy as a child. A cataract was removed from his right eye two years ago.
Patient A's father died of an MI at 55 years of age. His mother is alive and well, although the patient does not know her age. Two brothers, 65 and 58 years of age, are alive and well. The patient lives alone and works approximately 72 hours per week. He has been married and divorced twice; the last divorce was four years ago. He has no children.
Assessment and Diagnosis
Upon admittance to the CCU, a full physical exam is conducted ( Table 4 ). An ECG is done and shows ST elevation. Several laboratory tests are ordered, with the following results:
Serum cardiac enzymes:
CK: 164 IU/L
LDH: 219 IU/L
Serum glutamic-oxaloacetic transaminase (SGOT): 31 IU/L
CBC: Within normal limits
Electrolytes: Within normal limits
Urinalysis: Within normal limits
PATIENT A'S PHYSICAL EXAM RESULTS
IMAGES
COMMENTS
CASE STUDY 6 - 3: CIRCULATORY SYSTEM DISORDERS, DIAGNOSTIC TESTS, AND VEIN SELECTION. A phlebotomist is called to the ER to draw a STAT hct, hgb, and plt ct on a young girl who appears extremely pale and very close to being unconscious. While checking for a good puncture site, the phlebotomist notes the " M " pattern of veins on both ...
Give a reason for your selection of specimen type CASE STUDY 6-3: CIRCULATORY SYSTEM DISORDERS, DIAGNOSTIC TESTS, AND VEIN SELECTION A phlebotomist is called to the ER to draw a STAY het. hgb, and pltct on a young girl who appears extremely pale and very close to being unconscious. While checking for a good puncture site, the phlebotomist notes ...
Circulatory system. The circulatory system, also called cardiovascular system, is a vital organ system that delivers essential substances to all cells for basic functions to occur. Also commonly known as the cardiovascular system, is a network composed of the heart as a centralised pump, blood vessels that distribute blood throughout the body, and the blood itself, for transportation of ...
Proper adherence to medications like antiplatelets, beta-blockers, and statins is crucial for managing risk factors and preventing complications. Missing doses may lead to inadequate protection, increasing the likelihood of further cardiac events or complications. Study with Quizlet and memorize flashcards containing terms like symptoms of ...
The human circulatory system possesses a body-wide network of blood vessels. These comprise arteries, veins, and capillaries. The primary function of blood vessels is to transport oxygenated blood and nutrients to all parts of the body. It is also tasked with collecting metabolic wastes to be expelled from the body.
Quizlet has study tools to help you learn anything. Improve your grades and reach your goals with flashcards, practice tests and expert-written solutions today. Scheduled maintenance: June 20, 2024 from 09:30 PM to 11:30 PM
Read chapter 8 of Pathology: A Modern Case Study, 2e online now, exclusively on AccessMedicine. AccessMedicine is a subscription-based resource from McGraw Hill that features trusted medical content from the best minds in medicine. ... The heart is the principal organ of the blood circulatory system, pumping blood throughout the body and ...
Circulatory System. Carry oxygen and nutrients to the cells of the body and carbon dioxide and waste away from the cells. Pericardium. Thin fluid filled sac around the heart. Septa (Septum) Partitions that separate the right and left chambers of the heart. Epicardium. Thin outer layer of the heart. Myocardium.
Circulation. Cardiovascular Case Series. Cardiovascular medicine provides proof of the clear benefits of evidence-based care. The evaluation and treatment of many conditions are well-defined and practice is uniform. Despite the large size and quality of this evidence base, however, the majority of clinical practice relies on the accurate ...
The human circulatory system consists of several circuits: The pulmonary circuit provides blood flow between the heart and lungs. The systemic circuit allows blood to flow to and from the rest of the body. The coronary circuit strictly provides blood to the heart (not pictured in the figure below). Image credit: Blood flow from the heart by ...
This case study was revised in 2023, get the NEW VERSION! This case study focuses on a baby boy who was born with a problem with his heart. The story is based on a real scenario, though some of the names have been changed, and the parents gave permission to include photos of the infant. Students will read about symptoms that occur when a baby ...
A 67-year-old woman sought emergency medical care due to prolonged chest pain. In April 2009 the patient had prolonged chest pain and at that time she sought medical care. She was admitted at the hospital and diagnosed with myocardial infarction. The patient had hypertension, diabetes mellitus, dyslipidemia and was a smoker.
Upon admittance to the CCU, a full physical exam is conducted ( Table 4 ). An ECG is done and shows ST elevation. Several laboratory tests are ordered, with the following results: Serum cardiac enzymes: CK: 164 IU/L. LDH: 219 IU/L. Serum glutamic-oxaloacetic transaminase (SGOT): 31 IU/L.
Biology document from Treasure Valley Community College, 2 pages, Bio 232 Circulatory System Case Study 12 March 2024 Part 1 1. 2. 3. In a fetal heart, the blood flows directly between the atriums instead of flowing to the ventricles. This is from an opening in the interatrial septum. In an adult heart, the blood flows
About this unit. Your heart sits in the middle of your chest and pumps blood from about 4 weeks after conception until the day that you die. This little pump is the size of your clenched fist and it never stops. Watch these videos to learn more about how the heart works, blood flow in arteries and veins, blood pressure, and lymphatics.
CASE STUDY 6-2: CIRCULATORY SYSTEM DISORDERS, DIAGNOSTIC TESTS, AND VEIN SELECTION A phlebotomist receives a request to collect a specimen for a PT and D-dimer on a patient. The phlebotomist remembers drawing the patient in the ER when he was complaining of leg pain. Because the patient was a difficult draw, the phlebotomist wanted to draw from ...
CASE STUDY 6-3: CIRCULATORY SYSTEM DISORDERS, DIAGNOSTIC TESTS, AND VEIN SELECTION A phlebotomist is called to the ER to draw a STAT het, hgb, and plt ct on a young girl who appears extremely pale and very close to being unconscious. While checking for a good puncture site, the phlebotomist notes the "M" pattern of veins on both arms but really ...
CASE STUDY 6-3: CIRCULATORY SYSTEM DISORDERS, DIAGNOSTIC TESTS, AND VEIN SELECTION A phlebotomist is called to the ER to draw a STAT hct, hgb, and plt ct on a young girl who appears extremely pale and very close to being unconscious. While checking for a good puncture site, the phlebotomist notes the "M" pattern of veins on both arms but really ...
allows blood to flow from the right atrium to the left atrium. Ductus arteriosus. allows blood to flow from the pulmonary artery to the aorta. Infant first breath. 1) Lungs expand. 2) Rising oxygen levels stimulate constriction of ductus arteriosus. 3) Rising pressure in the left atrium closes the foramen ovale. Embryonic lungs.
It means death of cardiac tissue or heart muscle due to decreased or no supply of blood t …. 120 Unit Overview of the Human Body A AST sana store is being Case Studies Case Study 6-1: Circulatory System Disorders and Diagnostic Tests QUESTIONS A phlebotomist receives a request to collect specimens for stat electrolytes, CK, and AST on a ...