
- Letter from the Directors
- Health Topics
- Contact CIDI
- Active Studies
- Research Networks
- COVID-19 Grand Rounds
- Clinical Case Discussions
- Innovations
- Current Efforts
- Clinical Case Discussions and Video Conference Archive
- Field Study In India
- Research Elective at JHU
- Forms & Resources
- Current Scholars
- Former Scholars
- Publications
- About this Site
- Support CIDI
- India Campaign

Sangita Shelke, MD: Preventive and Social Medicine; Diplomas in Nutrition, Hospital Administration, Psychological counseling

MBBS- S.R.T.R Medical College, Ambejogai, Marathwada University, Maharashtra, Dec- 1990. MD- Preventive and Social Medicine, Government Medical College, Aurangabad. Marathwada University, Maharashtra, Dec- 1994. PG DHA- Diploma in Hospital Administration, Society for Development and education Coimbatore, Dec 1997. PG DND- Diploma in Nutrition and Dietetics, Society for Development and education Coimbatore, Dec 1998. PG DPC- Diploma in Psychological Counselling, Society for Development and education Coimbatore, May 1999. Have done course in Clinical Trials from CMC Vellore Dec- 2009. Honors and Awards:
Passed MD-PSM, Diploma in Hospital Administration, Diploma in Nutrition and Dietetics, Psychological Counselling all exams with DISTINCTION. Research paper “Husbands commitment in safe motherhood” presented in international conference on women and child health held at Rural Medical College Loni. Nov 1998 and was awarded prize of best paper. presented research paper “ A study on female Tamasha artists from pune district.” In Annual research conference of B.J.Medical College Pune 2006 and was awarded first prize.
Research Interests: Indeed TB is a social disease with so many social problems especially the women suffering from TB/HIV undergoes a pathetic life situation. Women are silent suffers, of both HIV and TB in male dominated society of India. My ultimate desire is if I can make a difference in the lives of these silent suffers. My research interests include understanding the factors that improve overall levels and distribution of health status of women. My research interest also includes operational research and health system research. I am also interested in finding out various ways in which defaulters and drug resistant can be minimised.
- Studies/Projects
Characterization of TB-specific T Cell Responses in Highly-exposed, but Uninfected Health Care Workers in India
Assessing the impact of psychosocial involvement in health care workers with and without active tuberculosis at the byramjee jeejeebhoy government medical college, pune, india, perceptions of hcws on barriers and opportunities to airborne infection control guideline implementation, utility of the interferon-gamma release assay for latent tuberculosis infection screening among indian health-care workers.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Case study ďavid health and social care

Birch View is a residential care home in Wales. It caters for older people, lots of whom have dementia. Many of the individuals living in Birch View speak Welsh and the home tries to employ care and support workers who speak both Welsh and English. Birch View aims to treat all individuals living in the home with dignity and respect and provide services that help them achieve their personal outcomes and what matters to them, for example knowing what time they like to get up and go to bed, when they like to eat their meals and the type of food that they enjoy, what their hobbies and interests are and how they would like to stay in touch with family and friends. The home is welcoming and has lots of different activities such as: • An art club • Singing for pleasure • Film and book clubs • A gardening group • Keep fit sessions e.g. chair-based exercises The home has an activities co-ordinator who organises the clubs and groups, she is always keen to hear from the individuals living at Birch View about their interests or what they would like to try. The activities co-ordinator has resources for the clubs and groups including computer tablets that can be used to watch films for the film club. Birch View involves the local community in the home including: • Visits from school children • Weekly hairdresser • Monthly visiting Chapel Service • Visits from people with their pets • Visits to events in the local town David has recently moved into Birch View, he is 88 years old and speaks Welsh as his first language. David has been diagnosed with dementia. Until recently, David lived at home with his wife Gwen who is 85 years old. He was supported by Gwen, health and social care services and their son and daughter who both live locally, have families of their own and work full time. David has become more confused recently, he is becoming muddled between night and day and Gwen has found him wandering outside in the middle of the night. He is struggling to access the bathroom in the house, is having difficulties with continence and has had a number of falls; after the last fall he was admitted to hospital where he was treated for minor injuries. Before he was discharged from hospital, an assessment was completed with David, Gwen, their son and daughter by social services and health professionals. This included a mental capacity and best-interest assessment. It was agreed that it was in David’s best interest for him to move into a residential care home as it was no longer safe for him to stay at home. Gwen, their children and grandchildren visit him regularly. 48 David has been given a walking frame to use at Birch View but forgets to use it. Since moving into Birch View, he has become more unstable, he has fallen twice and struggles to get in and out of bed. The care and support workers have reported that he seems agitated and confused, is not sleeping well, is trying to get out of bed in the night and has little appetite. David’s family and the care and support workers are worried that he is not settling in and is struggling more with his mobility. Nicole is one of the care and support workers at Birch View, she has noticed that David tends to be more confused in the mornings but is clearer in the afternoons. This information has been recorded in his personal plan to support his communication. Nicole is working with David and his family to find out more about his interests and background. Gwen tells her that before he became unwell, he was very active, walking the dog daily and gardening. She says that he loved growing vegetables and had been a vegetarian for the past 30 years. He was a history teacher and used to belong to the local history club at the library, he loved reading and enjoyed watching old war films. He spent a lot of time with the grandchildren as they were growing up, spending time with them in the garden, planting seeds and growing plants in their own little plots on his vegetable patch. Nicole explains to Gwen that even though David’s personal plan says that he is a vegetarian, he has been choosing the meat option from the lunch time menu and then not eating it. The care and support workers are offering David vegetarian food options but he is refusing these. Nicole asks Gwen for some ideas of the type of food that David enjoyed when he was living at home as she is worried that he is not eating enough and this may be affecting him. Nicole arranges for David to meet the activities co-ordinator in the afternoon when he is less confused and more able to express what he wants. Having spoken to Gwen and David, she thinks that he may enjoy the gardening group and film club and wonders whether they could arrange for one of his favourite war films to be shown to get him interested. Describe one method used by Birch View to meet David’s communication needs. The decline in David’s mobility has the potential to impact upon his well-being. a. State two potential impacts of this on his physical well-being. State two potential impacts on his mental well-being Explain how the principles of the Mental Capacity Act have been applied in supporting David’s health and well-being.
RELATED PAPERS
Betty Ssali
thenji bhebhe
The British Journal of Psychiatry
Ogbonna Amanze
Journal of Human Behavior in the Social Environment
Roberta R Greene
BMJ (Clinical research ed.)
David Nunan
Tony Schumacher Jones
Piers Gooding , Cher Nicholson
Robin Balbernie
julie ridley
Akinola Akinyemi
Health & Social Care in the Community
Australian and New Zealand Journal of Public Health
Kathryn Refshauge
Paul Spicker
Mayada Darfour
International Journal of Leadership in Public Services
Sylvia Elaine
spsw.ox.ac.uk
Giuliana Costa
Sue Yeandle
Val Williams
Michal Synek
Jakki Cowley
David Cobley
Health and social care level 3
Emma Stevens
Gary Lashko
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Open access
- Published: 02 September 2024
Sustaining the mobile medical units to bring equity in healthcare: a PLS-SEM approach
- Jignesh Patel 1 ,
- Sangita More 1 ,
- Pravin Sohani 1 ,
- Shrinath Bedarkar 1 ,
- Kamala Kannan Dinesh 2 ,
- Deepika Sharma 3 ,
- Sanjay Dhir 3 ,
- Sushil Sushil 3 ,
- Gunjan Taneja 4 &
- Raj Shankar Ghosh 5
International Journal for Equity in Health volume 23 , Article number: 175 ( 2024 ) Cite this article
Metrics details
Equitable access to healthcare for rural, tribal, and underprivileged people has been an emerging area of interest for researchers, academicians, and policymakers worldwide. Improving equitable access to healthcare requires innovative interventions. This calls for clarifying which operational model of a service innovation needs to be strengthened to achieve transformative change and bring sustainability to public health interventions. The current study aimed to identify the components of an operational model of mobile medical units (MMUs) as an innovative intervention to provide equitable access to healthcare.
The study empirically examined the impact of scalability, affordability, replicability (SAR), and immunization performance on the sustainability of MMUs to develop a framework for primary healthcare in the future. Data were collected via a survey answered by 207 healthcare professionals from six states in India. Partial least squares structural equation modeling (PLS-SEM) was conducted to empirically determine the interrelationships among various constructs.
The standardized path coefficients revealed that three factors (SAR) significantly influenced immunization performance as independent variables. Comparing the three hypothesized relationships demonstrates that replicability has the most substantial impact, followed by scalability and affordability. Immunization performance was found to have a significant direct effect on sustainability. For evaluating sustainability, MMUs constitute an essential component and an enabler of a sustainable healthcare system and universal health coverage.
This study equips policymakers and public health professionals with the critical components of the MMU operational model leading toward sustainability. The research framework provides reliable grounds for examining the impact of scalability, affordability, and replicability on immunization coverage as the primary public healthcare outcome.
As India advances towards universal healthcare with substantial improvements in coverage, addressing marginalized communities remains a persistent concern for the current healthcare system [ 1 , 2 ]. Many improvements have been made to India's healthcare system as a result of the country's successful efforts to address a wide range of challenges, such as unequal access to treatment, a dearth of high-quality medical services, and inaccurate information [ 3 , 4 , 5 , 6 ]. Hesitancy, social stigma, ignorance, and a shortage of medical professionals have all contributed to these difficulties and served as roadblocks to enhancing access to healthcare for India's rural, tribal, and underprivileged people [ 7 , 8 ]. Therefore, it is imperative to implement broad innovative interventions in India's current primary healthcare system to address these issues and advance universal health coverage.
In this context, mobile medical units (MMUs) have a tremendous potential to provide equal and effective access to various healthcare facilities, including immunization clinics for the disadvantaged and immunocompromised population [ 9 , 10 ]. For communities cut off from mainstream services due to climatic conditions, geography, and social stigma, MMUs can be essential for providing service to immunocompromised, vulnerable, and marginalized people living in remote and challenging places [ 11 , 12 ].
Research indicates that MMUs have been crucial in delivering specialized healthcare services in addition to primary healthcare in rural regions [ 13 , 14 ]. Also, research has indicated that MMUs are particularly effective in delivering health care to India's underprivileged and neglected communities [ 15 ]. Hence, MMUs appear promising in remote areas where local health services lack the necessary resources. MMUs can provide primary healthcare services in locations lacking or with insufficient established facilities and specialized service delivery [ 16 ].
Mobile units, especially in certain areas of emergency and preventive medicine, have shown considerable potential in rural regions, but MMUs should not be adopted without careful assessment. The effective execution and long-term sustainability of this intervention depend on evaluating the critical elements of the operational model for MMUs. While numerous studies have highlighted the role of mobile medical units (MMUs) in increasing healthcare accessibility, especially in remote and underserved areas, there is a limited understanding of the specific operational models adopted by these units and their impact on healthcare outcomes [ 9 , 10 , 11 , 12 ]. The diversity in operational strategies, ranging from the type of services offered, staffing models, technological integration, to partnership networks, remains largely unexplored. Furthermore, while the immediate benefits of MMUs, such as increased healthcare access, are well-documented, there is a paucity of research examining the long-term impact of these units on healthcare outcomes along with the impact on sustaining these models for delivering other primary healthcare services. To improve the operational model for the future and provide a framework for policy analysis, it is crucial to comprehend the impacts of operational model components on primary healthcare outcomes and the model’s sustainability. Therefore, this study aims to achieve the following research objectives:
RO1 . To empirically determine the potential impact of scalability, affordability, replicability, and immunization performance on the sustainability of the MMUs operational model.
RO2 . To develop a framework of MMUs for future innovations in primary healthcare.
This study will empirically analyze the operational model of MMUs to confirm the impact on performance and sustainability. Jharkhand, Maharashtra, Meghalaya, Karnataka, Telangana, and Tamil Nadu have been selected as the sample states where the where the case organization has been operationally implemented and subjected to a thorough evaluation of these factors. The relay of work can be used to revisit the components of the operational model for MMUs by the practitioners and policymakers. The theoretical underpinnings of this study are presented in the following sub-sections, along with the hypotheses developed for empirical validation.
Scalability
Various studies have identified scalability as a prominent driver for improving healthcare outcomes [ 17 , 18 ]. Scalability is often associated with sustainability and higher performance in terms of efficiency and increased immunization coverage. Scalability in regard to a healthcare intervention refers to its potential suitability for scaling up. It is essential to have a clear understanding of the term ‘scalability’ in the context of public health to develop an effective health promotion intervention. Various studies have been conducted to explore the indicators for accurately measuring the scalability of public health interventions and examining their impact on health outcomes, such as immunization coverage and performance [ 19 , 20 ]. In this study we measured scalability by examining the delivery system, the availability of technical assistance, the organizational capacity, management, financial support, and partnerships.
Aspects like a delivery system that would ensure the reach and expansion of mobile clinics are essential components of an efficient strategy. Similarly, technology plays a significant role in the seamless dispersal of the immunization program, and a technical assistant helps blur the lines between the digital and physical worlds. Such integration keeps the delivery of vaccines, scheduling of vaccination drives, and other logistical concerns in check and ensures accountability with regard to the number of individuals immunized [ 21 ]. Another component that influences scalability is the organizational capacity of the stakeholders, for example in the mobile clinics employed in the COVID-19 vaccination drive. Mapping various areas of coordination and utilizing the organizational capacity for various operational purposes has helped mobile clinics to achieve their immunization targets. Advanced planning, timely delivery of vaccines, transportation, securing of awareness creation, mobilization of beneficiaries, proper registration, safe vaccination, and dispersal of certificates were crucial for critical ordination. All the elements discussed above require decision support as well as financial support. Decision support should focus on the inclusiveness of the tribal areas for immunization programs [ 22 ]. Similarly, financial support was also directed toward achieving immunization targets for the marginalized population, including tribal people, daily wage workers, street vendors, sex workers, etc. [ 23 ]. The partnership between mobile clinics and government agencies led to the creation of robust and scalable processes that integrated infrastructural and digital spaces for the successful deployment of a vaccine program [ 7 ].
Affordability
Affordability is essential for the government to provide healthcare services to ensure vaccines for all. Especially in a developing country like India, which comprises a large population, where health budgets have to be outlined judiciously [ 24 ]. Specific mechanisms are needed to ensure sustainable financing of vaccines available to individuals from marginalized populations [ 25 ]. The ability of mobile clinics to cover the hard-to-reach parts of the state was made possible only because of well-planned transportation by a network of ambulances. Close management of the transportation costs was of immediate need as the goal of the program was to bring a mobile clinic within reach of everyone to vaccinate the marginalized population [ 3 ]. Vaccination procurement and allocation were done appropriately by the government agencies to smoothly execute the plan [ 8 ].
Consideration was not limited to transportation costs, however, and the mobile clinic’s team was also concerned about limiting waste as the vaccine solutions have a shelf-life of around four hours after opening. Keeping the vaccine cold to limit waste helped to cut down the cost of the vaccine and increase affordability [ 26 ]. Strong coordination was needed between the mobile clinics’ team and government agencies to monitor and regulate the deployment of vaccines once they were removed from cold storage [ 8 ]. The other aspect that was required to be regulated at this scale was the direct and indirect costs of providing a robust infrastructure, including arrangements for transporting elderly and disabled people, and creating awareness in the population of the critical importance of getting the second dose [ 27 ].
Replicability
Replicability of the mobile clinic model is also one more way to guarantee a faster and higher coverage of target population immunization. This would include clear and transparent communication on the part of government agencies regarding dedicated timelines, prioritization of the groups to be vaccinated first, the types of vaccine, and the vaccination schedules [ 28 ]. Training accredited social health activists, doctors, data operators, and other directly involved workers are also part of the replicability strategy. Common aspects of such strategies include developing awareness and vaccination knowledge, acquiring the means to engage the community through open-sourcing strategic partnerships with influential local leaders to build confidence and trust for the medical community regarding the safety of the vaccine, preventing the spread of misinformation and rumors, and making vaccines available in hard-to-reach places [ 29 ]. Programs like mobile clinics can be replicated if government agencies are familiar with social franchising, subcontracting, and branching out to develop the necessary infrastructure [ 30 ]. Such healthcare-oriented interventions can help achieve a higher percentage of vaccination in the general population. Another strategy that can be employed if necessary in resource-constrained areas is to obtain support through public-private partnerships (PPP), not just for the COVID-19 vaccination program but also for other public healthcare initiatives [ 31 ].
- Sustainability
The main objective of mobile clinics is to create sustainability for long-term impact. Sustainable funding for vaccines and vaccination programs comprises distribution costs, administrative expenses, surveillance, record keeping, and other needs [ 1 ]. Government agencies, the World Bank, and other multilateral banks have allocated extensive resources to achieve vaccination targets worldwide [ 32 ]. However, such financial support for the mobile clinic model should also have an element of internal rate of return and a sustainable cash flow [ 33 ]. Participation of government, private companies, and non-profit organizations has inculcated trust among the general population regarding the vaccine’s efficacy, safety, and affordability. This aspect of social sustainability is achieved through tailor-made strategies to reassure the local population regarding vaccine safety [ 34 ]. Technological assistance is one way to generate engineering sustainability to facilitate a mechanism to control pollution, recycle and reduce waste. A robust data system to check vaccine storage infrastructure, immunization schedules, and other logistics-related matters has enhanced the accountability of mobile clinics and established them as effective vaccination instruments [ 35 ]. Maximum transparency and communication between stakeholders are indispensable for a successful immunization program. Seamless coordination between these parties can aid in project management sustainability, not just at the local level but also at the national level; vaccine roll-out can be tracked, monitored, and evaluated, which helps in formulating efficient campaigns for creating awareness regarding vaccination importance [ 36 ]. Additionally, a robust data infrastructure cannot exist without isolated resources and environmental sustainability. Such data is necessary to identify the individuals eligible for priority vaccinations, create awareness, arrange transportation, and ensure that beneficiaries get the second dose [ 37 ]. The innovative methods adopted helped to coordinate the central pool of vaccine distribution with the local vaccination locations. Such a network ensured the efficient distribution of vaccines with limited wastage after they were removed from cold storage [ 38 ].
Theoretical framework and development of hypotheses
The following hypotheses have been developed based on the theoretical background described in the previous sub-sections to develop a theoretical foundation for this study. The research hypotheses were designed to demonstrate the relationship between the various constructs used in this study. Figure 1 illustrates the structural model for validating the three research hypotheses designed to evaluate the direct relationship between scalability, affordability, and replicability with immunization performance and sustainability.
H 1 . Scalability positively influences immunization performance.
H 2 . Scalability positively influences sustainability.
H 3 . Affordability positively influences immunization performance.
H 4 . Affordability positively influences sustainability.
H 5 . Replicability positively influences immunization performance.
H 6 . Replicability positively influences sustainability.
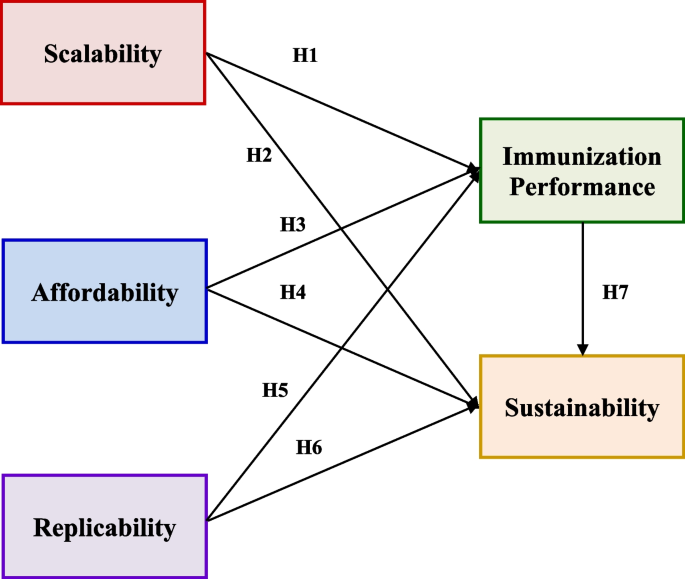
Conceptual model for empirical testing
Case organization
In the context of mobile clinics in India, the study has considered Jivika Healthcare’s VaccineOnWheels (VOW) as the primary case organization. To develop an operational framework for MMUs by defining the components and analyzing their impacts on immunization performance as the primary healthcare outcome [ 39 ] and sustainability, the Bill & Melinda Gates Foundation, Jivika Healthcare Ltd, and the Indian Institute of Technology Delhi partnered to conduct this research. In this regard, Jivika Healthcare's service innovation VaccineOnWheels (VOW) has been regarded as one of several businesses providing immunization services through mobile clinics. In 2019, Jivika Healthcare Private Limited, in partnership with the Indian Institute of Technology Hyderabad and the Bill & Melinda Gates Foundation, launched Vaccine on Wheels, India's doctor-based mobile vaccination clinic with the objective of “ensuring access to quality vaccination for all” through the following three goals:
to reduce "inequitable access" to vaccines and increase immunization reach
to reduce the vaccine cost by cutting down out-of-pocket expenses, including travel and missed wages
to create awareness of the critical importance of immunization
Jivika's mobile vaccination unit provide ‘doorstep’ service to underserved communities hard-to-reach areas with access to COVID-19 vaccines and up-to-date information regarding vaccine safety and efficacy. To “meet communities where they are,” mobile vaccine units and staff conduct vaccination awareness camps among the community to mitigate the impact of misinformation regarding vaccination effects. In 2019, mobile clinics began mobile vaccination service in Maharashtra’s Pune city. In recent times, the mobile clinic service has been spread across six states of India. Under public-private partnership (PPP), with the support of governments, corporate social responsibility (CSR), and non-profit government organizations (NGOs), the core idea of a mobile clinic “reaching the unreached” grew rapidly. VOW provides sufficient grounds to understand the operational model of a mobile clinic to create a transformative force to increase immunization based upon collaboration with various stakeholders, processes adopted, and strategies implemented during the immunization drive.
This program helped to understand the gaps in the vaccine delivery model from close quarters and identify various issues faced by diverse stakeholders, primarily infants/caregivers/parents, in getting vaccinated. VOW has made vaccines accessible to the elderly, individuals with disabilities, female sex workers, tribal communities, rural communities, street vendors, maids, slum residents, frontline workers, the bedridden, and school children, among other vulnerable segments of society. They have also provided at-home service for those who could not get to the vaccination center, especially persons with disabilities. They have served the people residing in remote locations of the six states through more than 200 mobile vaccination units. Under the unique framework of the PPP, vaccination was administered at a reduced cost for beneficiaries with vaccines provided by the government. The PPP model enables stakeholder collaboration across industries under CSR, government, and NGOs to share a commitment to making vaccination services available even at the grass-roots level. This initiative should help India achieve higher immunization penetration by getting faster acceptance of vaccination, providing convenience, and reducing the cost of service with zero travel cost, travel time, and lost wages.
Research instrument
The questionnaire was developed with the literature review on the factors identified and the significant input from a diverse team of healthcare professionals, including public health experts and academic researchers who have extensive experience in the field of healthcare delivery and MMUs. Their practical insights and hands-on experience were invaluable in formulating relevant and context-specific questions. Given the unique operational environment of MMUs and the specific healthcare needs of rural, tribal, and underprivileged populations in India, we deemed it crucial to tailor the questionnaire to these specific contexts. The expertise of the involved professionals ensured that the questions were both relevant and comprehensive, covering critical aspects of scalability, affordability, replicability, and sustainability.
Questionnaire development began with the identification of the factors to be measured, followed by the selection of items to assess those factors, and then the testing and refinement of the items. The questionnaire items include five significant features derived from the literature linked with mobile clinics: scalability, affordability, replicability, sustainability, and immunization performance. Before distribution to respondents, a team of health professionals and academic researchers evaluated the questionnaire. The questionnaire contained six sub-factors for scalability, three to describe affordability, four to define replicability, and two to define sustainability. To factorize the broad characteristics of mobile clinics, eighteen, nine, twelve, six, and four items were proposed to structure scalability, affordability, replicability, and sustainability, respectively. An example of a statement from the questionnaire describing the scalability of the mobile clinics’ delivery system is “Mobile clinics reply quickly to vaccination-related questions from beneficiaries.”
Respondents to a questionnaire were directed to make appropriate selections ranging from 1 (strongly disagree) to 5 (strongly agree) for each item. A Likert scale ranging from strongly disagree (1) to strongly agree (5) has been utilized to simplify the response to the forty-nine questionnaire items. Various studies have adopted similar empirical techniques for health and policy-related research [ 40 , 41 ].
Statistical analysis
Numerous research studies in health and policy sectors utilize empirical methods including PLS-SEM and Covariance-based SEM (CB-SEM) [ 40 , 41 ]. While each method has distinct goals and applications, they can be seen as complementary [ 42 ]. In the realm of public health, PLS-SEM is more apt than CB-SEM for identifying relationships between key influencing factors [ 43 ]. The PLS-SEM technique has become increasingly popular across various disciplines due to its ability to calculate path coefficients, handle latent variables in non-normal distributions, and process data with modest sample sizes [ 44 , 45 ]. The research model in this study was examined using the Partial Least Square Structured Equation Modeling (PLS-SEM) method [ 46 ]. This study employed Smart PLS 4.0, a renowned tool for PLS-SEM evaluations. The PLS method, using the Smart-PLS 4.0 software, explored the causal connections among constructs. Given the study's explorative nature, the PLS approach has been adopted. Following the recommendations of Henseler et al. (2009), a two-phase data analysis method was adopted [ 47 ]. Initially, the measurement model was evaluated, followed by an exploration of the latent constructs' interrelationships. This two-phase approach ensures the reliability and validity of measurements before delving into the model's structural dynamics [ 48 ].
Sampling technique
According to the standard method for determining sample size in PLS-SEM studies, the model structure should have at least 10 times the number of structural routes [ 49 , 50 ]. There's a notable relationship between sample size and statistical power. For a model with five external variables, a minimum of 169 respondents is recommended to achieve 80% statistical power at a 5% significance level [ 51 , 52 ]. The study ensured to meet the mentioned criteria.
Participants and procedures
The questionnaire assessed mobile clinics' scalability, affordability, replicability, immunization performance, and sustainability. The target respondents for this study were healthcare stakeholders, including health officers, grassroots workers, mobile clinic operators, NGOs, policymakers, and other support staff.
Initially, the questionnaire was tested in a pilot study with a small group of healthcare stakeholders before it was finalized. Feedback from the pilot study was used to make any necessary revisions to the questionnaire. Then, the data was acquired from 207 respondents from the states of Jharkhand, Maharashtra, Meghalaya, Karnataka, Telangana, and Tamil Nadu, directly involved in a mobile clinic vaccination campaign. The respondents occupied a variety of roles within the healthcare system. The states were chosen to collect data since VOW only operated in these states.
The survey was conducted using a self-administered paper-based survey, which lasted for around two months. Participants received the questionnaire in English language and were provided with the detailed explanation of the survey's purpose and instructions on how to complete it. The participants were selected based on their professional roles and expertise in the healthcare sector, specifically those with experience in MMUs or similar healthcare delivery models. This selection criterion ensured that respondents had the necessary knowledge and expertise to answer the questions accurately.
An exploratory factor analysis (EFA) followed by a confirmatory factor analysis (CFA) was used to structure the critical factors of mobile clinics for optimal immunization performance and sustainability. This study employed a survey-based methodology to conduct proper statistical analyses to determine and validate the success factors of mobile clinics.
Respondents’ profiles
The respondents included mobile clinic healthcare workers, support employees, and consulting partners associated with mobile clinics (VOW). To better understand the nature of respondents, we classified them into different demographic profiles to interpret their contribution in terms of gender distribution, states, and geography (Refer Table 1 ). The number of female respondents was only marginally higher than that of male ones, with the female percentage at 51.21% and the male percentage at 48.79%. This shows a great degree of gender equitability in India’s fight against the COVID-19 pandemic, a remarkable sign of equality. Telangana had the highest number of responses (47.34%), followed by Maharashtra (29.5%), showing a non-uniform trend, with the other states being much lower. Thus, the state-wise distribution was governed by the severity of the pandemic showing drastic differences in percentage.
EFA Results
EFA was used as a first stage in the factorization process to extract a factor structure that ensures conceptual significance to the overall study. The initial sample of 100 responses was considered for exercising the EFA. The factor accounting for the most significant common variance was deleted during factor extraction. The Kaiser-Meyer- Olkin (KMO) test was used to ensure data sufficiency for the EFA. The KMO value from the analysis was 0.837, which is considered meritorious by various studies. EFA was carried out using principal component analysis as the extraction method and Varimax rotation as the rotation method. During the EFA procedure, the cross-loading items were deleted iteratively to increase the reliability parameters and obtain a perfect set of factors. Twelve items were deleted throughout this iterative procedure, yielding five factors with eigenvalues greater than one. Table 2 shows the extracted factors and associated items from EFA.
CFA Results
The analysis was carried out to evaluate the derived measurement model using IBM SPSS AMOS 26 [ 53 ]. To begin, Cronbach’s alpha (α) and composite reliability (CR) were used to evaluate internal consistency reliability. The values of α for all obtained factors were more significant than 0.8, while those linked with CR were greater than 0.8. Both α and CR values indicate commendable fit, which implies that they are more significant than the acceptable threshold of 0.7 for all factors [ 52 ], which means that the internal consistency reliability is satisfactory. The outer loadings and average variance extracted (AVE) were examined to assess convergent validity. The outside loading values were ≥ 0.7, whereas the AVEs values were more significant than 0.5. [ 54 ]. Thus, convergent validity of the factors was ensured by these findings. Table 3 displays the extracted values for the three outer loadings, Cronbach’s alpha, composite reliability, and average variance.
It was observed that the CFA measurement model fitted the data effectively. Comparative fit index (CFI), standardized root mean square residual (SRMR), and root mean square error of approximation (RMSEA) were calculated to be 0.96, 0.0503, and 0.035, respectively. Detailed information is provided in Table 4 .
In addition, discriminant validity was evaluated using the Heterotrait-monotrait ratio (HTMT), as shown in Table 5 . Based on these findings, it is apparent that the discriminant validity of the components in the proposed model was significantly validated by the HTMT standards [ 54 ].
Path model assessment
The model developed in the paper illustrates six critical hypotheses regarding the influence of scalability, affordability, and replicability on immunization performance and sustainability. Moreover, the model demonstrates the hypothesized link between immunization performance and sustainability. For the empirical validation of the model, the gathered data were utilized to examine the hypothesized correlations. Using SmartPLS 4.0 software, the model was empirically validated (Refer Fig. 2 ). Table 6 displays the results obtained by analyzing the structural model. All factors (SAR) were discovered to impact immunization performance substantially. While examining the direct effect of independent factors (SAR) on sustainability, it was observed that only affordability positively affected sustainability. It was also noticeable from the tested model that there was a significant path from immunization performance to sustainability. It is evident from Table 6 that the model has been validated and that several significant hypotheses were supported. The model also revealed an SRMR value of 0.053, indicating a satisfactory model fit. Analysis reveals that the R-squared values for immunization performance and sustainability were 0.494 and 0.290, respectively.
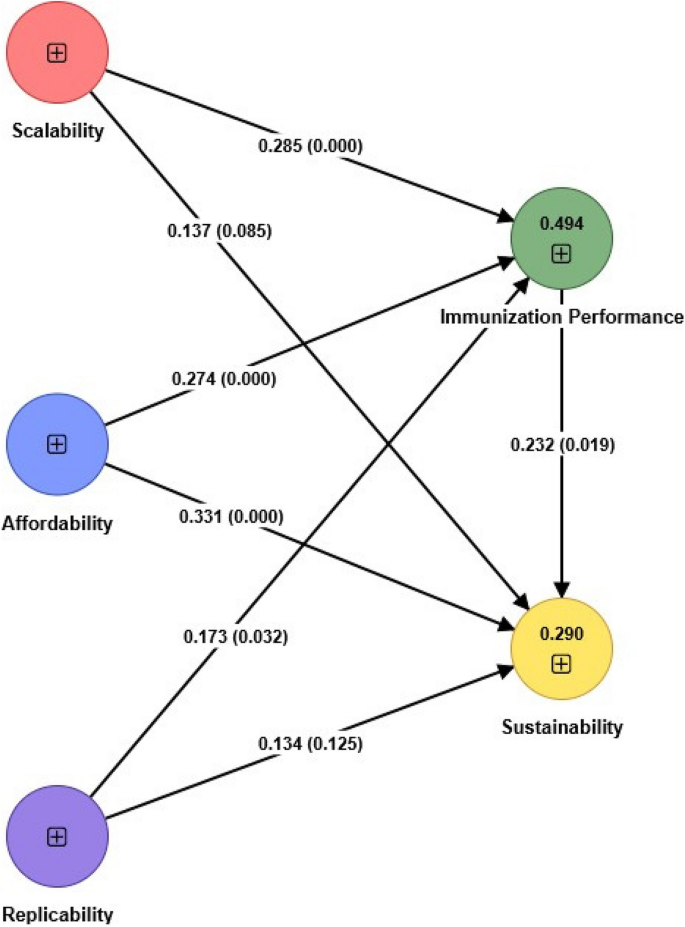
Empirical validation of the model
In general, all significant relationships have values ranging from 0.17 to 0.33. Regarding the effect of independent factors on immunization performance, all three factors (SAR) have a substantial direct effect. Scalability and replicability were found to have a more substantial influence on immunization performance than affordability. The effect (β) values presented for hypotheses H 1 and H 5 are 0.28 and 0.33, respectively.
The β value of affordability on immunization performance (H 3 ) was 0.274. Comparing all three hypothesized links revealed that replicability had the most significant impact, followed by scalability and affordability. Similarly, when investigating the direct relationship between independent factors (SAR) and the sustainability of mobile clinics, the reported β value for the only significant influence of affordability was 0.173. In addition, the hypothesized pathway between immunization performance and sustainability was observed, providing evidence for the association. The reported β value for the relationship between immunization performance and mobile clinics’ sustainability was 0.232. Table 6 provides information regarding the validation of hypothesized linkages.
Equitable access to healthcare and immunizations is crucial for promoting public health, particularly in underserved rural and tribal areas. Mobile Medical Units (MMUs) represent a valuable community-based service delivery approach to address healthcare disparities in both urban and rural settings. While MMUs have been recognized as essential providers of medical care, their full potential and effectiveness have not been comprehensively explored in previous studies. This empirical study was conducted to shed light on the critical factors influencing the effectiveness and sustainability of mobile clinics for immunization programs.
The primary objective of this study was to discern the critical components of the operational model for MMUs and assess their impact on immunization performance and the sustainability of the model within the context of primary healthcare. For this purpose, a quantitative analysis assessed the five key factors: scalability, affordability, replicability, immunization performance, and sustainability. By employing structural equation modeling, the direct effects of these factors were examined. We aimed to construct a framework of guidelines that could enhance healthcare coverage in developing countries, specifically focusing on developing countries like India. The findings directly address the research objectives by elucidating the relationships among scalability, affordability, replicability, immunization performance, and sustainability of the MMUs operational model. In support of RO1, the results showcased that scalability, affordability, and replicability (SAR) significantly influence immunization performance, with replicability having the most substantial impact. Furthermore, immunization performance has a direct effect on the sustainability of MMUs, underscoring its crucial role. These findings collectively inform the development of a comprehensive framework for MMUs, as outlined in RO2. This framework emphasizes that to achieve sustainable primary healthcare innovations, MMUs must prioritize enhancing immunization performance through scalable, affordable, and replicable models. By directly linking these empirical findings to our research objectives, we provide actionable insights for policymakers and healthcare professionals.
Our empirical findings have yielded valuable insights into the factors contributing to mobile clinics' successful operation in India. Scalability primarily hinges on a well-defined delivery system, technical support, organizational capability, partnerships, integration, and community engagement. Affordability is closely linked to factors such as the procurement and distribution of vaccines, cold storage infrastructure, waste management, and managing both direct and indirect costs. Replicability, however, depends on open-sourcing training, strategic collaboration, and capacity building.
In the sustainability domain, a significant emphasis was placed on developing an ecosystem that supports the enduring presence of mobile clinics. This involves effective management strategies that ensure both social and project sustainability. This includes securing funding for vaccines, equipment, maintenance, and staff salaries, establishing strategic partnerships with local stakeholders, raising public awareness about immunization programs, and ensuring equitable access to quality immunization services for all, regardless of socioeconomic status or geographical location.
During the factorization process, it became evident that the delivery system is pivotal in determining scalability. Successful mobile clinics must implement standard operating procedures, maintain effective communication and data management systems, and possess a well-trained workforce capable of allocating resources efficiently to meet the diverse needs of their communities.
Similarly, in terms of affordability, cold storage and waste management emerged as the key factors. Ensuring that vaccines are stored at the appropriate temperature during transportation, particularly in remote areas, is essential for cost-effectiveness and minimizing dose wastage in immunization programs.
In the context of replicability, capacity building was identified as the strongest indicator. Building the competence of mobile clinic teams, which include nurse practitioners, physicians, public health workers, and other healthcare professionals, is critical for agile and effective vaccine delivery. Proper training and adherence to best practices are essential for success.
Lastly, when examining the 'sustainability' factor, it became evident that creating an ecosystem conducive to the long-term operation of mobile clinics is vital. This involves continuous monitoring, sound financial planning, strategic partnerships, public awareness campaigns, and a commitment to equitable service provision.
Considering the overall model, the validated framework highlights the significance of scalability, affordability, and replicability in improving immunization performance. However, while affordability significantly impacts sustainability, the other factors appear to have no direct influence. Nevertheless, a strong link exists between immunization performance and the sustainability of mobile clinics. Affordable mobile clinics are more likely to be utilized, resulting in improved immunization rates and greater sustainability due to increased demand. Furthermore, the scalability and replicability of mobile clinics enables them to adapt to various contexts, which encourages broader adoption and, consequently, enhances their long-term sustainability. This study underscores the vitality of these factors in optimizing the impact of mobile clinics in advancing public health goals.
Previous studies have highlighted the challenges and benefits of scaling up healthcare interventions and replicating successful models in different settings. Our study builds on this body of work by empirically demonstrating that while scalability and replicability do not have a direct effect on sustainability, they significantly influence immunization performance, which in turn impacts sustainability. This finding adds a nuanced understanding of the indirect pathways through which these factors contribute to sustainable healthcare systems.
Affordability has consistently been recognized as a critical factor in healthcare delivery, particularly in resource-constrained settings. Our results corroborate this by showing that affordability significantly impacts immunization performance, thus reinforcing the need for cost-effective healthcare solutions. This aligns with existing literature that emphasizes the importance of economic feasibility in healthcare interventions.
This study confirms the pivotal role of immunization performance in achieving sustainability, consistent with prior research that underscores the importance of effective immunization programs for long-term health outcomes. By linking immunization performance directly to sustainability, our findings provide empirical support for strategies aimed at enhancing immunization coverage as a pathway to sustainable healthcare.
The healthcare challenges addressed in this study, such as equitable access to healthcare for rural, tribal, and underprivileged populations, are not unique to India. Many developing countries face similar issues, making the findings of this study potentially applicable to other contexts. The operational model of MMUs evaluated in this study can serve as a reference for other developing countries looking to implement or enhance similar healthcare interventions.
The concept of scalability, as evaluated in this study, involves expanding healthcare interventions while maintaining effectiveness and efficiency. This aspect is crucial for developing countries with large rural populations and limited healthcare infrastructure. Affordability is a significant consideration in many developing countries where economic constraints limit access to healthcare services. The insights from this study on making MMUs cost-effective can guide policymakers in similar settings. The ability to replicate successful healthcare interventions in different settings is vital for broader implementation. The findings of this study on the replicability of MMUs can inform strategies in other developing countries to achieve consistent healthcare outcomes. Ensuring the long-term sustainability of healthcare interventions is a common challenge across developing nations. The study's findings on the sustainability of MMUs provide a framework for integrating such models into existing health systems for lasting impact.
Research on improving the sustainability of MMUs has not received much attention in developing countries and has also been recognized as a prominent gap in the past literature [ 10 ]. This study recognized that MMUs have the capability to engage and win underprivileged people’s trust by driving directly into communities and opening their doors on the steps of their target beneficiaries. Services offered by MMUs have been proven to enhance immunization coverage and individual health outcomes, advance community health, and lower healthcare costs compared with typical clinical settings because MMUs can overcome numerous healthcare barriers. MMUs can operate as significant players in our developing healthcare system since they can address social, behavioral, and medical health challenges and act as a bridge between the physical clinics and the community. Continuous research must be conducted to resolve the problems and enhance the capacity of MMUs, strengthen the cost-effectiveness of MMUs services, and explore both qualitative and quantitative evidence to advocate for more widespread integration of MMUs into the public health ecosystem to tackle some of the most significant challenges facing primary healthcare services in the current day.
The study examined the impact of scalability, affordability, and replicability on immunization performance and further the effect of immunization performance on the sustainability of the MMUs operation model in the future. While the initiative applies to all regions, it benefited Tier-II, rural, and tribal communities. The mobile vaccination program aims to reach and vaccinate people in hard-to-reach locations. In this way, the program had firmly established itself in urban catchment areas, rural and tribal communities. Finally, a similar model is believed to be replicated in other distant and underprivileged regions of India where healthcare services are lacking. For future routine immunization programs and other primary healthcare services in rural and tribal areas, a similar strategy can be implemented.
Additionally, this study has several limitations that should be acknowledged. The operational model of MMUs might vary significantly across different regions and settings. The study’s findings on scalability, affordability, and replicability may therefore need contextual adaptation when applied to different healthcare environments. Also, the data were collected from healthcare professionals in six states of India, which may not fully represent the diversity of healthcare settings across the entire country. Consequently, the findings may not be entirely generalizable to other regions within India or to other countries with different healthcare contexts.
Implications and future research avenues
MMUs have been recognized as a transformative intervention towards equitable access to health care and the achievement of universal health coverage in developing countries like India. MMUs can be efficient alternatives for delivering quality healthcare to the most vulnerable populations and improving the early diagnosis of various diseases. Practically, this study equips policymakers and public health professionals with the critical components of the MMUs operational model leading toward sustainability. The research framework provides reliable grounds for examining the impact of scalability, affordability, and replicability on immunization coverage as the primary public healthcare outcome. The model can be employed in planning and developing an ecosystem of MMUs for underserved populations and integrating MMUs into the public health structure of a developing country. The model can also be utilized as a management tool for monitoring and assessment of various interventions to be introduced along with MMUs in the future. Practitioners can assess the scalability and affordability of their interventions and improve their decision-making by examining the impact on sustainability.
Our study has primarily identified the impact of scalability, affordability, and replicability on immunization performance, but the model could be extended by examining how the technological readiness of MMUs influences their sustainability. Also, future researchers could explore other public health outcomes and measure the overall impact of scalability, affordability, and replicability on public health in general. In addition, it has been suggested that future researchers utilize a multiple case study approach to examine the impact of the critical components of MMU operation by generating evidence from more than one case organization and covering a wider range of geographies in India.
Availability of data and materials
Not applicable
Abbreviations
- Mobile medical units
Scalability, affordability, replicability
Partial least squares structural equation modeling
VaccineOnWheels
Coronavirus Disease 2019
Public-private partnership
Non-profit government organizations
Corporate social responsibility
Covariance based structural equation modeling
Exploratory factor analysis
Kaiser-Meyer-Olkin
Confirmatory factor analysis
Composite reliability
Average variance extracted
Comparative fit index
Standardized root mean square residual
Heterotrait-monotrait ratio
Root mean square error of approximation
Effect value
Amimo F, Lambert B, Magit A, Hashizume M. A review of prospective pathways and impacts of COVID-19 on the accessibility, safety, quality, and affordability of essential medicines and vaccines for universal health coverage in Africa. Globalization health. 2021;17(1):1–5.
Article Google Scholar
Ho CJ, Khalid H, Skead K, Wong J. The politics of universal health coverage. Lancet. 2022.
Dar M, Moyer W, Dunbar-Hester A, Gunn R, Afokpa V, Federoff N, Brown M, Dave J. Supporting the most vulnerable: Covid-19 vaccination targeting and logistical challenges for the homebound population. NEJM Catalyst Innovations Care Delivery. 2021;2(5). https://catalyst.nejm.org/doi/full/10.1056/CAT.21.0117 .
Kumar A, Nayar KR, Koya SF. COVID-19: Challenges and its consequences for rural health care in India. Public Health Pract. 2020;1:100009.
Das P, Shukla S, Bhagwat A, Purohit S, Dhir S, Jandu HS, Kukreja M, Kothari N, Sharma S, Das S, Taneja G. Modeling a COVID-19 vaccination campaign in the State of Madhya Pradesh, India. Global J Flex Syst Manage. 2023;24(1):143–61.
Dhawan V, Aggarwal MK, Dhalaria P, Kharb P, Sharma D, Dinesh KK, Dhir S, Taneja G, Ghosh RS. Examining the Impact of Key Factors on COVID-19 Vaccination Coverage in India: A PLS-SEM Approach. Vaccines. 2023;11(4):868.
Article PubMed PubMed Central Google Scholar
Stamm A, Strupat C, Hornidge AK. Global access to COVID-19 vaccines: Challenges in production, affordability, distribution and utilisation. Discussion Paper; 2021.
Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397(10278):1023–34.
Article PubMed PubMed Central CAS Google Scholar
Mishra V, Seyedzenouzi G, Almohtadi A, Chowdhury T, Khashkhusha A, Axiaq A, Wong WY, Harky A. Health inequalities during COVID-19 and their effects on morbidity and mortality. J Healthc Leadersh. 2021:19–26.
Khanna AB, Narula SA. Mobile health units: mobilizing healthcare to reach unreachable. Int J Healthc Manag. 2016;9(1):58–66.
Chanda S, Randhawa S, Bambrah HS, Fernandes T, Dogra V, Hegde S. Bridging the gaps in health service delivery for truck drivers of India through mobile medical units. Indian J Occup Environ Med. 2020;24(2):84.
Dwivedi YK, Shareef MA, Simintiras AC, Lal B, Weerakkody V. A generalised adoption model for services: A cross-country comparison of mobile health (m-health). Government Inform Q. 2016;33(1):174–87.
Akhtar MH, Ramkumar J. Primary Health Center: Can it be made mobile for efficient healthcare services for hard to reach population? A state-of-the-art review. Discover Health Syst. 2023;2(1):3.
Patel V, Parikh R, Nandraj S, Balasubramaniam P, Narayan K, Paul VK, Kumar AS, Chatterjee M, Reddy KS. Assuring health coverage for all in India. Lancet. 2015;386(10011):2422–35.
Article PubMed Google Scholar
Attipoe-Dorcoo S, Delgado R, Gupta A, Bennet J, Oriol NE, Jain SH. Mobile health clinic model in the COVID-19 pandemic: lessons learned and opportunities for policy changes and innovation. Int J Equity Health. 2020;19(1):1–5.
Chillimuntha AK, Thakor KR. Disadvantaged rural health–issues and challenges: a review. Natl J Med Res. 2013;3(01):80–2.
Google Scholar
Landis-Lewis Z, Flynn A, Janda A, Shah N. A scalable service to improve health care quality through precision audit and feedback: proposal for a randomized controlled trial. JMIR Res Protocols. 2022;11(5):e34990.
Liu A, Sullivan S, Khan M, Sachs S, Singh P. Community health workers in global health: scale and scalability. Mt Sinai J Medicine: J Translational Personalized Med. 2011;78(3):419–35.
Azizatunnisa L, Cintyamena U, Mahendradhata Y, Ahmad RA. Ensuring sustainability of polio immunization in health system transition: lessons from the polio eradication initiative in Indonesia. BMC Public Health. 2021;21(1):1–6.
Cintyamena U, Azizatunnisa L, Ahmad RA, Mahendradhata Y. Scaling up public health interventions: case study of the polio immunization program in Indonesia. BMC Public Health. 2021;21(1):1–2.
English SW, Barrett KM, Freeman WD, Demaerschalk BM. Telemedicine-enabled ambulances and mobile stroke units for prehospital stroke management. J Telemed Telecare. 2022;28(6):458–63.
Ganapathy K, Reddy S. Technology enabled remote healthcare in public private partnership mode: A story from India. Telemedicine, Telehealth and Telepresence: Principles, Strategies, Applications, and New Directions. 2021:197–233.
Lin SC, Zhen A, Zamora-Gonzalez A, Hernández J, Fiala S, Duldulao A. Research Brief Report: Variation in State COVID-19 Disease Reporting Forms on Social Identity, Social Needs, and Vaccination Status. J Public Health Manage Pract. 2022;28(5):486.
Pegurri E, Fox-Rushby JA, Damian W. The effects and costs of expanding the coverage of immunisation services in developing countries: a systematic literature review. Vaccine. 2005;23(13):1624–35.
Levine DM, Chalasani R, Linder JA, Landon BE. Association of the Patient Protection and Affordable Care Act with ambulatory quality, patient experience, utilization, and cost, 2014–2016. JAMA Netw open. 2022;5(6):e2218167.
Sharma P, Pardeshi G. Rollout of COVID-19 vaccination in India: a SWOT analysis. Disaster Med Pub Health Prep. 2022;16(6):2310–3.
Epstein S, Ayers K, Swenor BK. COVID-19 vaccine prioritisation for people with disabilities. Lancet Public Health. 2021;6(6):e361.
Merritt L, Fennie K, Booher J, Fulcher O, Carretta J. Community-led effort to Reduce Disparities in COVID Vaccination: A Replicable Model. J Natl Med Assoc. 2021;114(3):S38. https://doi.org/10.1016/j.jnma.2021.08.014 .
Chadambuka A, Chimusoro A, Apollo T, Tshimanga M, Namusisi O, Luman ET. The need for innovative strategies to improve immunisation services in rural Zimbabwe. Disasters. 2012;36(1):161–73.
Kumar VM, Pandi-Perumal SR, Trakht I, Thyagarajan SP. Strategy for COVID-19 vaccination in India: the country with the second highest population and number of cases. npj Vaccines. 2021;6(1):60.
Baig MB, Panda B, Das JK, Chauhan AS. Is public private partnership an effective alternative to government in the provision of primary health care? A case study in Odisha. J Health Manage. 2014;16(1):41–52.
Skolnik A, Bhatti A, Larson A, Mitrovich R. Silent consequences of COVID-19: why it’s critical to recover routine vaccination rates through equitable vaccine policies and practices. Annals Family Med. 2021;19(6):527–31.
Oriol NE, Cote PJ, Vavasis AP, Bennet J, DeLorenzo D, Blanc P, Kohane I. Calculating the return on investment of mobile healthcare. BMC Med. 2009;7(1):1–6.
Mukherjee S, Baral MM, Chittipaka V, Pal SK, Nagariya R. Investigating sustainable development for the COVID-19 vaccine supply chain: a structural equation modelling approach. J Humanitarian Logistics Supply Chain Manage. 2022.
Christie A, Brooks JT, Hicks LA, Sauber-Schatz EK, Yoder JS, Honein MA, Team COVIDC. Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage. Morb Mortal Wkly Rep. 2021;70(30):1044.
Article CAS Google Scholar
Pilati F, Tronconi R, Nollo G, Heragu SS, Zerzer F. Digital twin of COVID-19 mass vaccination centers. Sustainability. 2021;13(13):7396.
Russo AG, Decarli A, Valsecchi MG. Strategy to identify priority groups for COVID-19 vaccination: A population based cohort study. Vaccine. 2021;39(18):2517–25.
Kimble C, Coustasse A, Maxik K. Considerations on the distribution and administration of the new COVID-19 vaccines. Int J Healthc Manag. 2021;14(1):306–10.
Kress DH, Su Y, Wang H. Assessment of primary health care system performance in Nigeria: using the primary health care performance indicator conceptual framework. Health Syst Reform. 2016;2(4):302–18.
Park K, Park J, Kwon YD, Kang Y, Noh JW. Public satisfaction with the healthcare system performance in South Korea: Universal healthcare system. Health Policy. 2016;120(6):621–9.
Hald AN, Bech M, Burau V. Conditions for successful interprofessional collaboration in integrated care–lessons from a primary care setting in Denmark. Health Policy. 2021;125(4):474–81.
Hair JF, Ringle CM, Sarstedt M. Partial least squares structural equation modeling: Rigorous applications, better results and higher acceptance. Long Range Plann. 2013;46(1–2):1–2.
Ali F, Omar R. Determinants of customer experience and resulting satisfaction and revisit intentions: PLS-SEM approach towards Malaysian resort hotels. Asia-Pacific J Innov Hospitality Tourism (APJIHT). 2014;3:1–9.
Henseler J, Dijkstra TK, Sarstedt M, Ringle CM, Diamantopoulos A, Straub DW, Ketchen DJ Jr, Hair JF, Hult GT, Calantone RJ. Common beliefs and reality about PLS: Comments on Rönkkö and Evermann (2013). Organizational Research Methods. 2014;17(2):182–209.
Rigdon EE. Rethinking partial least squares path modeling: breaking chains and forging ahead. Long Range Plann. 2014;47(3):161–7.
Hair JF, Ringle CM, Sarstedt M. PLS-SEM: Indeed a silver bullet. J Mark theory Pract. 2011;19(2):139–52.
Henseler J, Ringle CM, Sinkovics RR. The use of partial least squares path modeling in international marketing. InNew challenges to international marketing 2009 Mar 6 (Vol. 20, pp. 277–319). Emerald Group Publishing Limited.
HUYUT M, Soygüder S. The multi-relationship structure between some symptoms and features seen during the new coronavirus 19 infection and the levels of anxiety and depression post-Covid. Eastern J Med. 2022;27(1):1–10.
Tabachnick BG, Fidell LS. Experimental designs using ANOVA. Belmont, CA: Thomson/Brooks/Cole; 2007. Dec 6.
Iantovics LB, Rotar C, Morar F. Survey on establishing the optimal number of factors in exploratory factor analysis applied to data mining. Wiley Interdisciplinary Reviews: Data Min Knowl Discovery. 2019;9(2):e1294.
Jung S. Exploratory factor analysis with small sample sizes: A comparison of three approaches. Behav Process. 2013;97:90–5.
Hair J Jr, Hair JF Jr, Hult GT, Ringle CM, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM). Sage; 2021.
Book Google Scholar
Hulland J. Use of partial least squares (PLS) in strategic management research: A review of four recent studies. Strateg Manag J. 1999;20(2):195–204.
Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci. 2015;43:115–35.
Download references
Acknowledgments
Not applicable.
This study has been funded by Bill and Melinda Gates Foundation (027027; RP04054F)
Author information
Authors and affiliations.
Jivika Healthcare Private Limited, Pune, Maharashtra, India
Jignesh Patel, Sangita More, Pravin Sohani & Shrinath Bedarkar
Jindal Global Business School, O. P. Jindal Global University, Haryana, India
Kamala Kannan Dinesh
Department of Management Studies, Indian Institute of Technology Delhi, Delhi, India
Deepika Sharma, Sanjay Dhir & Sushil Sushil
Bill & Melinda Gates Foundation, New Delhi, India
Gunjan Taneja
Public Health Consultant, New Delhi, India
Raj Shankar Ghosh
You can also search for this author in PubMed Google Scholar
Contributions
JP, SM, PS, SB, SD, SS, GT, and RG conceptualized the paper. KD, DS, SD, and SS collected and analyzed the data. KD and DS prepared the first draft of the manuscript, which was revised and edited by all other authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Deepika Sharma .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: annexure 1. profile of respondents based on their expertise., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Patel, J., More, S., Sohani, P. et al. Sustaining the mobile medical units to bring equity in healthcare: a PLS-SEM approach. Int J Equity Health 23 , 175 (2024). https://doi.org/10.1186/s12939-024-02260-x
Download citation
Received : 29 April 2023
Accepted : 26 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1186/s12939-024-02260-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care
- Immunization
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
- Oxford Thesis Collection
- CC0 version of this metadata
Integrated care in practice: a case study of health and social care for adults considered to be at high risk of hospital admission
Integrated care is pursued globally as a strategy to manage health and social care resources more effectively. It offers the promise of meeting increasingly complex needs, particularly those of aging populations, in a person-centred, co-ordinated way that addresses fragmentation and improves quality.
However, policy to integrate health and social care in England has led to programmes which have had disappointing effects on reducing hospital admissions and costs. My concern with the...
Email this record
Please enter the email address that the record information will be sent to.
Please add any additional information to be included within the email.
Cite this record
Chicago style, access document.
- HUGHES 2018 thesis.pdf ( Preview , pdf, 3.1MB, Terms of use )
Why is the content I wish to access not available via ORA?
Content may be unavailable for the following four reasons.
- Version unsuitable We have not obtained a suitable full-text for a given research output. See the versions advice for more information.
- Recently completed Sometimes content is held in ORA but is unavailable for a fixed period of time to comply with the policies and wishes of rights holders.
- Permissions All content made available in ORA should comply with relevant rights, such as copyright. See the copyright guide for more information.
- Clearance Some thesis volumes scanned as part of the digitisation scheme funded by Dr Leonard Polonsky are currently unavailable due to sensitive material or uncleared third-party copyright content. We are attempting to contact authors whose theses are affected.
Alternative access to the full-text
Request a copy.
We require your email address in order to let you know the outcome of your request.
Provide a statement outlining the basis of your request for the information of the author.
Please note any files released to you as part of your request are subject to the terms and conditions of use for the Oxford University Research Archive unless explicitly stated otherwise by the author.
Contributors
Bibliographic details, item description, terms of use, views and downloads.
If you are the owner of this record, you can report an update to it here: Report update to this record
Report an update
We require your email address in order to let you know the outcome of your enquiry.
Coronavirus (COVID-19) Updates For the latest information and advice see: Coronavirus (COVID-19) frequently asked questions

Scottish Graduate School of Social Science
Improving person-centred care communication in health and social care settings.

PHD STUDENT: Natalia Rodriguez UNIVERSITY: Heriot-Watt COMPANY: Healthcare Improvement Scotland
In January 2019 Healthcare Improvement Scotland welcomed Natalia Rodriguez to undertake a 3 month internship. Natalia is studying for a PhD with a focus on interpreting in mental healthcare settings at Heriot Watt University. During her time at Healthcare Improvement Scotland she worked within the Evidence and Evaluation for Improvement Team (EEvIT), supporting them to evaluate the ‘What Matters to You? Day’ (WMTY) initiative that is facilitated by the Person Centred Care Team. Natalia was happy to share information about her experience below.
"It has been an absolute joy working with Natalia. She has been a breath of fresh air. She picked it up quickly and I didn't feel that I had to direct her too much. I think we really lucked out on Natalia's skill set." Colleague from HIS
What attracted you to this internship?
When I first saw the advertisement for an internship position for PhD candidates with Healthcare Improvement Scotland (HIS) I was both thrilled and hesitant about applying. On paper, I was a good candidate, but I wondered if my academic background would be the right fit for the organisation. On the other hand, I was sure that it would be a great opportunity for me and that I definitely wanted to put my research skills to use in public healthcare.
My PhD had already given me the chance to witness the work of the NHS first-hand. For data collection purposes, I observed consultations conducted through spoken-language interpreters in two psychiatric wards within NHS Lothian for over a year. During this time, I not only collected data but also learnt lessons about human resilience that I will always carry with me. Having finished the data-collection work in December, I have now a year of funding left to convert my data into a thesis. So, the chance to work with HIS in this transition stage could not have come at a better time!
What did you do?
During my time at HIS, I supported the Evidence and Evaluation for Improvement Team (EEvIT). Specifically, I supported EEvIT to evaluate the ‘What matters to you? day’ initiative that is facilitated by the Person-Centred Care Team within HIS. For this purpose, I conducted primary and secondary research to produce an evidence report called: “‘What matters to you?’ Embedding the question in everyday practice: a multiple case-study”.
Did the internship meet your expectations?
It definitely exceeded my expectations. When I applied for the post, I was expecting that I would be doing some kind of work for a public health organisation, which in itself was to enough to make me feel excited. What I did not know then was that I would be applying my whole range of research skills to explore a topic fully in line with my PhD aims. I really was not expecting that before I started.
How did you utilise your research skills and knowledge during the internship?
There was clear common ground between my PhD topic and the aims of my internship project, which made it possible for me to use my knowledge and apply the research skills required to fulfil my internship aims. My PhD is about how linguistically and culturally diverse patients access healthcare services when they do not share a language with the service provider. During my internship, I evaluated the impact of a campaign that aims to promote a communication model in which patients and practitioners are encouraged to interact as equal partners in the planning of care. Methodologically speaking, for my PhD I have adopted a single case-study research design and for my internship, I adopted a multiple-case study design. In summary, my knowledge on the topic and the methodology required to explore was useful as a starting point, but the internship aims required me to take my expertise a step further.
How has it impacted your professional and personal development?
I am not sure about what type of work I will conduct after my PhD but public health and social care provision is definitely a research and personal interest that I am going to carry with me for life after my internship.
I do believe that my internship will help open up a new range of future possibilities that I would have never even thought about until now. The National Health Service is such a complex organisation that encompasses so many different departments, teams and staff with different backgrounds. Particularly, Healthcare Improvement Scotland contains different portfolios that have different objectives but pursue the common aim of driving improvement in the provision of health and social care services. This is an excellent area of work and definitely worth considering in the future.
Are there any outputs from the internship that you would like to share?
It was key for me to meet other people in the organisation outside from the team that I was allocated to work with as that provided me with unintended benefits. E.g. I was able to meet the Equality and Diversity advisor from HIS whose work is closely connected with my research interests and PhD aims. Because of his support, I was able to provide some feedback on a policy document draft around my area of expertise (healthcare interpreting) that will soon be published. That was not part of my internship aims but I definitely count that as one my main internship accomplishments.
What transferable skills did you learn?
Communicate clearly with a wide audience. During my internship I worked with a multidisciplinary team made up of health service researchers, a health economist and an information scientist. During data-collection, I interviewed people with a wide range of backgrounds including consultant, nurses, health service managers, etc. Developing appropriate timescales and sticking to them which was key to success as I was fully responsible for the development of the project. Being flexible: we had to consider different study designs as we depended on data availability.
How did you find coming back to your research after the internship?
I feel more confident now when approaching my PhD dataset. I did my internship during a transition time, right in between finishing data collection and starting data analysis and subsequent reporting. During my internship, I had to analyse and report data and that gave me a small-scale taster of what would come after. A team of health service researchers supported my work and provided guidance at all times so that I could fulfil my internship study aims. I am going to keep using that guidance to safeguard rigour in my own research work. I feel that I have more research tools and resources now.

What advice would you give other PhD students thinking about an internship?
1- Be more confident in their own potential contribution to the hosting organisation. I think that they might find it refreshing to work with someone new who brings a unique set of research skills to their organisation. 2- Remember that you do not need to know everything from the beginning as people want you to do well and will train you and you learn on the job 3- Your co-workers are engaged in their own routine so speak up if you need anything from them as they may not be used to having an intern. It is important to be self-directed (within limits and guidance)
Subscribe to our Newsletter

Privacy Policy
© 2023 All rights reserved
Scottish Graduate School of Social Science, proudly funded by

Give your feedback to help us improve our website This is the new Equality and Human Rights Commission website
On this page
Case study 1, case study 2, case study 3, health and social care case studies.
Published: 3 March 2016
Last updated: 3 March 2016
What countries does this apply to?
Increasing awareness of bowel cancer symptoms among the Asian Community –NHS Hillingdon Clinical Commissioning Group (Formerly NHS Hillingdon)
This case study illustrates the benefits of collecting and using equality information to identify the needs of people with particular protected characteristics and to measure progress in responding to those needs over time.
NHS Hillingdon Public Health Team looked at the information available on cancer types and rates in the Borough in 2010. They found that:
- Among cancers, bowel cancer accounted for a large proportion of cancer deaths;
- More people under 75 were dying of cancer in the South of the Borough which has a high Asian population compared to in the North;
- Cancer was a substantial contributor to inequality in death rates, particularly among women living in the most deprived 20 percent of the borough.
Cancer can often be successfully treated if detected early. For example, eight out of 10 cases of bowel cancer can be treated successfully if detected early .
Action taken
Based on the baseline data outlined above, the Public Health Team decided to launch an awareness campaign in the South of the Borough (Hayes and Harlington) which has a high Asian population.
The Public Health Team found that members of the Asian community had more limited awareness of the symptoms of bowel cancer, which was reducing the chances of early diagnosis with implications for survival rates. One of the reasons for this appeared to be that Asian people felt that cancer did not affect their family or their community (or was less likely to affect them).
In light of these findings, NHS Hillingdon focused their campaign on various actions to raise awareness of the symptoms of bowel cancer among the Asian community, particularly women. Those actions included:
- Designing and distributing leaflets about bowel cancer in English and in relevant Asian languages;
- Holding workshops, facilitated both in English and in other predominant languages. These were organised through existing local organisations e.g. women's groups or charities particularly targeting Asian communities or religious centres;
- Displaying campaign posters on buses and in tube stations in the Borough;
- Promoting messages by advertising on the Sunrise Radio Network - the UK's largest Asian radio network.
Surveys undertaken before and after the campaign revealed that awareness of the main symptoms of bowel cancer increased among people who had received information from the Public Health Team. Almost 80 percent of those who had seen or heard at least one element of the campaign could spontaneously recall at least one symptom, compared to less than 60 percent of those who had not been exposed to promotional material.
Advertising on the Sunrise Radio Network was found to be particularly successful in reaching Asian women.
Using equality information to reduce non-attendance at the Diabetic Eye Screening Programme - Royal Marsden NHS Foundation Trust
All people with diabetes are at risk of developing diabetic retinopathy. This is the most common cause of blindness in people of working age in the UK. There are usually no obvious symptoms until it is well advanced. Evidence shows that early detection and treatment can prevent sight loss. It is therefore very important that it is identified and treated as early as possible.
The Diabetic Eye Screening Programme (DESP) offers annual eye screening to people with diabetes. Data collected in 2011/2012[1] about patients who did not attend showed that the service had the highest non-attendance rate (21.2 percent) of all services delivered by Sutton and Merton community services.
Actions taken
A health equity audit was commissioned to look at equity of service provision, uptake and outcomes among patients referred to the DESP. The audit looked at whether there were differences between the non-attendance rates of people with particular protected characteristics, i.e. age, gender and ethnicity.
The audit concluded in late 2012. It showed that patients of working age were more likely to miss appointments compared with older age groups, and the highest non-attendance rate (40 percent) was found in the 22-31 age group.
To improve accessibility for patients of working age, the service has expanded its out-of-hours provision to include weekend clinics. It also offers patients the option to make and change their appointments by email so that busy patients no longer have to call during working hours to do this.
These initiatives have contributed to reducing the overall non-attendance rate for the DESP. It has gone from 21.2 percent in 2011/12 to 15 percent in 2012/13.
Such a reduction in the non-attendance rate represents a financial saving for the Royal Marsden[2]. In addition, given the important role of screening in the early detection of diabetic retinopathy, such initiatives should have a positive impact over time in preventing sight loss among patients of working age.
Additional work currently under way
The audit commissioned in 2012 also suggested that White and Asian females and African males had higher non-attendance rates when compared with other ethnicities. However, it cautioned against drawing conclusions due to the quality of the data available.
As a result, the service has amended the data collection process for primary care providers. This will provide a more complete ethnicity profile for the population in future and will be used to re-audit service uptake in 2014/15.
[1] For the Royal Marsden Patient and Membership Equality Profile report 2011/2012
[2] According to the Dr Foster Hospital Guide 2012, 5.8 million outpatient appointments were missed by patients in 2011/2012, representing a loss of potential revenue to the NHS of £585 million. Reducing non-attendance rates not only represents a financial saving for the NHS, it is also a way to reduce waiting times and to improve efficiency.
Supporting job applications from disabled people: improving confidence and work experience for disabled people - Frimley Park Hospital
In its employment equality compliance report for 2010/2011, the Frimley Park Hospital NHS Foundation Trust (the Trust) noted that it had received fewer job applications from disabled people than might be expected, given that eight percent of the population in its catchment area is estimated to have a disability.
Although disability is generally underreported among applicants in the job market, the Trust felt that a specific commitment was needed in order to encourage more disabled people to apply for jobs at the Trust. Mindful of the specific duties (under the Public Sector Equality Duty), the hospital defined the following objective to fulfil this aim:
- Work with organisations such as the Shaw Trust to place disabled people with the aim of developing skills and confidence to support long-term employment prospects. This includes provision of support for applying for permanent posts within the organisation.
In 2012/2013, the hospital contacted the Shaw Trust to ask for curriculum vitae of disabled people who were looking for work placements. The Shaw Trust put forward three curriculum vitae and the hospital identified placements that would best suit the skills of these individuals. Assistance with job applications/interviews was given at the end of the placements so that the three individuals could apply for temporary and permanent positions within the Trust.
In 2012/13, the Trust reported the following progress: out of the three disabled people appointed through Shaw Trust on work placements, two have now been appointed as temporary staff, and one to a permanent post.
The work placements at the hospital made a significant difference to the lives of those involved. In particular, it has enabled participants to gain skills and confidence to apply for jobs afterwards. One participant stated that it has enabled him to demonstrate his skills in a real workplace which gave him the confidence to apply for a permanent post in the Trust. 'At the interview, I could talk about real work skills I had developed in my placement, something I had previously been unable to do'.
The hospital is still working with the Shaw Trust to continue providing more disabled people with potential job opportunities in the coming years.
Advice and support
If you think you might have been treated unfairly and want further advice, you can contact the Equality Advisory and Support Service (EASS) .
The EASS is an independent advice service, not operated by the Equality and Human Rights Commission.
Phone: 0808 800 0082
Call the EASS on:
0808 800 0082
Page updates
3 March 2016
Last updated:
Was this page useful? Yes No
Thank you for your feedback
Help us to improve this website
Why isn't this page helpful.
Please tell us more about why this page is not helpful. We can't reply, so, if you need help with a problem, find out where to go for advice.
Do not include personal information such as e-mail, telephone number or address.
What kind of problem are you experiencing on this page?
Stay informed.
Sign up to receive our email newsletter for the latest news, legal action and guidance.

Get inspired with empowering stories from across the health sector.
Speaking the same language
Seeing through wards, super-efficiency saves lives, case studies.
Read our healthcare case studies and discover powerful solutions.
Barking, Havering and Redbridge University NHS Trust
Cambridge university hospitals nhs foundation trust, guy’s and st thomas’ nhs foundation trust, leeds teaching hospitals nhs trust.
- Uncategorised
- Procurement
- Medical records
- Diagnostics
Recent Articles
- Harnessing GS1 standards to reduce unwarranted clinical variation View Case Study
- Harnessing the clinical benefits of point-of-care scanning View Case Study
- CareScan+: Enabling safer more efficient care View Case Study
- Terms and conditions
- Privacy Policy
- Cookie policy
- Competition policy
Department of Health and Social Care introduces Scan4Safety to revolutionise patient care
Key results, gs1 standards allow clinical staff to build a complete patient picture that is easily accessible, increased data visibility can aid efficiencies in catalogue management and staffing, the problem.
The Department of Health and Social Care (DHSC) needed to support the NHS in improving the delivery of patient care through process standardisation and efficiency.
The 2014 NHS eProcurement strategy highlighted that investment in digital platforms, staff organisation, and standardised purchasing could make a huge difference in the way the NHS operates. It calculated that these changes could contribute to cost savings of up to £5 billion per year.
But with varying degrees of readiness across NHS trusts, the challenge to roll out a completely new system across the service was huge.
The solution
With support from GS1 UK, the DHSC announced six NHS acute trusts in England that would act as Scan4Safety demonstrator sites.
£12 million of funding was made available to the six trusts, and teams were asked to focus on three core enablers: patient identification, catalogue management, and location numbering. In addition to this, three use cases were highlighted including purchase to pay, inventory management, and product recall.
GS1 UK also put together an advisory board of industry leaders, senior clinical staff and regulators from across the UK. This team would support all activities in order to ensure success.

"GS1 standards enable everything that happens to a patient to be recorded accurately and with minimal impact on patient or clinical staff. "
The results
The adoption of the Scan4Safety initiative clearly demonstrated that GS1 standards are key in building a more efficient, future-proofed NHS.
Through the use of barcodes and handheld scanners, clinicians are provided with an accurate and real-time record of exactly who did what to the patient, when it happened, and where it took place.
Hosting patient data electronically and accessing it via barcoded wristbands means that any potential problems can be flagged before they happen. For example, if a patient is mistakenly prescribed a treatment that does not tally with their record, the scanning device will flag it immediately.
Submit a case study
If you would like to submit a case study demonstrating how your trust has implemented GS1 standards, email us at [email protected]
- Download the PDF
- icon-share Contact us
- icon-share Submit a case study
Related case studies
Helping nhs organisations better manage non-pay spend, salisbury nhs foundation trust.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Patel V, Chisholm D, Dua T, et al., editors. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2016 Mar 14. doi: 10.1596/978-1-4648-0426-7_ch11

Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4).
Chapter 11 health care platform interventions.
Rahul Shidhaye , Crick Lund , and Dan Chisholm .
Affiliations
- Introduction
Evidence-based interventions often fail to achieve their goal, not so much because of an inherent flaw in the interventions, but because of the unpredictable behavior of the system around them. Every intervention, from the simplest to the most complex, has an effect on the overall system, and the overall system has an effect on every intervention ( Savigny and Adam 2009 ). As a result of this, the current Disease Control Priorities series has shifted its focus from a strictly disorder-oriented intervention analysis (vertical approach) to a more horizontal approach focusing on health system strengthening.
This chapter seeks to identify cost-effective interventions that can be appropriately packaged for one or more specific mental, neurological, and substance use (MNS) disorders, as well as for different levels or platforms of the health or welfare system. A platform is the level of the health or welfare system at which interventions can be appropriately, effectively, and efficiently delivered. A particular platform is defined on the basis of where the intervention will be delivered (the setting) and who will deliver the intervention (service provider). There are essentially three major platforms for the provision of interventions: population, community, and health care. A specific delivery channel—such as a school—can be the vehicle for the delivery of a particular intervention on a specified platform (the community platform). Similarly, a primary health care center is the delivery channel for a specified platform (the health care platform). Identifying the set of interventions that fall within a particular delivery channel will help decision makers to identify potential opportunities, synergies, and efficiencies. This identification will also reflect how resources are often allocated in practice, for example, to schools or primary health care services, rather than to specific interventions or disorders.
Chapter 10 of this volume ( Petersen and others 2015 ) considers the evidence relating to interventions that improve mental health at the population and community levels. This chapter outlines the main elements and features of a health care platform and its delivery channels, namely, informal health care, primary health care, and specialized services. We consider evidence-based interventions that can be delivered in general health care settings and mental health care settings, as well as broader health system–strengthening strategies for more effective and efficient delivery of services on this platform.
- Elements of a Mental Health Care Delivery Platform
Health care services as a delivery platform for improving population mental health consist of three interlinked service delivery channels:
- Self-care and informal health care
- Primary health care
- Specialist health care.
These three key delivery channels map well onto the commonly cited Service Organization Pyramid for an Optimal Mix of Services for Mental Health supported by the World Health Organization (WHO) ( figure 11.1 ) ( WHO 2003a ). At each subsequent level of the pyramid, the mental health needs of individuals become greater and require more intensive professional assistance, usually resulting in higher costs of care. In certain settings beset with conflict, natural disaster, or other emergencies, a further channel for delivering much-needed mental health care is humanitarian aid and emergency response.
Figure 11.1
World Health Organization Service Organization Pyramid for an Optimal Mix of Services for Mental Health.
Self-Care and Informal Health Care
The foundation of the health care delivery platform rests on self-care and emphasizes health worker–patient partnerships. Persons with MNS disorders and their family and friends play a central role in the management of mental health problems. The role of individuals may range from collaborative decision-making concerning their treatment, to actively adhering to prescribed medication, to changing health-related behaviors, such as drug and alcohol use, stress management, and identification of seizure triggers and avoiding them for seizure control.
Self-care is important for MNS disorders, but it is also important for the prevention and treatment of physical health problems ( WHO 2003a ). Self-care is most effective when it is supported by populationwide health promotion programs and formal health care services. Health promotion interventions delivered at the population level can be important in improving mental health literacy by helping people to recognize problems or illnesses, increasing their knowledge about the causes of disorders and options for treatment, and informing them about where to go to get help (see chapter 10 in this volume, Petersen and others 2015 ).
Informal health care comprises service providers who are not part of the formal health care system, such as traditional healers, village elders, faith-based organizations, peers, user and family associations, and lay people ( WHO 2003a ). Traditional and religious healers are of particular significance, as populations throughout East Asia and Pacific, South Asia, Latin America and the Caribbean, and Sub-Saharan Africa often use traditional medicine to meet their health needs ( WHO 2002 ). In many parts of the world, making contact with such informal providers represents the initial pathway to care ( Bekele and others 2009 ); these service providers are typically very accessible and more acceptable because they are integral members of the local community. Given the widespread presence of traditional and religious healers and the shortage of human resources in mainstream biomedical services, it is imperative that primary health and other formal care services establish strong links with informal health care providers, especially traditional healers ( Patel 2011 ). It is also critical to note that the evidence base regarding the effectiveness of services provided by traditional and religious healers is limited. Nevertheless, it is essential to engage with them, as they provide accessible, acceptable, and affordable care, and efforts need to be made to ensure that their practices do not harm the patients.
Peers are another key human resource at this level of health care. Peer-led education and behavioral interventions have been effective with target populations and health issues in low- and middle-income countries (LMICs) ( Manandhar and others 2004 ; Medley and others 2009 ; Tripathy and others 2010 ). Peers are more numerous, may be perceived as more approachable, and may be able to identify with other community members, as they share similar characteristics, experiences, and health conditions with members of the target population ( Simoni and others 2011 ).
Mental health self-help groups form another key component of informal community care. Mental health self-help groups may be defined as “any mutual support oriented initiative directed by people with [MNS disorders] or their family members” ( Brown and others 2008 , 105). Participation in mental health self-help groups has a positive impact on the clinical and social outcomes of patients with MNS disorders ( Pistrang, Barker, and Humphreys 2008 ). Some of these self-help groups are primarily concerned with the provision of peer support, while others may devote their efforts toward changing public policies and, more broadly, changing public attitudes. Still others may focus on self-empowerment, including monitoring and critiquing the mental health services they are receiving ( Cohen and others 2012 ). Social support also plays an important role in self-management of epilepsy ( Jayalakshmi and others 2014 ; Walker and others 2014 ). However, informal community care should not be viewed as a substitute for publicly funded, evidence-based mental health care.
Stigmatization of and discrimination against people with MNS disorders is common in all sections of society, from community to schools, workplace, and even health care settings. Stigma and discrimination present formidable barriers to social inclusion for affected people and their families, and to access to appropriate health care ( Shidhaye and Kermode 2013 ). This is particularly important in the area of self-care and informal care services, which are relatively less regulated and less subject to quality review or policy oversight. Interventions at the community level to address negative attitudes toward people with MNS disorders and improve health care utilization are covered in chapter 10 in this volume ( Petersen and others 2015 ).
Primary Health Care
Delivery of mental health services through primary health care is a fundamental component of a mental health care delivery platform, since it serves as the first level of care within the formal health care system. The strong emphasis on primary health care is due to the fact that the services provided at this level of the health system are generally accessible, affordable, and acceptable for individuals, families, and communities ( WHO 2003a ). Where the provision of mental health care is integrated into these services, access is improved, MNS disorders are more likely to be identified and treated, and comorbid physical and mental health problems can be managed more seamlessly.
Specialist Health Care
Psychiatric services in first-level hospitals and community mental health services.
People with severe MNS disorders may require hospitalization at some point. First-level hospitals provide an accessible and acceptable location for 24-hour medical care for people with acute worsening of disorders, in the same way that these facilities manage acute exacerbations of physical health conditions ( WHO 2003a ).
The mental health services provided in first-level hospitals also enable 24-hour access to services for any physical health problems that might arise during the course of inpatient stays. Ideally, first-level hospitals will have wards dedicated to the treatment of MNS disorders; these wards will have floor plans that support good observation and care, minimizing the risk of neglect and suicide. To minimize the risk of human rights violations, facilities should adhere to clear policies and guidelines that support the treatment and management of MNS disorders within a framework that promotes human dignity and uses evidence-based clinical practice.
In addition, specialist mental health services are needed in the community for severe cases that cannot be managed by generalists. Examples include assertive community treatment teams and community outreach teams, which provide support to service users to enable them to continue to function in the community without requiring admission, and close liaison with general primary care services and other social and criminal justice services ( WHO 2003a ).
Extended-Stay Facilities and Specialist Psychiatric Services
A small minority of people with MNS disorders requires specialist care ( WHO 2003a ). For example, people with treatment-resistant or complex presentations may need to be referred to specialized centers for further testing and treatment. In LMICs with meager resources, the demand of the population and the emphasis of the public health system is to treat persons with severe MNS disorders. These aspects of care provision along with services for vulnerable populations—such as individuals living in abject poverty; women, especially in childbearing age; children facing abuse; and elderly persons—should not be overlooked when designing programs.
Because of their severe mental disorders or intellectual disabilities and lack of family support, many of these individuals may occasionally require ongoing care in community-based residential facilities. Unfortunately, very scarce resources are allocated to these services. The vulnerable populations require particular attention, from a mental health care perspective and a financial risk protection perspective. The final part of this volume addresses the issue of financial risk protection at length. Forensic psychiatry is another type of specialist service in this category. The need for referral to specialist and extended-stay services is reduced when first-level hospitals are staffed with highly specialized health workers, such as psychiatrists and psychologists.
Emergency Mental Health Care
The traumas, personal losses, and other consequences of armed conflict and disasters place affected populations at an increased risk of mental and behavioral problems; these consequences can overwhelm the local capacity to respond, particularly if the existing infrastructure or health system is already weak. Moreover, the local health care system may have been rendered dysfunctional as a result of the emergency situation, placing further limits on access to key resources, such as mental health professionals or essential psychotropic medicines. There is a heightened need to identify and allocate resources to provide mental health and psychosocial support in these humanitarian settings, for those with mental or behavioral problems induced by emergencies and those with preexisting illness. International humanitarian aid and emergency response at the national level can be a channel for rapidly enabling or supporting the availability of and access to basic or specialist care. In many countries, such emergencies have provided opportunities for systemic change or service reform in public mental health ( WHO 2013a ). Emergency response or relief efforts are essentially concerned with setting up, organizing, and rebuilding services for local populations; the central principles and standard practice of care, including what evidence-based interventions should be prioritized, remain unchanged.
Relationships among Different Delivery Channels
No single service delivery channel can meet all mental health needs. For example, on the one hand, primary mental health care must be complemented by specialist care services that primary health workers can use for referrals, support, and supervision; on the other hand, primary mental health care needs to promote and support self-care and informal community care that encourages the involvement of people in their own recovery. Support of self-care and management can be provided via routine primary care visits or via group sessions led by health or lay workers in health care settings or community venues. Another increasingly accessible option for the effective support of self-care and management is telephone- or Internet-based programs. In short, the potential of the health care system as a delivery platform for enhanced mental health and well-being can only be fully realized if genuine continuity and collaboration of care occur across the three service delivery channels; continuity and collaboration, in turn, rely on an appropriate flow of support, supervision, information-sharing, and education.
- Evidence-Based Interventions for Health Care Delivery Platforms
A strong evidence base supports integrated services across the different delivery channels of the health care platform. This evidence has been synthesized in several publications, including the mhGAP Intervention Guide ( WHO 2010b ); a series of papers on packages of care for MNS disorders in LMICs, published in PLoS Medicine ( Patel and Thornicroft 2009 ); and a report on mental health in primary health care ( WHO and WONCA 2008 ). Earlier disagreement and controversy over emergency mental health care has given way to emerging consensus on key social and mental health intervention strategies and principles, as exemplified by the Inter-Agency Standing Committee’s Guidelines on Mental Health and Psychosocial Support in Emergency Settings ( IASC 2007 ); the inclusion of a mental and social aspects of health standard in the handbook on minimal standards in disaster response ( Sphere 2011 ); and the report on sustainable mental health care after emergencies, Building Back Better ( WHO 2013a ).
For each of the delivery channels, interventions may be categorized as follows:
- Promotion and primary prevention
- Identification and case detection
- Treatment, care, and rehabilitation.
Table 11.1 summarizes the evidence base for interventions by various delivery channels. The interventions are intended as examples rather than as recommendations.
Examples of Evidence-Based Interventions Relating to the Mental Health Care Delivery Platform, by Various Delivery Channels.
- System-Strengthening Strategies for Integrated Health Care Delivery
The availability of evidence-based interventions does not ensure their translation into practice. In this section, we address the question of how to integrate evidence-based mental health care interventions into primary care and self-care delivery channels and how to link this integration to specialist care.
A comprehensive and multifaceted approach that contains the following elements is essential for the successful integration of mental health into health care systems:
- A whole-of-government approach involves the promotion, pursuit, and protection of health through concerted action by many sectors of government. These include ministries of planning and development, finance, law and justice, labor, education, and social welfare. The health system cannot tackle the health, social, and economic determinants and consequences of MNS disorders alone.
- A public health approach stresses the establishment of partnerships between patients and service providers, as well as equitable access for the whole population ( Lund and others 2012 ). This approach requires the integration of care at the patient level. Services should be person centered and coordinated across diseases and settings. Collaborative, coordinated, and continuing care, within a framework of evidence-based interventions, provides the foundation of the public health approach. This means providing good quality, accessible services to those in need, as well as preventing the onset of disease and promoting mental health and well-being over the entire life course ( WHO 2010a ). Priority setting and provision of interventions based on the needs of the population under consideration are also an integral part of the public health approach, which is also central to the work undertaken by the Disease Control Priorities Network.
Table 11.2 summarizes the key features of a public mental health approach.
Key Characteristics of a Public Health Approach to MNS Disorder Prevention and Management.
- A systems approach to integrated service planning and development encompasses the critical ingredients of a health system—good governance, appropriate resourcing, timely information, and the actual delivery of health services or technologies—that need to be in place for desired health outcomes or program goals to be realized. Effective governance, strong leadership, and cogent policy making merit particular mention, since they provide the framework for appropriate action and subsequent service development. Indeed, a well-articulated mental health policy, along with a clear mental health implementation plan and budget, can be a strong driver for change and can appreciably boost efforts to deliver mental health services at the primary care level ( WHO and WONCA 2008 ).
How to operationalize the public health, whole-of-government, and systems approaches to integrate service delivery for MNS disorders is a major challenge. In South Africa, some important steps have been taken toward intersectoral collaboration, particularly at the national level, such as a national forum on forensic psychiatry convened by the Department of Health, with the South African Police Service (SAPS), the Department of Justice, and the Department of Correctional Services. The Departments of Education and Correctional Services have developed policies regarding mental health, and SAPS has developed a standing order that sets out roles and responsibilities for police in relation to mental health. At the provincial level, there are formal collaborations between the government department responsible for mental health and other departments and agencies in most provinces across a range of sectors. Some provinces have also established intersectoral forums for mental health, and intersectoral collaboration is a standing item on the agenda of the quarterly meetings of the provincial mental health coordinators. However, at the district level, such intersectoral collaboration is not common. A policy brief prepared by the Mental Health and Poverty Project provides specific recommendations for shared responsibilities in policy and program development among sectors, such as education, social development, housing, justice and constitutional development, correctional services, labor, local government, public works, and mental health ( MHaPP 2008 ).
Many evidence-based interventions fail to translate into practice because key decision makers, especially in LMICs, are merely seen as targets for dissemination of study results by academicians and researchers. To address this challenge, it is imperative to understand that research should be concerned with the users of the research and not purely the production of knowledge. The users may include managers and teams using research findings, executive decision makers seeking advice for specific decisions, policy makers who need to be informed about particular programs, practitioners who need to be convinced to use interventions that are based on evidence, people who are influenced to change their behavior to have a healthier life, or communities that are conducting the research and taking action through the research to improve their conditions. It is critical to involve these actors in the identification, design, and conduct phases of research and program implementation ( Peters and others 2013 ).
Within the three broad approaches, specific strategies can be identified for integrated health care delivery.
Strategy 1: Improving the Organization and Delivery of Services through Collaborative Stepped Care
Collaborative care is an evidence-based approach to improve the management of MNS disorders at the primary care level. The overall aim of collaborative care is to enhance the quality of care and quality of life, consumer satisfaction, and system efficiency for patients with complex, long-term problems ( Kodner and Spreeuwenberg 2002 ). Collaborative care has been used successfully for the management of common mental disorders, such as depression, as well as for comorbidities cutting across multiple services, providers, and settings ( Katon and others 2010 ). Collaborative care is closely related to a stepped care approach; some programs describe themselves as collaborative stepped care , in that they incorporate aspects of each approach within their interventions ( Patel and others 2010 ). In the stepped care approach, patients typically start treatment with low-intensity, low-cost interventions. Treatment results are monitored systematically, and patients move to a higher-intensity treatment only if necessary. Programs seek to maximize efficiency by deploying available human resources according to need, reserving the most specialized and intensive resources for those with the most complex or severe problems.
The essential element of collaborative care is a multidisciplinary team approach that seeks to integrate primary care professionals and specialists. Collaborative care rests primarily on the presence of a case manager with enhanced responsibilities for integration of care across comorbid conditions. It starts with systematic identification of those in need, followed by close involvement of patients in joint decision-making regarding their care. It continues with the design of a holistic care plan that includes medication management and psychological interventions and, where appropriate, social care, with a streamlined referral pathway that allows patients to move easily from one service to another. There is provision for regular and planned monitoring of patients and systematic caseload reviews and consultation with mental health specialists regarding patients who do not show clinical improvement ( WHO and Calouste Gulbenkian Foundation 2014 ).
Collaborative care is the best-evaluated model for treating common mental disorders in primary care. A recent Cochrane Collaboration review of 79 randomized controlled trials concluded that collaborative care for depression is consistently more effective than usual care; it has also been shown to be effective in a range of MNS disorders—anxiety disorders and post-traumatic stress disorder—and for improving general health outcomes. The evidence base for collaborative care is mostly from high-income countries (HICs), although evidence from LMICs is growing ( Archer and others 2012 ). It might be very difficult to replicate these case studies directly in low-income settings, but it is possible to extract the lessons from these experiences and contextualize them for a particular setting. There is absolutely no one-size-fits-all strategy for the heterogeneous settings across and within the countries. It is critical to test rigorously and generate evidence around the contextualization of these strategies in low-resource settings. The Balanced Care Model provides guidelines for the inclusion of program components that are appropriate for the available resources ( Thornicroft and Tansella 2013 ).
Mental health programs can be designed on the basis of these guiding principles, drawing on the following case studies.
- The MANAS (MANashanti Sudhar Shodh, or project to promote mental health) study in Goa, India, is the largest mental health care trial to date in that country. The study showed that a lay counselor–led collaborative stepped care intervention for depression and anxiety disorders in primary health care settings led to substantial reductions in the prevalence of these disorders, suicidal behaviors, and days of work lost, compared with usual care. The trial also evaluated the economic impact of the intervention and found that the overall health system costs were lower in the intervention arm, despite the intervention costs, because patients recovered sooner and had lower overall health care costs ( Patel and others 2010 ).
- The Home Care Program for elderly people affected by dementia, led by the Dementia Society of Goa, evaluated a community-based collaborative care model led by lay counselors. The model showed benefits in reducing caregiver burden and improving caregiver mental health ( Dias and others 2008 ).
- In Chile, a multicomponent intervention lasting three months and comprising nine weekly sessions of psychoeducational groups, structured and systematic follow-up, and pharmacotherapy for women with severe depression, and led by nonmedical health workers, demonstrated that at the six-month follow-up, 70 percent of the stepped care group had recovered, compared with 30 percent in the usual-care group ( Araya and others 2003 ). The program is being rolled out across Chile. A similar program was subsequently tested among low-income mothers in postnatal primary care clinics in Santiago, Chile. The program demonstrated significant improvement in the intervention group ( Rojas and others 2007 ).
- In Ibadan, Nigeria, a pilot study evaluated the usefulness of a stepped care intervention for depression. The intervention was delivered by non-physician primary health workers, with support and supervision by physicians and psychiatrists, as needed, using mobile phones. The intervention was based on WHO’s mhGAP guidelines, adapted for the Nigerian health system. Recovery at follow-up, defined as no longer meeting the Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR , 4th edition ( APA 2000 ), major depression criteria at six months, was achieved by 73.0 percent of the participants in the intervention group and 51.6 percent in the usual-care group, representing a risk difference of 21.4 percent. A fully powered study is being implemented to determine the effectiveness and cost-effectiveness of the package ( WHO and Calouste Gulbenkian Foundation 2014 ).
- The Headache Management Trial assessed the effect of a coordinated headache management program in general clinical practice. Patients in the intervention arm received a headache management program consisting of a class specifically designed to inform them about headache types, triggers, and treatment options; diagnosis and treatment by a professional specially trained in headache care; and proactive follow-up by a case manager. This trial demonstrated that a systematic approach to headache care is practical and achievable in a general clinical setting and effectively reduced headache disability in a wide range of patients ( Matchar and others 2008 ).
These case studies primarily focused on evidence generation and were conducted in controlled settings. There are also several case studies from LMICs.
- In the city of Sobral, Brazil, primary care practitioners conducted physical and mental health assessments for all patients as part of integrated primary care for mental health. Primary care practitioners treat patients if they are able, or request an assessment from a specialist mental health team, which makes regular visits to family health centers. Joint consultations are undertaken among mental health specialists, primary care practitioners, and patients. This model ensures good-quality mental health care, and it serves as a training and supervision tool whereby primary care practitioners gain skills that enable greater competence and autonomy in managing mental disorders ( WHO and WONCA 2008 ).
- A similar model is being practiced as part of the District Mental Health Programme in Thiruvananthapuram district, Kerala, India. Trained medical officers diagnose and treat mental disorders as part of their general primary care functions. A multidisciplinary district mental health team provides outreach clinical services, including direct management of complex cases and in-service training and support of the trained medical officers and other workers in the primary care centers. The primary care centers have incrementally assumed responsibility for independently operating mental health clinics with minimal support from the mental health team ( WHO and WONCA 2008 ).
- In the Moorreesburg district of Western Cape province, South Africa, the role of primary care practitioners is filled by general primary care nurses, who provide basic mental health services in the primary health clinic. They are supported by specialist mental health nurses and a psychiatrist, who visits the clinic intermittently to manage complex cases and provide supervision ( WHO and WONCA 2008 ).
- The European Headache Federation and Lifting the Burden: the Global Campaign against Headache ( Steiner and others 2011 ) has proposed a collaborative care model for the management of headache disorders. In this model, 90 percent of people consulting for migraine and tension-type headaches can be diagnosed and managed by staff at the primary care level. In the case of the remaining 10 percent of the patients, common primary and secondary headache disorders can be recognized but not necessarily managed; these can be referred to the next level, where physicians can provide more advanced care. Finally, specialists can provide advanced care to approximately 1 percent of patients first seen at the first-level and second-level facilities, and can focus on the diagnosis and management of the underlying causes of all secondary headache disorders. There is a demonstrational intervention project based on this model in Yekaterinburg, Sverdlovsk Oblast, Russian Federation ( Lebedeva and others 2013 ). Headache services in China have been designed on this model ( Yu and others 2014 ).
The collaborative stepped care approach relies heavily on the introduction of additional human resources, identification of core competencies, adequate training to ensure that these core competencies are fulfilled, and specialist support to maintain these competencies. The next section describes this critical component of mental health system strengthening in more detail.
Strategy 2: Strengthening Human Resources for Mental Health through Task-Sharing
One of the main reasons for the substantial treatment gap for MNS disorders is the lack of a skilled workforce. In HICs, the number of mental health workers is often inadequate; in LMICs, the situation is dramatically worse, with an estimated shortage of 1.18 million workers ( Kakuma and others 2011 ). The collaborative stepped care approach can be implemented only if skilled human resources are available at the different levels of service delivery.
Task-Sharing Approach
Task-sharing is a human resource innovation in which the skills to deliver specific mental health care tasks are transferred to appropriately trained and supervised general health workers. This process helps in improving access to evidence-based mental health care and leads to more efficient use of the limited resources. This approach has been evaluated for mental health service delivery, and its efficacy has been established using rigorous evaluation methodologies ( Araya and others 2003 ; Patel and others 2010 ; Rahman and others 2008 ). Task-sharing is implemented through a collaborative care framework with four key human resources: the community health worker or case manager; the person with a mental health problem and family members; the primary or general health care physician; and the mental health professional ( Bower and Gilbody 2005 ). The overall shortage of human resources can be addressed by introducing newly skilled nonspecialist health workers at the community level; reorienting medical officers and paramedical staff to integrate mental health interventions; and redefining the role of specialists from service providers to leaders, trainers, and supervisors of mental health programs.
The task-sharing approach is at the heart of establishing the collaborative stepped care model of care; the most crucial element in this approach is the availability of a case manager. The results of the MANAS trial clearly indicate the effectiveness of a lay health counselor or case manager leading the collaborative stepped care intervention for common mental disorders in public primary health care facilities in India ( Patel and others 2010 ). Several global case studies have found that primary care for mental health is usually most effective where a mental health coordinator or case manager is responsible for overseeing integration ( WHO and WONCA 2008 ). These case managers can play a crucial role in screening; engaging; educating patients and family members; maintaining close follow-up; tracking adherence and clinical outcomes; and delivering targeted, evidence-based, psychological interventions, such as motivational interviewing, behavioral activation, problem solving, or interpersonal therapy ( Patel and others 2013 ). The case managers can serve as the link between the primary care and self-care platforms, and can work under the close supervision of the medical officers. The evidence base for psychological interventions delivered using a task-sharing approach is set out in box 11.1 .
Clinical and Functional Outcomes of Psychological Interventions Delivered Using a Task-Sharing Approach. Recovery of adults suffering from depression or anxiety, or both, at 7–12 months following the intervention Reduction in symptoms for mothers (more...)
A recent multi-site, qualitative study as part of the PRogramme for Improving Mental health carE (PRIME) investigated the acceptability and feasibility of task-sharing mental health care in five LMICs. The study examined the perceptions of primary care service providers (physicians, nurses, and community health workers), community members, and service users ( Mendenhall and others 2014 ). Task-sharing mental health services is feasible as long as the following key conditions are met:
- Increased numbers of human resources and better access to medications
- Ongoing structured supportive supervision at the community and primary care levels
- Adequate training and compensation for health workers involved in task-sharing.
Competency-Based Education
Primary care workers function best when their tasks related to mental health service delivery are limited and achievable. The most common reasons for failure to integrate mental health care into primary care programs are the lack of adequate assessment and the overly ambitious target-setting without the necessary customization of the detailed activities, and a full and explicit agreement on the targets and activities needed to achieve them ( Patel and others 2013 ). A shift away from knowledge-based education to competency-based education is needed. This approach mainly focuses on the skills of providers, with the ultimate goal of improving patient outcomes. Competency is defined as an attribute of an individual human resource and the ability of that worker to deliver an intervention to a desired performance standard based on the acquired knowledge and skills.
The Institute of Medicine’s (IOM) Forum on Neuroscience and Nervous System Disorders convened a workshop to discuss and identify core competencies that specialized and nonspecialized primary care providers might need to help ensure the effective delivery of services for depression, psychosis, epilepsy, and alcohol use disorders in Sub-Saharan Africa ( IOM 2013 ). Table 11.3 lists the steps to strengthen human resource competencies for MNS disorders; the core competencies for all service providers across MNS disorders are listed in table 11.4 . In addition to the common competencies for all service providers, the IOM framework also focuses on a diverse range of cadre-specific competencies.
Steps to Strengthen Human Resource Competencies for MNS Disorders.
Core Competencies for All Service Providers across MNS Disorders.
Pre-service and in-service training of primary care workers on mental health issues is an essential prerequisite for the integration of mental health into primary care platforms. The training, to the extent possible, should happen in primary care or community mental health care facilities, to ensure that practical experience is gained and that ongoing training and support are facilitated ( WHO and WONCA 2008 ). The effects of training are nearly always short lived if health workers do not practice newly learned skills and receive ongoing specialist supervision. A trial from Kenya did not find any impact of the training program of medical officers on improvement in diagnostic rates of mental disorders ( Jenkins and others 2013 ). A quasi-experimental study from Brazil had similar findings and noted that wider changes in the system of care may be required to augment training and encourage reliable changes in clinical practice ( Goncalves and others 2013 ). Ongoing support and supervision from mental health specialists are essential. Case studies from Australia, Brazil, and South Africa have demonstrated that a collaborative stepped care approach, in which joint consultations and interventions occur between primary care workers and mental health specialists, increases the skills of primary care workers and builds mental health networks ( WHO and WONCA 2008 ).
Specialist Transitioning
Specialists, especially in LMICs, are usually engaged in service delivery. It is imperative to make a transition from providing clinical services to training and supervising the primary health care staff and providing direct clinical interventions judiciously and sparingly. In separate projects focusing on integrated primary care for mental health in the city of Sobral, Brazil, and the Sembabule district of Uganda, specialists together with medical officers in primary care visited primary care settings and assessed patients. Over time, psychiatrists started taking less active roles, while general practitioners assumed added responsibilities, under the supervision of the psychiatrists. Specialists can interact with primary care staff via referral and back-referral ( WHO and WONCA 2008 ).
Planning and Consultation
Involving primary health care staff in the overall program planning and rollout process enhances ownership and commitment to achieve the planned outcomes within agreed timelines ( Patel and others 2013 ). Consultations with general practitioners have been demonstrated to be one of the key factors in the success of the new mental health services in Australia ( WHO and WONCA 2008 ). Decisions need to be made after careful consideration of local circumstances; this requires consultation with policy makers as well as users of mental health services and their families and the primary care staff.
Psychotropic Medications
It is important to ensure that primary care staff members have the appropriate permission to prescribe psychotropic medications, and they must be adequately trained to perform this task. In many countries, nurses and even general physicians are not permitted to prescribe psychotropic medications. If access to psychotropic medications is to be improved, then initiatives to allow primary care nurses to prescribe psychotropic medications need to be promoted and undertaken, provided appropriate training and supervision is conducted. In Belize, psychiatric nurse practitioners have been given additional prescription rights. In Uganda, general primary care nurses are permitted to prescribe psychotropic medication to patients who require continued medication on the recommendation of a mental health professional ( WHO and WONCA 2008 ).
Strategy 3: Integrating Mental Health into Existing Health Programs
MNS disorders frequently occur throughout the course of many noncommunicable diseases and infectious diseases, such as HIV/AIDS and tuberculosis, increasing morbidity and mortality ( Prince and others 2007 ). People with comorbid disorders risk poor outcomes for both disorders. To achieve the desired outcomes for priority programs in the health sector, it is crucial to manage MNS disorders, pursue synergies in the health system, and deliver interventions through integrated approaches to care. Expansion and integration of mental health services in primary health care can be achieved by using existing service delivery for maternal and child health, noncommunicable diseases, and HIV/AIDS and tuberculosis ( Collins and others 2013 ). Patients with severe MNS disorders often do not receive appropriate care for their general health conditions because of the negative attitudes of service providers, resulting in reductions of 10–25 years in life expectancy compared with the general population. Integration of MNS services within other health care platforms is essential.
Maternal and Child Health Programs
Maternal depression is the second leading cause of disease burden in women worldwide, following infections and parasitic diseases ( Rahman and others 2013 ). Systematic reviews from HICs provide evidence of the effectiveness of psychological therapies—including cognitive behavioral therapy (CBT) and interpersonal therapy that can be delivered in individual or group format—and pharmacotherapy in the treatment of maternal depression ( Rahman and others 2013 ). Promising evidence suggests the benefits of the integration of maternal mental health into maternal and child health (MCH) programs. Examples of community-based trials with a maternal mental health component integrated into an MCH program, and a case study demonstrating that the screening and management of maternal mental disorders can be integrated successfully into an existing health system at a facility level, build a strong case for the integration of mental health care into MCH programs ( Rahman and others 2013 ). The Thinking Healthy Programme in Pakistan is a simple and culturally appropriate intervention for integrating depression care into an MCH program. The intervention is child centered, ensuring buy-in from the families and avoiding stigmatization. It is woven into the routine work of the community health workers, so it is not perceived as an additional burden. The Thinking Healthy Programme has been further adapted so that it can be used universally for all women rather than only depressed women ( Rahman and others 2013 ).
The Perinatal Mental Health Project in the Western Cape Province in South Africa developed a stepped care intervention for maternal mental health that is integrated into antenatal care in three primary care midwife obstetric units ( Honikman and others 2012 ). Midwives are trained to screen women routinely during their antenatal visits for maternal mood and anxiety disorders. Women who screen positive for anxiety or depression are referred to onsite counselors who also act as case managers. Women are referred to an onsite psychiatrist when specialist intervention is indicated. The Perinatal Mental Health Project works directly with facility managers and health workers through collaborative partnerships, focusing on problem solving and capacity development in the primary health care system. Over a three-year period, 90 percent of all women attending antenatal care in the maternity clinic were offered mental health screening, with 95 percent uptake. Of those screened, 32 percent qualified for referral; of these, 47 percent received counseling through the program. This case study clearly demonstrates that onsite, integrated mental health services can increase access for women who have scarce resources and competing health, family, and economic priorities ( Honikman and others 2012 ).
Parenting skills training aims to enhance and support the parental role through education and skills enhancement, thereby improving emotional and behavioral outcomes for children. Primary health care workers can play a significant role in this training. The use of scarce professional resources to train parents is a cost-effective use of resources. Several systematic reviews have shown parent skills training to be effective for reducing internalizing and externalizing problems in children ( Furlong and others 2012 ; Kaminski and others 2008 ), as well as reducing the risk of unintentional childhood injuries ( Kendrick and others 2013 ) and improving the mental health of parents ( Barlow and others 2014 ). Individual and group parent training have been beneficial. Four components of parenting skills training have been found to be most effective:
- Increasing positive parent-child interactions
- Teaching parents how to communicate emotionally with their children
- Teaching parents the use of time-out as a means of discipline
- Supporting parents to respond in a consistent manner to their children’s behavior ( Kaminski and others 2008 ).
Noncommunicable Disease Programs
Existing service delivery platforms for noncommunicable diseases are also promising entry points for the integration of mental health into primary care. The collaborative care models discussed demonstrate a strong evidence base for integration in primary care settings.
In North America, TEAMcare USA and TEAMcare Canada provide team-based primary care for diabetes, coronary heart disease, and depression. TEAMcare trains primary care staff to work in collaborative teams that deliver care in a clinic and by phone. Each service user is assigned a TEAMcare care manager, usually a medically supervised nurse, who serves as the conduit for the consultation team, the primary care team, and the service user. The program takes a treat-to-target approach, modifying treatment as needed to ensure improvement in symptoms. The program teaches self-care skills to service users to control illnesses and encourages behaviors that enhance the quality of life. About 1,400 people have received TEAMcare, with a trial showing improvements in medical disease control and depression symptoms ( Katon and others 2012 ). In the United Kingdom, 3 Dimensions of Care for Diabetes uses a team consisting of a psychiatrist and a social worker from a nongovernmental organization embedded in the diabetes care team to integrate medical, psychological, and social care for people with diabetes and mental health problems, and social problems, such as housing and debt ( Parsonage, Fossey, and Tutty 2012 ).
The National Depression Detection and Treatment Program in Chile integrated depression care with more traditional primary care programs for the management of hypertension and diabetes within a network of 520 primary care clinics. The program follows a collaborative stepped care approach and is led by psychologists, with additional support from physicians and specialists for severe depression ( Araya and others 2012 ). In Myanmar and several other LMICs, epilepsy has been included as part of the process of local adaptation and implementation of WHO’s package of essential noncommunicable disease interventions in primary care ( WHO and Calouste Gulbenkian Foundation 2014 ).
Care for patients with dementia can be well integrated with health care for noncommunicable diseases. Patients with dementia need to be assessed for behavioral and psychosocial symptoms, in addition to a careful physical assessment to monitor hearing and visual impairments, pain, constipation, urinary tract infections, and bed sores that may explain some exacerbation of psychological symptoms. Monitoring and effective treatment of vascular risk factors and diseases, including high blood pressure, hypercholesterolemia, smoking, obesity, and diabetes, to improve secondary prevention of cerebrovascular events, are an integral component of care. A well-conducted clinical trial of cognitive stimulation (reality orientation, games, and discussions based on information processing rather than knowledge) conducted in the United Kingdom as a group intervention and a small pilot trial from Brazil suggest that cognitive benefits from this intervention are similar to the benefits from pharmacological management of dementia using cholinesterase inhibitors ( Prince and others 2009 ). Cognitive rehabilitation, an individualized therapy designed to enhance residual cognitive skills and cope with deficits, showed promise in uncontrolled case series undertaken in HICs. A large body of literature attests to the benefits of caregiver interventions in dementia. These include psychoeducational interventions, often caregiver training; psychological therapies such as CBT and counseling; caregiver support; and respite care ( Chapter 5 in this volume, Thakur and others 2015 ). Many interventions combine several of these elements. Interventions targeting the caregiver may have small, but significant, beneficial effects on the behavior of the person with dementia.
HIV/AIDS and Tuberculosis Programs
WHO’s Integrated Management of Adult and Adolescent Illness (IMAI) is a broadly disseminated health care strategy that addresses the overall health of patients with HIV/AIDS and co-occurring tuberculosis; clear opportunities exist for the integration of mental health in this program. IMAI promotes the inclusion of mental health in the overall care model for HIV/AIDS, as the mental health needs of many persons living with HIV/AIDS can be largely addressed with little duplication or waste, while improving program outcomes, such as antiretroviral drug adherence ( WHO 2013b ). Interventions for substance use disorders can be integrated with HIV/AIDS interventions. This delivery channel can be used to identify individuals who use injectable drugs, as well as those with dependence on opioids, cannabis, and cocaine. The evidence base supports the efficacy of brief interventions on harm from drug use and the overall pattern of drug consumption, including drug abstinence. The brief intervention constitutes a single session of 5–30 minutes, incorporating individualized feedback and advice on reducing or stopping cannabis/psychostimulant consumption, and the offer of follow-up ( NICE 2008 ).
In South Africa, the government has published integrated guidelines for all primary health workers, including HIV/AIDS; major noncommunicable diseases; and a range of mental health problems, including depression, anxiety, mania, substance abuse, and psychosis. These guidelines, called Primary Care 101 (PC101) ( DOH 2012 ), are used by the national Department of Health as part of a primary care revitalization program to deliver integrated care within a chronic disease management framework ( Asmall and Mahomed 2013 ). This approach includes consolidating care for all patients with chronic diseases into a single care delivery point at the facility level and strengthening clinical decision support for nurses. PC101 provides a set of clinical algorithms using a pragmatic signs-and-symptoms approach and integrates detection and management of MNS disorders with other chronic conditions. The guidelines include training materials delivered in a cascaded train-the-trainer format and ongoing support for primary care practitioners from trainers at the district and sub-district levels. At the community level, outreach teams of community health workers are trained to support clinically stable patients and self-care.
- Quality of Care for MNS Disorders
Quality in health care has been defined by the IOM as the degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge ( IOM 2001 ). Good-quality care is effective, efficient, equitable, timely, person centered, and safe, and delivers a positive patient experience ( IOM 2001 ).
Despite the strong and growing knowledge base for delivery of mental health services, the treatment gap for MNS disorders remains unacceptably large, with over 90 percent of people with mental disorders in LMICs going without treatment ( Kohn and others 2004 ). This treatment gap is not just a quantitative phenomenon; it also contains an important quality of care dimension. There is a significant gap between what is known about effective treatment and what is actually provided to and experienced by consumers in routine care ( Proctor and others 2009 ). In the language of universal health coverage, it is the difference between contact coverage and effective coverage; that is, substantial improvement in access to care needs to be accompanied by improvement in the quality of service delivery. The inadequacy of resources and low priority given to MNS disorders might suggest that consideration of the quality of care is subservient to the quantity of available and accessible services. However, quality improvement (QI) mechanisms ensure that available resources are well-utilized, in the sense that those in contact with services actually derive appropriate benefit from evidence-based interventions.
Moreover, good-quality services help to build people’s confidence in making use of mental health care interventions, increasing the likelihood of seeking the care that they need ( Funk and others 2009 ). Low-quality services lead people with MNS disorders to experience human rights violations and discrimination in health care settings. In many countries, the quality of care in inpatient and outpatient facilities is poor or even harmful and can actively hinder recovery ( The Health Foundation 2013 ).
QI methods have been shown to be effective for sustained scale-up and adaptation of standardized treatment packages for Millennium Development Goal health priority areas. QI could be included as a routine part of mental health implementation and customization ( Patel and others 2013 ). Quality assurance (QA) involves the use of tools and logic to assess quality performance. QI is the use of methods to enhance quality performance. QA/QI is an integrative process for identifying current levels of quality and improving the quality of performance. QA/QI plays an important role in monitoring and improving the implementation of evidence-based practices; it also helps to monitor and improve the quality of training and supervision required for the delivery of services. Some important QI approaches are continuous quality improvement, Lean, Six Sigma, Plan Do Study Act, Statistical Process Control, and Total Quality Management ( The Health Foundation 2013 ).
QI frameworks and guidelines for LMICs have been developed in the form of a WHO guidance package for QI in mental health services ( WHO 2003b ). The package provides an integrated resource for the planning and refining of mental health systems on a national scale ( Funk and others 2009 ). In a quality framework, standards and criteria are important tools for assessment and improvement. A standard is a broad statement of the desired and achievable level of performance against which actual performance can be measured. The criteria are measurable elements of service provision. Criteria relate to the desired outcome or performance of staff or services. The standard is achieved when all criteria associated with it are met.
Protection of human rights is a critical aspect of the quality of mental health care. The treatment provided in health care settings is often intended to keep people and their conditions under control rather than to enhance their autonomy and improve their quality of life. People can be seen as objects of treatment rather than human beings with the same rights and entitlements as everybody else. They often are not consulted on their care or recovery plans; many receive treatment against their wishes. The situation in inpatient facilities is often far worse: people may be locked away for weeks, months, and even years in psychiatric hospitals or social care homes, where they can be subject to dehumanizing, degrading treatment, including violence and abuse ( WHO 2003b ).
WHO developed the QualityRights Toolkit to assess and improve the quality of life and human rights of people with MNS disorders receiving treatment in mental health and social care facilities ( WHO 2012 ). People living in these facilities are isolated from society and have little or no opportunity to lead normal, fulfilling lives in the community. WHO recommends that countries progressively close down this type of facility and instead establish community-based services and integrate mental health into primary care services and the services offered by general hospitals. Although this tool does not endorse long-stay facilities as an appropriate setting for treatment and care, as long as these types of facilities continue to exist all over the world, there is a need to promote the rights of those residing in them.
The QualityRights Toolkit covers the following five themes drawn from the United Nations Convention on the Rights of Persons with Disabilities:
- Right to an adequate standard of living and social protection
- Right to enjoyment of the highest attainable standard of physical and mental health
- Right to exercise legal capacity and the right to personal liberty and security of person
- Freedom from torture or cruel, inhuman, or degrading treatment or punishment and from exploitation, violence, and abuse
- Right to live independently and be included in the community.
A comprehensive assessment of facilities based on these themes can help to identify problems in existing health care practices and to plan effective means to ensure that the services are of good quality, respectful of human rights, and responsive to the users’ requirements, and promote the users’ autonomy, dignity, and right to self-determination.
- Conclusions
This chapter has described the health care delivery platform and its delivery channels and evidence-based interventions. The key points for effective and efficient delivery of mental health services are as follows:
- To deliver interventions for MNS disorders, the focus needs to move from vertical programs to horizontal health service platforms.
- The WHO pyramid framework of self-care, primary care, and specialist care continues to provide a useful approach for understanding potential delivery channels.
- A set of evidence-based interventions within this framework can be identified for promotion and prevention; identification and case detection; and treatment, care, and rehabilitation interventions.
- The delivery of these interventions requires an approach that embraces public health, systems, and whole-government principles.
- The key strategies for this delivery are implementing collaborative stepped care, strengthening human resources, and integrating mental health into general health care.
- Finally, it is important not only to improve access to health services, but also to focus on improving the quality of care delivered.
Recommendations for policy makers include adopting these principles and strategies using a platformwide approach. Policy makers need to engage with a wide range of stakeholders in this process and make use of the best available evidence in a transparent manner.
- APA (American Psychiatric Association). 2000. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR . 4th ed., text revision. Washington, DC: APA.
- Araya R, Alvarado R, Sepulveda R, Rojas G. 2012. “ Lessons from Scaling Up a Depression Treatment Program in Primary Care in Chile .” Revista Panamericana de Salud Publica 32 (3): 234–40. [ PubMed : 23183564 ]
- Araya R, Rojas G, Fritsch R, Gaete J, Rojas M. others. 2003. “ Treating Depression in Primary Care in Low-Income Women in Santiago, Chile: A Randomised Controlled Trial .” The Lancet 361 (9362): 995–1000. doi:10.1016/S0140-6736(03)12825-5. [ PubMed : 12660056 ]
- Archer J, Bower P, Gilbody S, Lovell K, Richards D. others. 2012. “ Collaborative Care for Depression and Anxiety Problems .” Cochrane Database of Systematic Reviews 10: CD006525. doi:10.1002/14651858.CD006525.pub2. [ PubMed : 23076925 ]
- Asmall S, Mahomed O H. 2013. The Integrated Chronic Disease Management Manual . Pretoria, South Africa: Department of Health.
- Barlow J, Smailagic N, Huband N, Roloff V, Bennett C. 2014. “ Group-Based Parent Training Programmes for Improving Parental Psychosocial Health .” Cochrane Database of Systematic Reviews 5: CD002020. doi:10.1002/14651858.CD002020.pub4. [ PubMed : 24838729 ]
- Bekele Y Y, Flisher A J, Alem A, Baheretebeb Y. 2009. “ Pathways to Psychiatric Care in Ethiopia .” Psychological Medicine 39 (3): 475–83. doi:10.1017/S0033291708003929. [ PubMed : 18606050 ]
- Bower P, Gilbody S. 2005. “ Managing Common Mental Health Disorders in Primary Care: Conceptual Models and Evidence Base .” BMJ 330 (7495): 839–42. doi:10.1136/bmj.330.7495.839. [ PMC free article : PMC556082 ] [ PubMed : 15817554 ]
- Brown L D, Shepherd M D, Wituk S A, Meissen G. 2008. “ Introduction to the Special Issue on Mental Health Self-Help .” American Journal of Community Psychology 42 (1–2): 105–09. doi:10.1007/s10464-008-9187-7. [ PubMed : 18597168 ]
- Clarke K, King M, Prost A. 2013. “ Psychosocial Interventions for Perinatal Common Mental Disorders Delivered by Providers Who Are Not Mental Health Specialists in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis .” PLoS Medicine 10 (10): e1001541. doi:10.1371/journal.pmed.1001541. [ PMC free article : PMC3812075 ] [ PubMed : 24204215 ]
- Cohen A, Raja S, Underhill C, Yaro B P, Dokurugu A Y. others. 2012. “ Sitting with Others: Mental Health Self-Help Groups in Northern Ghana .” International Journal of Mental Health Systems 6 (1): 1. doi:10.1186/1752-4458-6-1. [ PMC free article : PMC3366888 ] [ PubMed : 22436354 ]
- Collins P Y, Insel T R, Chockalingam A, Daar A, Maddox Y T. 2013. “ Grand Challenges in Global Mental Health: Integration in Research, Policy, and Practice .” PLoS Medicine 10 (4): e1001434. doi:10.1371/journal.pmed.1001434. [ PMC free article : PMC3640093 ] [ PubMed : 23637578 ]
- Dias A, Dewey M E, D’Souza J, Dhume R, Motghare D D. others. 2008. “ The Effectiveness of a Home Care Program for Supporting Caregivers of Persons with Dementia in Developing Countries: A Randomised Controlled Trial from Goa, India .” PLoS One 3 (6): e2333. [ PMC free article : PMC2396286 ] [ PubMed : 18523642 ]
- DOH (Department of Health). 2012. “ Primary Care 101 .” DOH, Pretoria , South Africa.
- Funk M, Lund C, Freeman M, Drew N. 2009. “ Improving the Quality of Mental Health Care .” International Journal for Quality in Health Care 21 (6): 415–20. doi:10.1093/intqhc/mzp048. [ PubMed : 19841029 ]
- Furlong M, McGilloway S, Bywater T, Hutchings J, Smith S M. others. 2012. “ Behavioural and Cognitive-Behavioural Group-Based Parenting Programmes for Early-Onset Conduct Problems in Children Aged 3 to 12 Years .” Cochrane Database of Systematic Reviews 2: CD008225. doi:10.1002/14651858.CD008225.pub2. [ PubMed : 22336837 ]
- Goncalves D A, Fortes S, Campos M, Ballester D, Portugal F B. others. 2013. “ Evaluation of a Mental Health Training Intervention for Multidisciplinary Teams in Primary Care in Brazil: A Pre- and Posttest Study .” General Hospital Psychiatry 35 (3): 304–08. doi:10.1016/j.genhosppsych.2013.01.003. [ PubMed : 23521815 ]
- Honikman S, van Heyningen T, Field S, Baron E, Tomlinson M. 2012. “ Stepped Care for Maternal Mental Health: A Case Study of the Perinatal Mental Health Project in South Africa .” PLoS Medicine 9 (5): e1001222. doi:10.1371/journal.pmed.1001222. [ PMC free article : PMC3362637 ] [ PubMed : 22666181 ]
- IASC (Inter-Agency Standing Committee). 2007. Guidelines on Mental Health and Psychosocial Support in Emergency Settings . Geneva: IASC.
- IOM (Institute of Medicine). 2001. Crossing the Quality Chasm: A New Health System for the 21st Century . Washington, DC: National Academies Press. [ PubMed : 25057539 ]
- IOM (Institute of Medicine). 2013. “ Strengthening Human Resources through Development of Candidate Core Competencies for Mental, Neurological, and Substance Use Disorders in Sub-Saharan Africa: Workshop Summary .” National Academies Press , Washington, DC. [ PubMed : 24199264 ]
- Jayalakshmi S, Padmaja G, Vooturi S, Bogaraju A, Surath M. 2014. “ Impact of Family Support on Psychiatric Disorders and Seizure Control in Patients with Juvenile Myoclonic Epilepsy .” Epilepsy and Behavior 37: 7–10. doi:10.1016/j.yebeh.2014.05.020. [ PubMed : 24949575 ]
- Jenkins R, Othieno C, Okeyo S, Kaseje D, Aruwa J. others. 2013. “ Short Structured General Mental Health in Service Training Programme in Kenya Improves Patient Health and Social Outcomes But Not Detection of Mental Health Problems—A Pragmatic Cluster Randomised Controlled Trial .” International Journal of Mental Health Systems 7 (1): 25. doi:10.1186/1752-4458-7-25. [ PMC free article : PMC4174904 ] [ PubMed : 24188964 ]
- Kakuma R, Minas H, van Ginneken N, Dal Poz M R, Desiraju K. others. 2011. “ Human Resources for Mental Health Care: Current Situation and Strategies for Action .” The Lancet 378 (9803): 1654–63. doi:10.1016/S0140-6736(11)61093-3. [ PubMed : 22008420 ]
- Kaminski J W, Valle L A, Filene J H, Boyle C L. 2008. “ A Meta-Analytic Review of Components Associated with Parent Training Program Effectiveness .” Journal of Abnormal Child Psychology 36 (4): 567–89. doi:10.1007/s10802-007-9201-9. [ PubMed : 18205039 ]
- Katon W J, Lin E H, Von Korff M, Ciechanowski P, Ludman E J. others. 2010. “ Collaborative Care for Patients with Depression and Chronic Illnesses .” New England Journal of Medicine 363 (27): 2611–20. doi:10.1056/NEJMoa1003955. [ PMC free article : PMC3312811 ] [ PubMed : 21190455 ]
- Katon W, Russo J, Lin E H, Schmittdiel J, Ciechanowski P. others. 2012. “ Cost-Effectiveness of a Multicondition Collaborative Care Intervention: A Randomized Controlled Trial .” Archives of General Psychiatry 69 (5): 506–14. doi:10.1001/archgenpsychiatry.2011.1548. [ PMC free article : PMC3840955 ] [ PubMed : 22566583 ]
- Kendrick D, Mulvaney C A, Ye L, Stevens T, Mytton J A. others. 2013. “ Parenting Interventions for the Prevention of Unintentional Injuries in Childhood .” Cochrane Database of Systematic Reviews 3: CD006020. doi:10.1002/14651858.CD006020.pub3. [ PMC free article : PMC8908963 ] [ PubMed : 23543542 ]
- Kodner D L, Spreeuwenberg C. 2002. “ Integrated Care: Meaning, Logic, Applications, and Implications: A Discussion Paper .” International Journal of Integrated Care 2: e12. [ PMC free article : PMC1480401 ] [ PubMed : 16896389 ]
- Kohn R, Saxena S, Levav I, Saraceno B. 2004. “ The Treatment Gap in Mental Health Care .” Bulletin of the World Health Organization 82 (11): 858–66. [ PMC free article : PMC2623050 ] [ PubMed : 15640922 ]
- Lebedeva E R, Olesen J, Osipova V V, Volkova L I, Tabeeva G R. others. 2013. “ The Yekaterinburg Headache Initiative: An Interventional Project, within the Global Campaign against Headache, to Reduce the Burden of Headache in Russia .” Journal of Headache Pain 14: 101. doi:10.1186/1129-2377-14-101. [ PMC free article : PMC3880007 ] [ PubMed : 24367919 ]
- Lund C, Tomlinson M, De Silva M, Fekadu A, Shidhaye R. others. 2012. “ PRIME: A Programme to Reduce the Treatment Gap for Mental Disorders in Five Low- and Middle-Income Countries .” PLoS Medicine 9 (12): e1001359. [ PMC free article : PMC3531506 ] [ PubMed : 23300387 ]
- Manandhar D S, Osrin D, Shrestha B P, Mesko N, Morrison J. others. 2004. “ Effect of a Participatory Intervention with Women’s Groups on Birth Outcomes in Nepal: Cluster-Randomised Controlled Trial .” The Lancet 364 (9438): 970–79. doi:10.1016/S0140-6736(04)17021-9. [ PubMed : 15364188 ]
- Matchar D B, Harpole L, Samsa G P, Jurgelski A, Lipton R B. others. 2008. “ The Headache Management Trial: A Randomized Study of Coordinated Care .” Headache 48 (9): 1294–310. doi:10.1111/j.1526-4610.2007.01148.x. [ PubMed : 18547268 ]
- Medley A, Kennedy C, O’Reilly K, Sweat M. 2009. “ Effectiveness of Peer Education Interventions for HIV Prevention in Developing Countries: A Systematic Review and Meta-Analysis .” AIDS Education and Prevention 21 (3): 181–206. doi:10.1521/aeap.2009.21.3.181. [ PMC free article : PMC3927325 ] [ PubMed : 19519235 ]
- Mendenhall E, De Silva M J, Hanlon C, Petersen I, Shidhaye R. others. 2014. “ Acceptability and Feasibility of Using Non-Specialist Health Workers to Deliver Mental Health Care: Stakeholder Perceptions from the PRIME District Sites in Ethiopia, India, Nepal, South Africa, and Uganda .” Social Science and Medicine 118C: 33–42. doi:10.1016/j.socscimed.2014.07.057. [ PMC free article : PMC4167946 ] [ PubMed : 25089962 ]
- MHaPP (Mental Health and Poverty Project). 2008. “ Inter-Sectoral Collaboration for Mental Health in South Africa .” World Health Organization , Geneva. http://www .who.int/mental_health /policy/development/MHPB5 .pdf .
- NICE (National Institute for Health and Care Excellence). 2008. “ Drug Misuse: Psychosocial Interventions .” National Clinical Practice Guideline 51, NICE , London.
- Parsonage M, Fossey M, Tutty C. 2012. Liaison Psychiatry in the Modern NHS . London: Centre for Mental Health.
- Patel V. 2011. “ Traditional Healers for Mental Health Care in Africa .” Global Health Action 4. doi:10.3402/gha.v4i0.7956. [ PMC free article : PMC3150105 ] [ PubMed : 21845145 ]
- Patel V, Belkin G S, Chockalingam A, Cooper J, Saxena S. others. 2013. “ Grand Challenges: Integrating Mental Health Services into Priority Health Care Platforms .” PLoS Medicine 10 (5): e1001448. doi:10.1371/journal.pmed.1001448. [ PMC free article : PMC3666874 ] [ PubMed : 23737736 ]
- Patel V, Thornicroft G. 2009. “ Packages of Care for Mental, Neurological, and Substance Use Disorders in Low- and Middle-Income Countries: PLoS Medicine Series .” PLoS Medicine 6 (10): e1000160. [ PMC free article : PMC2747279 ] [ PubMed : 19806180 ]
- Patel V, Weiss H A, Chowdhary N, Naik S, Pednekar S. others. 2010. “ Effectiveness of an Intervention Led by Lay Health Counsellors for Depressive and Anxiety Disorders in Primary Care in Goa, India (MANAS): A Cluster Randomised Controlled Trial .” The Lancet 376 (9758): 2086–95. [ PMC free article : PMC4964905 ] [ PubMed : 21159375 ]
- Peters D H, Adam T, Alonge O, Agyepong I A, Tran N. 2013. “ Implementation Research: What It Is and How to Do It .” BMJ 347: f6753. doi:10.1136/bmj.f6753. [ PubMed : 24259324 ]
- Petersen I, Evans-Lacko S, Semrau M, Barry M, Chisholm D, Gronholm P, Egbe C, Thornicroft G. 2015. “ Population- and Community-Level Platforms .” In Disease Control Priorities (third edition): Volume 4, Mental, Neurological, and Substance Use Disorders , edited by Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora M E, editors. . Washington, DC: World Bank.
- Pistrang N, Barker C, Humphreys K. 2008. “ Mutual Help Groups for Mental Health Problems: A Review of Effectiveness Studies .” American Journal of Community Psychology 42 (1–2): 110–21. doi:10.1007/s10464-008-9181-0. [ PubMed : 18679792 ]
- Prince M, Acosta D, Castro-Costa E, Jackson J, Shaji K. 2009. “ Packages of Care for Dementia in Low- and Middle-Income Countries .” PLoS Medicine 6 (11): e1000176. [ PMC free article : PMC2766257 ] [ PubMed : 19888456 ]
- Prince M, Patel V, Saxena S, Maj M, Maselko J. others. 2007. “ No Health without Mental Health .” The Lancet 370 (9590): 859–77. [ PubMed : 17804063 ]
- Proctor E K, Landsverk J, Aarons G, Chambers D, Glisson C. others. 2009. “ Implementation Research in Mental Health Services: An Emerging Science with Conceptual, Methodological, and Training Challenges .” Administration and Policy in Mental Health 36 (1): 24–34. doi:10.1007/s10488-008-0197-4. [ PMC free article : PMC3808121 ] [ PubMed : 19104929 ]
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. 2008. “ Cognitive Behaviour Therapy–Based Intervention by Community Health Workers for Mothers with Depression and Their Infants in Rural Pakistan: A Cluster-Randomised Controlled Trial .” The Lancet 372 (9642): 902–09. [ PMC free article : PMC2603063 ] [ PubMed : 18790313 ]
- Rahman A, Surkan P J, Cayetano C E, Rwagatare P, Dickson K E. 2013. “ Grand Challenges: Integrating Maternal Mental Health into Maternal and Child Health Programmes .” PLoS Medicine 10 (5): e1001442. doi:10.1371/journal.pmed.1001442. [ PMC free article : PMC3646722 ] [ PubMed : 23667345 ]
- Rojas G, Fritsch R, Solis J, Jadresic E, Castillo C. others. 2007. “ Treatment of Postnatal Depression in Low-Income Mothers in Primary-Care Clinics in Santiago, Chile: A Randomised Controlled Trial .” The Lancet 370 (9599): 1629–37. doi:10.1016/S0140-6736(07)61685-7. [ PubMed : 17993363 ]
- Savigny D, Adam T. eds. 2009. Systems Thinking for Health Systems Strengthening . Geneva: World Health Organization.
- Shidhaye R, Kermode M. 2013. “ Stigma and Discrimination as a Barrier to Mental Health Service Utilization in India .” International Health 5 (1): 6–8. doi:10.1093/inthealth/ihs011. [ PubMed : 24029838 ]
- Simoni J M, Franks J C, Lehavot K, Yard S S. 2011. “ Peer Interventions to Promote Health: Conceptual Considerations .” American Journal of Orthopsychiatry 81 (3): 351–59. doi:10.1111/j.1939-0025.2011.01103.x. [ PMC free article : PMC3607369 ] [ PubMed : 21729015 ]
- Sphere. 2011. Humanitarian Charter and Minimum Standards in Disaster Response . Geneva: Sphere Project.
- Steiner T J, Antonaci F, Jensen R, Lainez M J, Lanteri-Minet M. others. 2011. “ Recommendations for Headache Service Organisation and Delivery in Europe .” Journal of Headache Pain 12 (4): 419–26. doi:10.1007/s10194-011-0320-x. [ PMC free article : PMC3139057 ] [ PubMed : 21380555 ]
- Thakur K, Albanese E, Giannakopoulos P, Jette N, Linde M, Prince M, Steiner T, Dua T. 2015. “ Neurological Disorders .” In Disease Control Priorities (third edition): Volume 4, Mental, Neurological, and Substance Use Disorders , edited by Patel V, Chisholm D, Dua T, Laxminarayan R, Medina-Mora M E, editors. . Washington, DC: World Bank.
- The Health Foundation. 2013. Quality Improvement Made Simple . London: The Health Foundation.
- Thornicroft G, Tansella M. 2013. “ The Balanced Care Model for Global Mental Health .” Psychological Medicine 43 (4): 849–63. doi:10.1017/S0033291712001420. [ PubMed : 22785067 ]
- Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J. others. 2010. “ Effect of a Participatory Intervention with Women’s Groups on Birth Outcomes and Maternal Depression in Jharkhand and Orissa, India: A Cluster-Randomised Controlled Trial .” The Lancet 375 (9721): 1182–92. [ PubMed : 20207411 ]
- van Ginneken N, Tharyan P, Lewin W, Rao G N, Meera S M. others. 2013. “ Non-Specialist Health Worker Interventions for the Care of Mental, Neurological and Substance-Abuse Disorders in Low- and Middle-Income Countries .” Cochrane Database of Systematic Reviews 11: CD009149. doi:10.1002/14651858.CD009149.pub2. [ PubMed : 24249541 ]
- Walker E R, Barmon C, McGee R E, Engelhard G, Sterk C E. others. 2014. “ Perspectives of Adults with Epilepsy and Their Support Persons on Self-Management Support .” Qualitative Health Research 24 (11): 1553–66. doi:10.1177/1049732314548880. [ PMC free article : PMC4623566 ] [ PubMed : 25192759 ]
- WHO (World Health Organization). 2002. Traditional Medicine: Growing Needs and Potential . Geneva: WHO.
- WHO (World Health Organization). 2003a. “ Organization of Services for Mental Health .” In Mental Health Policy and Service Guidance Package . Geneva: WHO.
- WHO (World Health Organization). 2003b. “ Quality Improvement for Mental Health .” In Mental Health Policy and Service Guidance Package . Geneva: WHO.
- WHO (World Health Organization). 2010a. The World Health Report 2010: Health Systems Financing: The Path to Universal Coverage . Geneva: WHO.
- WHO (World Health Organization). 2010b. mhGAP Intervention Guide for Mental, Neurological and Substance Use Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme (mhGAP) . Geneva: WHO. [ PubMed : 23741783 ]
- WHO (World Health Organization). 2012. WHO QualityRights Toolkit . Geneva: WHO.
- WHO (World Health Organization). 2013a. Building Back Better: Sustainable Mental Health Care after Emergencies . WHO: Geneva.
- WHO (World Health Organization). 2013b. “ HIV Service Delivery [Internet] .” http://www .who.int/hiv /topics/capacity/imai/en/index.html .
- WHO and Calouste Gulbenkian Foundation. 2014. Integrating the Response to Mental Disorders and Other Chronic Diseases in Health Care Systems . Geneva: WHO.
- WHO and WONCA (World Organization of Family Doctors). 2008. Integrating Mental Health in Primary Care: A Global Perspective . Geneva: WHO.
- Yu S, Zhang M, Zhou J, Liu R, Wan Q. others. 2014. “ Headache Care in China .” Headache: The Journal of Head and Face Pain 54 (4): 601–09. doi:10.1111/head.12330.
Disclaimer: Dan Chisholm is a staff member of the World Health Organization. The author alone is responsible for the views expressed in this publication, and they do not necessarily represent the decisions, policy, or views of the World Health Organization.
This chapter was previously published as an article by R. Shidhaye, C. Lund, and D. Chisholm, titled “Closing the Treatment Gap for Mental, Neurological, and Substance Use Disorders by Strengthening Existing Health Care Platforms: Strategies for Delivery and Integration of Evidence-Based Interventions.” International Journal of Mental Health Systems , 2015: 9 (40). doi:10.1186/s13033-015-0031-9.
- Low-income countries (LICs) = US$1,045 or less
- Middle-income countries (MICs) are subdivided: a) Lower-middle-income = US$1,046 to US$4,125 b) Upper-middle-income (UMICs) = US$4,126 to US$12,745
- High-income countries (HICs) = US$12,746 or more.
This work is available under the Creative Commons Attribution 3.0 IGO license (CC BY 3.0 IGO) http://creativecommons.org/licenses/by/3.0/igo . Under the Creative Commons Attribution license, you are free to copy, distribute, transmit, and adapt this work, including for commercial purposes, under the following conditions:
Attribution —Please cite the work as follows: Patel, V., D. Chisholm., T. Dua, R. Laxminarayan, and M. E. Medina-Mora, editors. 2015. Mental, Neurological, and Substance Use Disorders . Disease Control Priorities, third edition, volume 4. Washington, DC: World Bank. doi:10.1596/978-1-4648-0426-7. License: Creative Commons Attribution CC BY 3.0 IGO
Translations —If you create a translation of this work, please add the following disclaimer along with the attribution: This translation was not created by The World Bank and should not be considered an official World Bank translation. The World Bank shall not be liable for any content or error in this translation .
Third-party content —The World Bank does not necessarily own each component of the content contained within the work. The World Bank therefore does not warrant that the use of any third-party-owned individual component or part contained in the work will not infringe on the rights of those third parties. The risk of claims resulting from such infringement rests solely with you. If you wish to re-use a component of the work, it is your responsibility to determine whether permission is needed for that re-use and to obtain permission from the copyright owner. Examples of components can include, but are not limited to, tables, figures, or images.
All queries on rights and licenses should be addressed to the Publishing and Knowledge Division, The World Bank, 1818 H Street NW, Washington, DC 20433, USA; fax: 202-522-2625; e-mail: gro.knabdlrow@sthgirbup .
- Cite this Page Shidhaye R, Lund C, Chisholm D. Health Care Platform Interventions. In: Patel V, Chisholm D, Dua T, et al., editors. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2016 Mar 14. Chapter 11. doi: 10.1596/978-1-4648-0426-7_ch11
- PDF version of this title (4.2M)
In this Page
Related information.
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Cost-Effectiveness and Affordability of Interventions, Policies, and Platforms for the Prevention and Treatment of Mental, Neurological, and Substance Use Disorders. [Mental, Neurological, and Subs...] Review Cost-Effectiveness and Affordability of Interventions, Policies, and Platforms for the Prevention and Treatment of Mental, Neurological, and Substance Use Disorders. Levin C, Chisholm D. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4). 2016 Mar 14
- Review Global Priorities for Addressing the Burden of Mental, Neurological, and Substance Use Disorders. [Mental, Neurological, and Subs...] Review Global Priorities for Addressing the Burden of Mental, Neurological, and Substance Use Disorders. Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, Ferrari AJ, Hyman S, Laxminarayan R, Levin C, et al. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4). 2016 Mar 14
- Review Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. [Lancet. 2016] Review Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Patel V, Chisholm D, Parikh R, Charlson FJ, Degenhardt L, Dua T, Ferrari AJ, Hyman S, Laxminarayan R, Levin C, et al. Lancet. 2016 Apr 16; 387(10028):1672-85. Epub 2015 Oct 8.
- Review Population and Community Platform Interventions. [Mental, Neurological, and Subs...] Review Population and Community Platform Interventions. Petersen I, Evans-Lacko S, Semrau M, Barry M, Chisholm D, Gronholm P, Egbe CO, Thornicroft G. Mental, Neurological, and Substance Use Disorders: Disease Control Priorities, Third Edition (Volume 4). 2016 Mar 14
- Review Closing the treatment gap for mental, neurological and substance use disorders by strengthening existing health care platforms: strategies for delivery and integration of evidence-based interventions. [Int J Ment Health Syst. 2015] Review Closing the treatment gap for mental, neurological and substance use disorders by strengthening existing health care platforms: strategies for delivery and integration of evidence-based interventions. Shidhaye R, Lund C, Chisholm D. Int J Ment Health Syst. 2015; 9:40. Epub 2015 Dec 30.
Recent Activity
- Health Care Platform Interventions - Mental, Neurological, and Substance Use Dis... Health Care Platform Interventions - Mental, Neurological, and Substance Use Disorders
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Yekaterinburg Tourism
- Yekaterinburg Hotels
- Yekaterinburg Bed and Breakfast
- Flights to Yekaterinburg
- Things to Do in Yekaterinburg
- Yekaterinburg Travel Forum
- Yekaterinburg Photos
- Yekaterinburg Map
- All Yekaterinburg Hotels
- Yekaterinburg Hotel Deals
- Yekaterinburg
- Things to Do
- Restaurants
- Vacation Rentals
- Travel Stories
- Rental Cars
- Add a Place
- Travel Forum
- Travelers' Choice
- Help Center
A bit pretentious. - Case
- Europe
- Russia
- Urals District
- Sverdlovsk Oblast
- Yekaterinburg
- Yekaterinburg Restaurants
“A bit pretentious.” Review of Case
Why can't this place just be what it is. That is, an ok restaurant in a city centre business hotel. Rather dull jazz, small portions, decor from I don't know when and high prices. If they could just relax a bit, not pretend to be in the Ritz and look at the prices then they would do a lot better. Service is willing and the food - what there is of it - is ok.
- Excellent 2
- Very good 3
- All languages
- English (1)
- Russian (5)
- English (1)
- Russian (5)
1 - 5 of 6 reviews
Travelers who viewed Case also viewed
Been to case share your experiences, owners: what's your side of the story.
Own or manage this property? Claim your listing for free to respond to reviews, update your profile and much more.
Viewed restaurants
Browse nearby.
- All health topics
Popular topics
- Communicable Diseases Department
- Vaccine preventable disease
- Department of Healthier Populations and Noncommunicable Diseases (HPN)
- Universal health coverage
- Research and Innovation
- Planning, Monitoring and Evaluation
- Publications
- News releases
- Media Statements
- Feature stories
- Opinion Editorials
- World Health Day 2024
- Emergency Operations
- Country Health Emergency Preparedness & IHR
- Infectious Hazard Management
- Health Emergency Information & Risk Assessment
- Public health Laboratory services
- Regional Strategic Roadmap for Health Security (2023-2027) endorsed by the Regional Committee
- Nepal Earthquake
- Thailand becomes first in SEAR with WHO classified emergency medical team
- Where we work
- Country Strategy and Support
- Regional Director
- Regional Committee
- Seventy-sixth Session of the Regional Committee
- Collaborating Centers
Health officials, partners, and experts meet to strategize scale-up of regional innovations for improving quality integrated primary health care
Health officials, development partners, and experts met this week to strategize scaling up of innovations to improve quality integrated primary health care at a Regional Workshop here. Participants reviewed successful models from across the WHO South-East Asia Region, specifically explored innovations related to National PHC Integration in Indonesia, and collectively identified steps forward for improving both quality and integration in healthcare delivery.
“Poor quality care is today, a greater barrier to reducing mortality in low-and middle-income countries than insufficient access,” said Saima Wazed, Regional Director, WHO South-East Asia, in her inaugural address at the ‘Regional Workshop on Innovations for Quality Integrated Primary Health Care.’ She emphasized that as a key aspect of quality, the integration of primary health services is crucial for providing seamless care throughout an individual’s life.
“Integration through ensuring service continuity and people-centredness is a key determinant of quality,” the Regional Director added.

(Photo credit: WHO Indonesia)
The World Health Organization is urging countries in the WHO South-East Asia Region to expand the adoption of cutting-edge policies, practices, and technologies that provide comprehensive, quality care throughout all stages of life. This call-to-action highlights successful models from across the Region, aimed at tackling the increasing challenges of noncommunicable diseases (NCDs), mental health, public health emergencies, and climate effects alongside traditional priorities in service delivery.
The WHO South-East Asia Region has long recognized primary health care as the foundation of robust health systems and broader development goals. In 2023, health ministers from the Region reaffirmed their commitment to prioritizing investments in primary health care. The South-East Asia Region Primary Health Care Strategy 2022-2030 outlines key actions to transform health systems through a primary health care approach.
The recently launched WHO South-East Asia Regional Roadmap for Results and Resilience, underscores WHO’s commitment to building a learning health system that prioritises innovations, equity, and sustainability . The holistic approach aims to ensure health and well-being for all in a comprehensive manner. With WHO serving as a key enabler , the roadmap seeks to forge partnerships across governments, development agencies, philanthropic organizations, academia, the private sector, and civil society to achieve universal health coverage.
According to the Lancet Commission, nearly 60% of the 8.6 million annual deaths from treatable conditions are linked to poor quality care. During the COVID-19 pandemic, the lack of integration of public health functions in primary health care posed a significant bottleneck, in prevention, preparedness, and response. It also underscored the urgent need to strengthen primary health care systems while integrating essential public health functions in the Region for better preparedness and resilience against future health crises.
Addressing the diverse challenges in delivering quality integrated primary health care to the Region’s two billion people, the Regional Director said, “We stand at a historic moment in time. A remarkable transformation is taking place across our countries in our Region: a transformation from a focus on a few select diseases to that of the full human condition, across the life course.”A compilation of “Positive Practice Case Stories” was launched, featuring a set of 20 case studies from across the Region that highlight innovative approaches and solutions in various countries.

“My vision for our Region is where people have access to quality healthcare, regardless of where they live, and regardless of their income or social status. I would like us to be a Region which takes a holistic approach to health and well-being; where people are empowered - both physically and mentally - to achieve their full potential. I would like to shape a Region which cares for all and strengthens and protects the most vulnerable who live in it.” the Regional Director said.
To read more about the ‘ Positive practices in developing primary healthcare-oriented health systems’ scan the QR code below or click the link here

1 Distance Learning Programs in Health Care in Yekaterinburg, Russia for 2024
- Health Care
- Distance Learning
Health Care (1)
- Mental Healthcare (1)
- Neuroscience Studies (1)
- Back to main category
- United Kingdom (0)
- Australia (0)
- Bachelor (0)
- Certificate (0)
- Diploma (0)
- Associate Degree (0)
- Associate of Applied Science (0)
- Associate of Science (0)
- Pre-Med (0)
- Pre-Vet (0)
- Associate of Arts (0)
- Pre-Nurse (0)
- 2 years (1)
- 3 years (0)
- 4+ years (0)
- Full time (1)
- Part time (0)
- English (1)
- Spanish (0)
- Portuguese (0)
- Italian (0)
- On-Campus (1)
- Distance Learning (1)
- Blended (1)
- Mental Healthcare
- Neuroscience Studies
Popular degree type
Popular study format
Popular education type

COMMENTS
Unit 5: Meeting Individual Care and Support Needs Care Study 1: Valerie B. aged 24 years Valerie B. was admitted to the community hospital, following surgery for her appendix which burst before she could reach hospital. Valerie has mental health problems which began when her parents died when she was six years old.
Base your work on each individual in the case studies The report will demonstrate your understanding of the issues involved in meeting the needs of individuals who have diverse needs, preparing you for work experience. All of the individuals in the attached case studies, have needs that require particular support.
The social worker has arranged for Maria to have support from a community care assistant, who will help her mother with dressing and personal care during the day, and a night sitter once a week, to allow Maria an undisturbed night.
In the example, in the case of responses, 1, 3 and 4, the learner has correctly identified three factors from the case study that would have a negative effect on the health and wellbeing of Brian and then progressed to giving good explanations. Comments on content Response 2 was insufficient for two marks.
The case study outlines Porbandar's population, famous sites like temples and palaces, local cuisine, and concludes that Porbandar is developing as a city with improving infrastructure and growing industries.
presented research paper " A study on female Tamasha artists from pune district." In Annual research conference of B.J.Medical College Pune 2006 and was awarded first prize. Research Interests: Indeed TB is a social disease with so many social problems especially the women suffering from TB/HIV undergoes a pathetic life situation.
This is an example for an assignment in health and social care. case study valerie aged 24 years valerie was admitted to the community hospital, following
Bhatia has always been motivated by human disease and drawn to global health, in part because of her early experiences. As a child, Bhatia went with her aunt, a physician, to a local clinic during summer visits to India. There, she observed medical care in a low-resource community, an experience that has resonated with her throughout her life. She witnessed firsthand the differences in cancer ...
Case studies from Australia, Brazil, and South Africa have demonstrated that a collaborative stepped care approach in which joint consultations and interventions occur between primary care workers and mental health specialists increases the skills of primary care workers and builds mental health networks [ 16 ].
Introduction: International policies and legislation set a precedence of person-centred sustainable integrated Health and Social Care (HSC) that meets the health and wellbeing needs of service users through improved experiences. However, current research focuses on service models, with fewer studies investigating experiences and needs.
Birch View is a residential care home in Wales. It caters for older people, lots of whom have dementia. Many of the individuals living in Birch View speak Welsh and the home tries to employ care and support workers who speak both Welsh and English.
Background Equitable access to healthcare for rural, tribal, and underprivileged people has been an emerging area of interest for researchers, academicians, and policymakers worldwide. Improving equitable access to healthcare requires innovative interventions. This calls for clarifying which operational model of a service innovation needs to be strengthened to achieve transformative change and ...
Integrated care is pursued globally as a strategy to manage health and social care resources more effectively. It offers the promise of meeting increasingly complex needs, particularly those of aging populations, in a person-centred, co-ordinated way that addresses fragmentation and improves quality.
Improving person-centred care communication in health and social care settings PHD STUDENT: Natalia Rodriguez UNIVERSITY: Heriot-Watt COMPANY: Healthcare Improvement Scotland In January 2019 Healthcare Improvement Scotland welcomed Natalia Rodriguez to undertake a 3 month internship.
This is an example for an assignment in health and social care. case study valerie aged 24 years valerie was admitted to the community hospital, following
Lack of support (obstacles / barriers) From family, friends and professionals. Physical health (obstacles/barriers) Disability, chronic illnesses/disease. Barriers to access. Location, anxiety or fears. Study with Quizlet and memorise flashcards containing terms like Blood pressure, Type 2 Diabetes, BMI (body mass index) and others.
Case study 1. Increasing awareness of bowel cancer symptoms among the Asian Community -NHS Hillingdon Clinical Commissioning Group (Formerly NHS Hillingdon) This case study illustrates the benefits of collecting and using equality information to identify the needs of people with particular protected characteristics and to measure progress in ...
1 0 Health and Social Care Unit 7: Princ iples of Safe Practice in Health and Social Care Adult Case Study Merryvale Residence
Abstract This is a reflection on how deprivation of citizenship can create different classes of citizenship and can (symbolically) destabilise social cohesion. The Netherlands is used as a case study to exemplify this. This paper critically analyses three aspects that can contribute to the erosion of equal and unconditional citizenship. First, tensions at state level in the implementation of ...
Case Study. Department of Health and Social Care introduces Scan4Safety to revolutionise patient care. Scroll. Key Results. GS1 standards allow clinical staff to build a complete patient picture that is easily accessible. Increased data visibility can aid efficiencies in catalogue management and staffing. The problem.
Chapter 10 of this volume () considers the evidence relating to interventions that improve mental health at the population and community levels. This chapter outlines the main elements and features of a health care platform and its delivery channels, namely, informal health care, primary health care, and specialized services.
Case: A bit pretentious. - See 6 traveler reviews, candid photos, and great deals for Yekaterinburg, Russia, at Tripadvisor.
The South-East Asia Region Primary Health Care Strategy 2022-2030 outlines key actions to transform health systems through a primary health care approach. ... featuring a set of 20 case studies from across the Region that highlight innovative approaches and solutions in various countries.(Photo credit: WHO Indonesia)"My vision for our Region ...
1 Distance Learning Programs in Health Care in Yekaterinburg, Russia for 2024. Filters. Filters Reset. Health Care; Distance Learning; Fields of study. Health Care (1) Mental Healthcare (1) Neuroscience Studies (1) Back to main category; Locations. USA (0) United Kingdom (0) Spain (0) Canada (0) South Africa (0) + Show more locations. Find more ...