Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- Ethical Considerations in Research | Types & Examples

Ethical Considerations in Research | Types & Examples
Published on October 18, 2021 by Pritha Bhandari . Revised on May 9, 2024.
Ethical considerations in research are a set of principles that guide your research designs and practices. Scientists and researchers must always adhere to a certain code of conduct when collecting data from people.
The goals of human research often include understanding real-life phenomena, studying effective treatments, investigating behaviors, and improving lives in other ways. What you decide to research and how you conduct that research involve key ethical considerations.
These considerations work to
- protect the rights of research participants
- enhance research validity
- maintain scientific or academic integrity
Table of contents
Why do research ethics matter, getting ethical approval for your study, types of ethical issues, voluntary participation, informed consent, confidentiality, potential for harm, results communication, examples of ethical failures, other interesting articles, frequently asked questions about research ethics.
Research ethics matter for scientific integrity, human rights and dignity, and collaboration between science and society. These principles make sure that participation in studies is voluntary, informed, and safe for research subjects.
You’ll balance pursuing important research objectives with using ethical research methods and procedures. It’s always necessary to prevent permanent or excessive harm to participants, whether inadvertent or not.
Defying research ethics will also lower the credibility of your research because it’s hard for others to trust your data if your methods are morally questionable.
Even if a research idea is valuable to society, it doesn’t justify violating the human rights or dignity of your study participants.
Prevent plagiarism. Run a free check.
Before you start any study involving data collection with people, you’ll submit your research proposal to an institutional review board (IRB) .
An IRB is a committee that checks whether your research aims and research design are ethically acceptable and follow your institution’s code of conduct. They check that your research materials and procedures are up to code.
If successful, you’ll receive IRB approval, and you can begin collecting data according to the approved procedures. If you want to make any changes to your procedures or materials, you’ll need to submit a modification application to the IRB for approval.
If unsuccessful, you may be asked to re-submit with modifications or your research proposal may receive a rejection. To get IRB approval, it’s important to explicitly note how you’ll tackle each of the ethical issues that may arise in your study.
There are several ethical issues you should always pay attention to in your research design, and these issues can overlap with each other.
You’ll usually outline ways you’ll deal with each issue in your research proposal if you plan to collect data from participants.
| Voluntary participation | Your participants are free to opt in or out of the study at any point in time. |
|---|---|
| Informed consent | Participants know the purpose, benefits, risks, and funding behind the study before they agree or decline to join. |
| Anonymity | You don’t know the identities of the participants. Personally identifiable data is not collected. |
| Confidentiality | You know who the participants are but you keep that information hidden from everyone else. You anonymize personally identifiable data so that it can’t be linked to other data by anyone else. |
| Potential for harm | Physical, social, psychological and all other types of harm are kept to an absolute minimum. |
| Results communication | You ensure your work is free of or research misconduct, and you accurately represent your results. |
Voluntary participation means that all research subjects are free to choose to participate without any pressure or coercion.
All participants are able to withdraw from, or leave, the study at any point without feeling an obligation to continue. Your participants don’t need to provide a reason for leaving the study.
It’s important to make it clear to participants that there are no negative consequences or repercussions to their refusal to participate. After all, they’re taking the time to help you in the research process , so you should respect their decisions without trying to change their minds.
Voluntary participation is an ethical principle protected by international law and many scientific codes of conduct.
Take special care to ensure there’s no pressure on participants when you’re working with vulnerable groups of people who may find it hard to stop the study even when they want to.
Informed consent refers to a situation in which all potential participants receive and understand all the information they need to decide whether they want to participate. This includes information about the study’s benefits, risks, funding, and institutional approval.
You make sure to provide all potential participants with all the relevant information about
- what the study is about
- the risks and benefits of taking part
- how long the study will take
- your supervisor’s contact information and the institution’s approval number
Usually, you’ll provide participants with a text for them to read and ask them if they have any questions. If they agree to participate, they can sign or initial the consent form. Note that this may not be sufficient for informed consent when you work with particularly vulnerable groups of people.
If you’re collecting data from people with low literacy, make sure to verbally explain the consent form to them before they agree to participate.
For participants with very limited English proficiency, you should always translate the study materials or work with an interpreter so they have all the information in their first language.
In research with children, you’ll often need informed permission for their participation from their parents or guardians. Although children cannot give informed consent, it’s best to also ask for their assent (agreement) to participate, depending on their age and maturity level.
Anonymity means that you don’t know who the participants are and you can’t link any individual participant to their data.
You can only guarantee anonymity by not collecting any personally identifying information—for example, names, phone numbers, email addresses, IP addresses, physical characteristics, photos, and videos.
In many cases, it may be impossible to truly anonymize data collection . For example, data collected in person or by phone cannot be considered fully anonymous because some personal identifiers (demographic information or phone numbers) are impossible to hide.
You’ll also need to collect some identifying information if you give your participants the option to withdraw their data at a later stage.
Data pseudonymization is an alternative method where you replace identifying information about participants with pseudonymous, or fake, identifiers. The data can still be linked to participants but it’s harder to do so because you separate personal information from the study data.
Confidentiality means that you know who the participants are, but you remove all identifying information from your report.
All participants have a right to privacy, so you should protect their personal data for as long as you store or use it. Even when you can’t collect data anonymously, you should secure confidentiality whenever you can.
Some research designs aren’t conducive to confidentiality, but it’s important to make all attempts and inform participants of the risks involved.
As a researcher, you have to consider all possible sources of harm to participants. Harm can come in many different forms.
- Psychological harm: Sensitive questions or tasks may trigger negative emotions such as shame or anxiety.
- Social harm: Participation can involve social risks, public embarrassment, or stigma.
- Physical harm: Pain or injury can result from the study procedures.
- Legal harm: Reporting sensitive data could lead to legal risks or a breach of privacy.
It’s best to consider every possible source of harm in your study as well as concrete ways to mitigate them. Involve your supervisor to discuss steps for harm reduction.
Make sure to disclose all possible risks of harm to participants before the study to get informed consent. If there is a risk of harm, prepare to provide participants with resources or counseling or medical services if needed.
Some of these questions may bring up negative emotions, so you inform participants about the sensitive nature of the survey and assure them that their responses will be confidential.
The way you communicate your research results can sometimes involve ethical issues. Good science communication is honest, reliable, and credible. It’s best to make your results as transparent as possible.
Take steps to actively avoid plagiarism and research misconduct wherever possible.
Plagiarism means submitting others’ works as your own. Although it can be unintentional, copying someone else’s work without proper credit amounts to stealing. It’s an ethical problem in research communication because you may benefit by harming other researchers.
Self-plagiarism is when you republish or re-submit parts of your own papers or reports without properly citing your original work.
This is problematic because you may benefit from presenting your ideas as new and original even though they’ve already been published elsewhere in the past. You may also be infringing on your previous publisher’s copyright, violating an ethical code, or wasting time and resources by doing so.
In extreme cases of self-plagiarism, entire datasets or papers are sometimes duplicated. These are major ethical violations because they can skew research findings if taken as original data.
You notice that two published studies have similar characteristics even though they are from different years. Their sample sizes, locations, treatments, and results are highly similar, and the studies share one author in common.
Research misconduct
Research misconduct means making up or falsifying data, manipulating data analyses, or misrepresenting results in research reports. It’s a form of academic fraud.
These actions are committed intentionally and can have serious consequences; research misconduct is not a simple mistake or a point of disagreement about data analyses.
Research misconduct is a serious ethical issue because it can undermine academic integrity and institutional credibility. It leads to a waste of funding and resources that could have been used for alternative research.
Later investigations revealed that they fabricated and manipulated their data to show a nonexistent link between vaccines and autism. Wakefield also neglected to disclose important conflicts of interest, and his medical license was taken away.
This fraudulent work sparked vaccine hesitancy among parents and caregivers. The rate of MMR vaccinations in children fell sharply, and measles outbreaks became more common due to a lack of herd immunity.
Research scandals with ethical failures are littered throughout history, but some took place not that long ago.
Some scientists in positions of power have historically mistreated or even abused research participants to investigate research problems at any cost. These participants were prisoners, under their care, or otherwise trusted them to treat them with dignity.
To demonstrate the importance of research ethics, we’ll briefly review two research studies that violated human rights in modern history.
These experiments were inhumane and resulted in trauma, permanent disabilities, or death in many cases.
After some Nazi doctors were put on trial for their crimes, the Nuremberg Code of research ethics for human experimentation was developed in 1947 to establish a new standard for human experimentation in medical research.
In reality, the actual goal was to study the effects of the disease when left untreated, and the researchers never informed participants about their diagnoses or the research aims.
Although participants experienced severe health problems, including blindness and other complications, the researchers only pretended to provide medical care.
When treatment became possible in 1943, 11 years after the study began, none of the participants were offered it, despite their health conditions and high risk of death.
Ethical failures like these resulted in severe harm to participants, wasted resources, and lower trust in science and scientists. This is why all research institutions have strict ethical guidelines for performing research.
If you want to know more about statistics , methodology , or research bias , make sure to check out some of our other articles with explanations and examples.
- Normal distribution
- Measures of central tendency
- Chi square tests
- Confidence interval
- Quartiles & Quantiles
- Cluster sampling
- Stratified sampling
- Thematic analysis
- Cohort study
- Peer review
- Ethnography
Research bias
- Implicit bias
- Cognitive bias
- Conformity bias
- Hawthorne effect
- Availability heuristic
- Attrition bias
- Social desirability bias
Ethical considerations in research are a set of principles that guide your research designs and practices. These principles include voluntary participation, informed consent, anonymity, confidentiality, potential for harm, and results communication.
Scientists and researchers must always adhere to a certain code of conduct when collecting data from others .
These considerations protect the rights of research participants, enhance research validity , and maintain scientific integrity.
Research ethics matter for scientific integrity, human rights and dignity, and collaboration between science and society. These principles make sure that participation in studies is voluntary, informed, and safe.
Anonymity means you don’t know who the participants are, while confidentiality means you know who they are but remove identifying information from your research report. Both are important ethical considerations .
You can only guarantee anonymity by not collecting any personally identifying information—for example, names, phone numbers, email addresses, IP addresses, physical characteristics, photos, or videos.
You can keep data confidential by using aggregate information in your research report, so that you only refer to groups of participants rather than individuals.
These actions are committed intentionally and can have serious consequences; research misconduct is not a simple mistake or a point of disagreement but a serious ethical failure.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Bhandari, P. (2024, May 09). Ethical Considerations in Research | Types & Examples. Scribbr. Retrieved August 22, 2024, from https://www.scribbr.com/methodology/research-ethics/
Is this article helpful?

Pritha Bhandari
Other students also liked, data collection | definition, methods & examples, what is self-plagiarism | definition & how to avoid it, how to avoid plagiarism | tips on citing sources, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
- The Open University
- Accessibility hub
- Guest user / Sign out
- Study with The Open University
My OpenLearn Profile
Personalise your OpenLearn profile, save your favourite content and get recognition for your learning

Addressing ethical issues in your research proposal
This article explores the ethical issues that may arise in your proposed study during your doctoral research degree.
What ethical principles apply when planning and conducting research?
Research ethics are the moral principles that govern how researchers conduct their studies (Wellcome Trust, 2014). As there are elements of uncertainty and risk involved in any study, every researcher has to consider how they can uphold these ethical principles and conduct the research in a way that protects the interests and welfare of participants and other stakeholders (such as organisations).
You will need to consider the ethical issues that might arise in your proposed study. Consideration of the fundamental ethical principles that underpin all research will help you to identify the key issues and how these could be addressed. As you are probably a practitioner who wants to undertake research within your workplace, consider how your role as an ‘insider’ influences how you will conduct your study. Think about the ethical issues that might arise when you become an insider researcher (for example, relating to trust, confidentiality and anonymity).
What key ethical principles do you think will be important when planning or conducting your research, particularly as an insider? Principles that come to mind might include autonomy, respect, dignity, privacy, informed consent and confidentiality. You may also have identified principles such as competence, integrity, wellbeing, justice and non-discrimination.
Key ethical issues that you will address as an insider researcher include:
- Gaining trust
- Avoiding coercion when recruiting colleagues or other participants (such as students or service users)
- Practical challenges relating to ensuring the confidentiality and anonymity of organisations and staff or other participants.
(Heslop et al, 2018)
A fuller discussion of ethical principles is available from the British Psychological Society’s Code of Human Research Ethics (BPS, 2021).
You can also refer to guidance from the British Educational Research Association and the British Association for Applied Linguistics .

Ethical principles are essential for protecting the interests of research participants, including maximising the benefits and minimising any risks associated with taking part in a study. These principles describe ethical conduct which reflects the integrity of the researcher, promotes the wellbeing of participants and ensures high-quality research is conducted (Health Research Authority, 2022).
Research ethics is therefore not simply about gaining ethical approval for your study to be conducted. Research ethics relates to your moral conduct as a doctoral researcher and will apply throughout your study from design to dissemination (British Psychological Society, 2021). When you apply to undertake a doctorate, you will need to clearly indicate in your proposal that you understand these ethical principles and are committed to upholding them.
Where can I find ethical guidance and resources?
Professional bodies, learned societies, health and social care authorities, academic publications, Research Ethics Committees and research organisations provide a range of ethical guidance and resources. International codes such as the Universal Declaration of Human Rights underpin ethical frameworks (United Nations, 1948).
You may be aware of key legislation in your own country or the country where you plan to undertake the research, including laws relating to consent, data protection and decision-making capacity, for example, the Data Protection Act, 2018 (UK). If you want to find out more about becoming an ethical researcher, check out this Open University short course: Becoming an ethical researcher: Introduction and guidance: What is a badged course? - OpenLearn - Open University
You should be able to justify the research decisions you make. Utilising these resources will guide your ethical judgements when writing your proposal and ultimately when designing and conducting your research study. The Ethical Guidelines for Educational Research (British Educational Research Association, 2018) identifies the key responsibilities you will have when you conduct your research, including the range of stakeholders that you will have responsibilities to, as follows:
- to your participants (e.g. to appropriately inform them, facilitate their participation and support them)
- clients, stakeholders and sponsors
- the community of educational or health and social care researchers
- for publication and dissemination
- your wellbeing and development
The National Institute for Health and Care Research (no date) has emphasised the need to promote equality, diversity and inclusion when undertaking research, particularly to address long-standing social and health inequalities. Research should be informed by the diversity of people’s experiences and insights, so that it will lead to the development of practice that addresses genuine need. A commitment to equality, diversity and inclusion aims to eradicate prejudice and discrimination on the basis of an individual or group of individuals' protected characteristics such as sex (gender), disability, race, sexual orientation, in line with the Equality Act 2010.
The NIHR has produced guidance for enhancing the inclusion of ‘under-served groups’ when designing a research study (2020). Although the guidance refers to clinical research it is relevant to research more broadly.
You should consider how you will promote equality and diversity in your planned study, including through aspects such as your research topic or question, the methodology you will use, the participants you plan to recruit and how you will analyse and interpret your data.
What ethical issues do I need to consider when writing my research proposal?

You might be planning to undertake research in a health, social care, educational or other setting, including observations and interviews. The following prompts should help you to identify key ethical issues that you need to bear in mind when undertaking research in such settings.
1. Imagine you are a potential participant. Think about the questions and concerns that you might have:
- How would you feel if a researcher sat in your space and took notes, completed a checklist, or made an audio or film recording?
- What harm might a researcher cause by observing or interviewing you and others?
- What would you want to know about the researcher and ask them about the study before giving consent?
- When imagining you are the participant, how could the researcher make you feel more comfortable to be observed or interviewed?
2. Having considered the perspective of your potential participant, how would you take account of concerns such as privacy, consent, wellbeing and power in your research proposal?
[Adapted from OpenLearn course: Becoming an ethical researcher, Week 2 Activity 3: Becoming an ethical researcher - OpenLearn - Open University ]
The ethical issues to be considered will vary depending on your organisational context/role, the types of participants you plan to recruit (for example, children, adults with mental health problems), the research methods you will use, and the types of data you will collect. You will need to decide how to recruit your participants so you do not inappropriately exclude anyone. Consider what methods may be necessary to facilitate their voice and how you can obtain their consent to taking part or ensure that consent is obtained from someone else as necessary, for example, a parent in the case of a child.
You should also think about how to avoid imposing an unnecessary burden or costs on your participants. For example, by minimising the length of time they will have to commit to the study and by providing travel or other expenses. Identify the measures that you will take to store your participants’ data safely and maintain their confidentiality and anonymity when you report your findings. You could do this by storing interview and video recordings in a secure server and anonymising their names and those of their organisations using pseudonyms.
Professional codes such as the Code of Human Research Ethics (BPS, 2021) provide guidance on undertaking research with children. Being an ‘insider’ researching within your own organisation has advantages. However, you should also consider how this might impact on your research, such as power dynamics, consent, potential bias and any conflict of interest between your professional and researcher roles (Sapiro and Matthews, 2020).
How have other researchers addressed any ethical challenges?
The literature provides researchers’ accounts explaining how they addressed ethical challenges when undertaking studies. For example, Turcotte-Tremblay and McSween-Cadieux (2018) discuss strategies for protecting participants’ confidentiality when disseminating findings locally, such as undertaking fieldwork in multiple sites and providing findings in a generalised form. In addition, professional guidance includes case studies illustrating how ethical issues can be addressed, including when researching online forums (British Sociological Association, no date).
Watch the videos below and consider what insights the postgraduate researcher and supervisor provide regarding issues such as being an ‘insider researcher’, power relations, avoiding intrusion, maintaining participant anonymity and complying with research ethics and professional standards. How might their experiences inform the design and conduct of your own study?
Postgraduate researcher and supervisor talk about ethical considerations
Your thoughtful consideration of the ethical issues that might arise and how you would address these should enable you to propose an ethically informed study and conduct it in a responsible, fair and sensitive manner.
British Educational Research Association (2018) Ethical Guidelines for Educational Research. Available at: https://www.bera.ac.uk/publication/ethical-guidelines-for-educational-research-2018 (Accessed: 9 June 2023).
British Psychological Society (2021) Code of Human Research Ethics . Available at: https://cms.bps.org.uk/sites/default/files/2022-06/BPS%20Code%20of%20Human%20Research%20Ethics%20%281%29.pdf (Accessed: 9 June 2023).
British Sociological Association (2016) Researching online forums . Available at: https://www.britsoc.co.uk/media/24834/j000208_researching_online_forums_-cs1-_v3.pdf (Accessed: 9 June 2023).
Health Research Authority (2022) UK Policy Framework for Health and Social Care Research . Available at: https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/uk-policy-framework-health-and-social-care-research/#chiefinvestigators (Accessed: 9 June 2023).
Heslop, C., Burns, S., Lobo, R. (2018) ‘Managing qualitative research as insider-research in small rural communities’, Rural and Remote Health , 18: pp. 4576.
Equality Act 2010, c. 15. Available at: https://www.legislation.gov.uk/ukpga/2010/15/introduction (Accessed: 9 June 2023).
National Institute for Health and Care Research (no date) Equality, Diversity and Inclusion (EDI) . Available at: https://arc-kss.nihr.ac.uk/public-and-community-involvement/pcie-guide/how-to-do-pcie/equality-diversity-and-inclusion-edi (Accessed: 9 June 2023).
National Institute for Health and Care Research (2020) Improving inclusion of under-served groups in clinical research: Guidance from INCLUDE project. Available at: https://www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 (Accessed: 9 June 2023).
Sapiro, B. and Matthews, E. (2020) ‘Both Insider and Outsider. On Conducting Social Work Research in Mental Health Settings’, Advances in Social Work , 20(3). Available at: https://doi.org/10.18060/23926
Turcotte-Tremblay, A. and McSween-Cadieux, E. (2018) ‘A reflection on the challenge of protecting confidentiality of participants when disseminating research results locally’, BMC Medical Ethics, 19(supplement 1), no. 45. Available at: https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-018-0279-0
United Nations General Assembly (1948) The Universal Declaration of Human Rights . Resolution A/RES/217/A. Available at: https://www.un.org/en/about-us/universal-declaration-of-human-rights#:~:text=Drafted%20by%20representatives%20with%20different,all%20peoples%20and%20all%20nations . (Accessed: 9 June 2023).
Wellcome Trust (2014) Ensuring your research is ethical: A guide for Extended Project Qualification students . Available at: https://wellcome.org/sites/default/files/wtp057673_0.pdf (Accessed: 9 June 2023).
More articles from the research proposal collection
Writing your research proposal
A doctoral research degree is the highest academic qualification that a student can achieve. The guidance provided in these articles will help you apply for one of the two main types of research degree offered by The Open University.
Level: 1 Introductory

Defining your research methodology
Your research methodology is the approach you will take to guide your research process and explain why you use particular methods. This article explains more.

Writing your proposal and preparing for your interview
The final article looks at writing your research proposal - from the introduction through to citations and referencing - as well as preparing for your interview.
Free courses on postgraduate study

Are you ready for postgraduate study?
This free course, Are you ready for postgraduate study, will help you to become familiar with the requirements and demands of postgraduate study and ensure you are ready to develop the skills and confidence to pursue your learning further.

Succeeding in postgraduate study
This free course, Succeeding in postgraduate study, will help you to become familiar with the requirements and demands of postgraduate study and to develop the skills and confidence to pursue your learning further.

Applying to study for a PhD in psychology
This free OpenLearn course is for psychology students and graduates who are interested in PhD study at some future point. Even if you have met PhD students and heard about their projects, it is likely that you have only a vague idea of what PhD study entails. This course is intended to give you more information.
Become an OU student
Ratings & comments, share this free course, copyright information, publication details.
- Originally published: Tuesday, 27 June 2023
- Body text - Creative Commons BY-NC-SA 4.0 : The Open University
- Image 'Pebbles balance on a stone see-saw' - Copyright: Photo 51106733 / Balance © Anatoli Styf | Dreamstime.com
- Image 'Camera equipment set up filming a man talking' - Copyright: Photo 42631221 © Gabriel Robledo | Dreamstime.com
- Image 'Applying to study for a PhD in psychology' - Copyright free
- Image 'Succeeding in postgraduate study' - Copyright: © Everste/Getty Images
- Image 'Addressing ethical issues in your research proposal' - Copyright: Photo 50384175 / Children Playing © Lenutaidi | Dreamstime.com
- Image 'Writing your proposal and preparing for your interview' - Copyright: Photo 133038259 / Black Student © Fizkes | Dreamstime.com
- Image 'Defining your research methodology' - Copyright free
- Image 'Writing your research proposal' - Copyright free
- Image 'Are you ready for postgraduate study?' - Copyright free
Rate and Review
Rate this article, review this article.
Log into OpenLearn to leave reviews and join in the conversation.
Article reviews
For further information, take a look at our frequently asked questions which may give you the support you need.
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Activities /
Ensuring ethical standards and procedures for research with human beings
Research ethics govern the standards of conduct for scientific researchers. It is important to adhere to ethical principles in order to protect the dignity, rights and welfare of research participants. As such, all research involving human beings should be reviewed by an ethics committee to ensure that the appropriate ethical standards are being upheld. Discussion of the ethical principles of beneficence, justice and autonomy are central to ethical review.
WHO works with Member States and partners to promote ethical standards and appropriate systems of review for any course of research involving human subjects. Within WHO, the Research Ethics Review Committee (ERC) ensures that WHO only supports research of the highest ethical standards. The ERC reviews all research projects involving human participants supported either financially or technically by WHO. The ERC is guided in its work by the World Medical Association Declaration of Helsinki (1964), last updated in 2013, as well as the International Ethical Guidelines for Biomedical Research Involving Human Subjects (CIOMS 2016).
WHO releases AI ethics and governance guidance for large multi-modal models
Call for proposals: WHO project on ethical climate and health research
Call for applications: Ethical issues arising in research into health and climate change
Research Ethics Review Committee

Standards and operational guidance for ethics review of health-related research with...

WHO tool for benchmarking ethics oversight of health-related research involving human...
Related activities
Developing normative guidance to address ethical challenges in global health
Supporting countries to manage ethical issues during outbreaks and emergencies
Engaging the global community in health ethics
Building ethics capacity
Framing the ethics of public health surveillance
Related health topics
Global health ethics
Human genome editing
Related teams
Related links
- International ethical guidelines for biomedical research involving human subjects Council for International Organizations of Medical Sciences. pdf, 1.55Mb
- International ethical guidelines for epidemiological studies Council for International Organizations of Medical Sciences. pdf, 634Kb
- World Medical Association: Declaration of Helsinki
- European Group on Ethics
- Directive 2001/20/ec of the European Parliament and of the Council pdf, 152Kb
- Council of Europe (Oviedo Convention - Protocol on biomedical research)
- Nuffield Council: The ethics of research related to healthcare in developing countries
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Methodology
- Ethical Considerations in Research | Types & Examples
Ethical Considerations in Research | Types & Examples
Published on 7 May 2022 by Pritha Bhandari . Revised on 6 July 2024.
Ethical considerations in research are a set of principles that guide your research designs and practices. Scientists and researchers must always adhere to a certain code of conduct when collecting data from people.
The goals of human research often include understanding real-life phenomena, studying effective treatments, investigating behaviours, and improving lives in other ways. What you decide to research and how you conduct that research involve key ethical considerations.
These considerations work to:
- Protect the rights of research participants
- Enhance research validity
- Maintain scientific integrity
Table of contents
Why do research ethics matter, getting ethical approval for your study, types of ethical issues, voluntary participation, informed consent, confidentiality, potential for harm, results communication, examples of ethical failures, frequently asked questions about research ethics.
Research ethics matter for scientific integrity, human rights and dignity, and collaboration between science and society. These principles make sure that participation in studies is voluntary, informed, and safe for research subjects.
You’ll balance pursuing important research aims with using ethical research methods and procedures. It’s always necessary to prevent permanent or excessive harm to participants, whether inadvertent or not.
Defying research ethics will also lower the credibility of your research because it’s hard for others to trust your data if your methods are morally questionable.
Even if a research idea is valuable to society, it doesn’t justify violating the human rights or dignity of your study participants.
Prevent plagiarism, run a free check.
Before you start any study involving data collection with people, you’ll submit your research proposal to an institutional review board (IRB) .
An IRB is a committee that checks whether your research aims and research design are ethically acceptable and follow your institution’s code of conduct. They check that your research materials and procedures are up to code.
If successful, you’ll receive IRB approval, and you can begin collecting data according to the approved procedures. If you want to make any changes to your procedures or materials, you’ll need to submit a modification application to the IRB for approval.
If unsuccessful, you may be asked to re-submit with modifications or your research proposal may receive a rejection. To get IRB approval, it’s important to explicitly note how you’ll tackle each of the ethical issues that may arise in your study.
There are several ethical issues you should always pay attention to in your research design, and these issues can overlap with each other.
You’ll usually outline ways you’ll deal with each issue in your research proposal if you plan to collect data from participants.
| Voluntary participation | Your participants are free to opt in or out of the study at any point in time. |
|---|---|
| Informed consent | Participants know the purpose, benefits, risks, and funding behind the study before they agree or decline to join. |
| Anonymity | You don’t know the identities of the participants. Personally identifiable data is not collected. |
| Confidentiality | You know who the participants are but keep that information hidden from everyone else. You anonymise personally identifiable data so that it can’t be linked to other data by anyone else. |
| Potential for harm | Physical, social, psychological, and all other types of harm are kept to an absolute minimum. |
| Results communication | You ensure your work is free of plagiarism or research misconduct, and you accurately represent your results. |
Voluntary participation means that all research subjects are free to choose to participate without any pressure or coercion.
All participants are able to withdraw from, or leave, the study at any point without feeling an obligation to continue. Your participants don’t need to provide a reason for leaving the study.
It’s important to make it clear to participants that there are no negative consequences or repercussions to their refusal to participate. After all, they’re taking the time to help you in the research process, so you should respect their decisions without trying to change their minds.
Voluntary participation is an ethical principle protected by international law and many scientific codes of conduct.
Take special care to ensure there’s no pressure on participants when you’re working with vulnerable groups of people who may find it hard to stop the study even when they want to.
Informed consent refers to a situation in which all potential participants receive and understand all the information they need to decide whether they want to participate. This includes information about the study’s benefits, risks, funding, and institutional approval.
- What the study is about
- The risks and benefits of taking part
- How long the study will take
- Your supervisor’s contact information and the institution’s approval number
Usually, you’ll provide participants with a text for them to read and ask them if they have any questions. If they agree to participate, they can sign or initial the consent form. Note that this may not be sufficient for informed consent when you work with particularly vulnerable groups of people.
If you’re collecting data from people with low literacy, make sure to verbally explain the consent form to them before they agree to participate.
For participants with very limited English proficiency, you should always translate the study materials or work with an interpreter so they have all the information in their first language.
In research with children, you’ll often need informed permission for their participation from their parents or guardians. Although children cannot give informed consent, it’s best to also ask for their assent (agreement) to participate, depending on their age and maturity level.
Anonymity means that you don’t know who the participants are and you can’t link any individual participant to their data.
You can only guarantee anonymity by not collecting any personally identifying information – for example, names, phone numbers, email addresses, IP addresses, physical characteristics, photos, and videos.
In many cases, it may be impossible to truly anonymise data collection. For example, data collected in person or by phone cannot be considered fully anonymous because some personal identifiers (demographic information or phone numbers) are impossible to hide.
You’ll also need to collect some identifying information if you give your participants the option to withdraw their data at a later stage.
Data pseudonymisation is an alternative method where you replace identifying information about participants with pseudonymous, or fake, identifiers. The data can still be linked to participants, but it’s harder to do so because you separate personal information from the study data.
Confidentiality means that you know who the participants are, but you remove all identifying information from your report.
All participants have a right to privacy, so you should protect their personal data for as long as you store or use it. Even when you can’t collect data anonymously, you should secure confidentiality whenever you can.
Some research designs aren’t conducive to confidentiality, but it’s important to make all attempts and inform participants of the risks involved.
As a researcher, you have to consider all possible sources of harm to participants. Harm can come in many different forms.
- Psychological harm: Sensitive questions or tasks may trigger negative emotions such as shame or anxiety.
- Social harm: Participation can involve social risks, public embarrassment, or stigma.
- Physical harm: Pain or injury can result from the study procedures.
- Legal harm: Reporting sensitive data could lead to legal risks or a breach of privacy.
It’s best to consider every possible source of harm in your study, as well as concrete ways to mitigate them. Involve your supervisor to discuss steps for harm reduction.
Make sure to disclose all possible risks of harm to participants before the study to get informed consent. If there is a risk of harm, prepare to provide participants with resources, counselling, or medical services if needed.
Some of these questions may bring up negative emotions, so you inform participants about the sensitive nature of the survey and assure them that their responses will be confidential.
The way you communicate your research results can sometimes involve ethical issues. Good science communication is honest, reliable, and credible. It’s best to make your results as transparent as possible.
Take steps to actively avoid plagiarism and research misconduct wherever possible.
Plagiarism means submitting others’ works as your own. Although it can be unintentional, copying someone else’s work without proper credit amounts to stealing. It’s an ethical problem in research communication because you may benefit by harming other researchers.
Self-plagiarism is when you republish or re-submit parts of your own papers or reports without properly citing your original work.
This is problematic because you may benefit from presenting your ideas as new and original even though they’ve already been published elsewhere in the past. You may also be infringing on your previous publisher’s copyright, violating an ethical code, or wasting time and resources by doing so.
In extreme cases of self-plagiarism, entire datasets or papers are sometimes duplicated. These are major ethical violations because they can skew research findings if taken as original data.
You notice that two published studies have similar characteristics even though they are from different years. Their sample sizes, locations, treatments, and results are highly similar, and the studies share one author in common.
Research misconduct
Research misconduct means making up or falsifying data, manipulating data analyses, or misrepresenting results in research reports. It’s a form of academic fraud.
These actions are committed intentionally and can have serious consequences; research misconduct is not a simple mistake or a point of disagreement about data analyses.
Research misconduct is a serious ethical issue because it can undermine scientific integrity and institutional credibility. It leads to a waste of funding and resources that could have been used for alternative research.
Later investigations revealed that they fabricated and manipulated their data to show a nonexistent link between vaccines and autism. Wakefield also neglected to disclose important conflicts of interest, and his medical license was taken away.
This fraudulent work sparked vaccine hesitancy among parents and caregivers. The rate of MMR vaccinations in children fell sharply, and measles outbreaks became more common due to a lack of herd immunity.
Research scandals with ethical failures are littered throughout history, but some took place not that long ago.
Some scientists in positions of power have historically mistreated or even abused research participants to investigate research problems at any cost. These participants were prisoners, under their care, or otherwise trusted them to treat them with dignity.
To demonstrate the importance of research ethics, we’ll briefly review two research studies that violated human rights in modern history.
These experiments were inhumane and resulted in trauma, permanent disabilities, or death in many cases.
After some Nazi doctors were put on trial for their crimes, the Nuremberg Code of research ethics for human experimentation was developed in 1947 to establish a new standard for human experimentation in medical research.
In reality, the actual goal was to study the effects of the disease when left untreated, and the researchers never informed participants about their diagnoses or the research aims.
Although participants experienced severe health problems, including blindness and other complications, the researchers only pretended to provide medical care.
When treatment became possible in 1943, 11 years after the study began, none of the participants were offered it, despite their health conditions and high risk of death.
Ethical failures like these resulted in severe harm to participants, wasted resources, and lower trust in science and scientists. This is why all research institutions have strict ethical guidelines for performing research.
Ethical considerations in research are a set of principles that guide your research designs and practices. These principles include voluntary participation, informed consent, anonymity, confidentiality, potential for harm, and results communication.
Scientists and researchers must always adhere to a certain code of conduct when collecting data from others .
These considerations protect the rights of research participants, enhance research validity , and maintain scientific integrity.
Research ethics matter for scientific integrity, human rights and dignity, and collaboration between science and society. These principles make sure that participation in studies is voluntary, informed, and safe.
Anonymity means you don’t know who the participants are, while confidentiality means you know who they are but remove identifying information from your research report. Both are important ethical considerations .
You can only guarantee anonymity by not collecting any personally identifying information – for example, names, phone numbers, email addresses, IP addresses, physical characteristics, photos, or videos.
You can keep data confidential by using aggregate information in your research report, so that you only refer to groups of participants rather than individuals.
These actions are committed intentionally and can have serious consequences; research misconduct is not a simple mistake or a point of disagreement but a serious ethical failure.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
Bhandari, P. (2024, July 05). Ethical Considerations in Research | Types & Examples. Scribbr. Retrieved 21 August 2024, from https://www.scribbr.co.uk/research-methods/ethical-considerations/
Is this article helpful?

Pritha Bhandari
Other students also liked, a quick guide to experimental design | 5 steps & examples, data collection methods | step-by-step guide & examples, how to avoid plagiarism | tips on citing sources.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
National Institute of Environmental Health Sciences
Your environment. your health., what is ethics in research & why is it important, by david b. resnik, j.d., ph.d..
December 23, 2020
The ideas and opinions expressed in this essay are the author’s own and do not necessarily represent those of the NIH, NIEHS, or US government.

When most people think of ethics (or morals), they think of rules for distinguishing between right and wrong, such as the Golden Rule ("Do unto others as you would have them do unto you"), a code of professional conduct like the Hippocratic Oath ("First of all, do no harm"), a religious creed like the Ten Commandments ("Thou Shalt not kill..."), or a wise aphorisms like the sayings of Confucius. This is the most common way of defining "ethics": norms for conduct that distinguish between acceptable and unacceptable behavior.
Most people learn ethical norms at home, at school, in church, or in other social settings. Although most people acquire their sense of right and wrong during childhood, moral development occurs throughout life and human beings pass through different stages of growth as they mature. Ethical norms are so ubiquitous that one might be tempted to regard them as simple commonsense. On the other hand, if morality were nothing more than commonsense, then why are there so many ethical disputes and issues in our society?
Alternatives to Animal Testing

Alternative test methods are methods that replace, reduce, or refine animal use in research and testing
Learn more about Environmental science Basics
One plausible explanation of these disagreements is that all people recognize some common ethical norms but interpret, apply, and balance them in different ways in light of their own values and life experiences. For example, two people could agree that murder is wrong but disagree about the morality of abortion because they have different understandings of what it means to be a human being.
Most societies also have legal rules that govern behavior, but ethical norms tend to be broader and more informal than laws. Although most societies use laws to enforce widely accepted moral standards and ethical and legal rules use similar concepts, ethics and law are not the same. An action may be legal but unethical or illegal but ethical. We can also use ethical concepts and principles to criticize, evaluate, propose, or interpret laws. Indeed, in the last century, many social reformers have urged citizens to disobey laws they regarded as immoral or unjust laws. Peaceful civil disobedience is an ethical way of protesting laws or expressing political viewpoints.
Another way of defining 'ethics' focuses on the disciplines that study standards of conduct, such as philosophy, theology, law, psychology, or sociology. For example, a "medical ethicist" is someone who studies ethical standards in medicine. One may also define ethics as a method, procedure, or perspective for deciding how to act and for analyzing complex problems and issues. For instance, in considering a complex issue like global warming , one may take an economic, ecological, political, or ethical perspective on the problem. While an economist might examine the cost and benefits of various policies related to global warming, an environmental ethicist could examine the ethical values and principles at stake.
See ethics in practice at NIEHS
Read latest updates in our monthly Global Environmental Health Newsletter

Many different disciplines, institutions , and professions have standards for behavior that suit their particular aims and goals. These standards also help members of the discipline to coordinate their actions or activities and to establish the public's trust of the discipline. For instance, ethical standards govern conduct in medicine, law, engineering, and business. Ethical norms also serve the aims or goals of research and apply to people who conduct scientific research or other scholarly or creative activities. There is even a specialized discipline, research ethics, which studies these norms. See Glossary of Commonly Used Terms in Research Ethics and Research Ethics Timeline .
There are several reasons why it is important to adhere to ethical norms in research. First, norms promote the aims of research , such as knowledge, truth, and avoidance of error. For example, prohibitions against fabricating , falsifying, or misrepresenting research data promote the truth and minimize error.
Join an NIEHS Study
See how we put research Ethics to practice.
Visit Joinastudy.niehs.nih.gov to see the various studies NIEHS perform.

Second, since research often involves a great deal of cooperation and coordination among many different people in different disciplines and institutions, ethical standards promote the values that are essential to collaborative work , such as trust, accountability, mutual respect, and fairness. For example, many ethical norms in research, such as guidelines for authorship , copyright and patenting policies , data sharing policies, and confidentiality rules in peer review, are designed to protect intellectual property interests while encouraging collaboration. Most researchers want to receive credit for their contributions and do not want to have their ideas stolen or disclosed prematurely.
Third, many of the ethical norms help to ensure that researchers can be held accountable to the public . For instance, federal policies on research misconduct, conflicts of interest, the human subjects protections, and animal care and use are necessary in order to make sure that researchers who are funded by public money can be held accountable to the public.
Fourth, ethical norms in research also help to build public support for research. People are more likely to fund a research project if they can trust the quality and integrity of research.
Finally, many of the norms of research promote a variety of other important moral and social values , such as social responsibility, human rights, animal welfare, compliance with the law, and public health and safety. Ethical lapses in research can significantly harm human and animal subjects, students, and the public. For example, a researcher who fabricates data in a clinical trial may harm or even kill patients, and a researcher who fails to abide by regulations and guidelines relating to radiation or biological safety may jeopardize his health and safety or the health and safety of staff and students.
Codes and Policies for Research Ethics
Given the importance of ethics for the conduct of research, it should come as no surprise that many different professional associations, government agencies, and universities have adopted specific codes, rules, and policies relating to research ethics. Many government agencies have ethics rules for funded researchers.
- National Institutes of Health (NIH)
- National Science Foundation (NSF)
- Food and Drug Administration (FDA)
- Environmental Protection Agency (EPA)
- US Department of Agriculture (USDA)
- Singapore Statement on Research Integrity
- American Chemical Society, The Chemist Professional’s Code of Conduct
- Code of Ethics (American Society for Clinical Laboratory Science)
- American Psychological Association, Ethical Principles of Psychologists and Code of Conduct
- Statement on Professional Ethics (American Association of University Professors)
- Nuremberg Code
- World Medical Association's Declaration of Helsinki
Ethical Principles
The following is a rough and general summary of some ethical principles that various codes address*:

Strive for honesty in all scientific communications. Honestly report data, results, methods and procedures, and publication status. Do not fabricate, falsify, or misrepresent data. Do not deceive colleagues, research sponsors, or the public.

Objectivity
Strive to avoid bias in experimental design, data analysis, data interpretation, peer review, personnel decisions, grant writing, expert testimony, and other aspects of research where objectivity is expected or required. Avoid or minimize bias or self-deception. Disclose personal or financial interests that may affect research.

Keep your promises and agreements; act with sincerity; strive for consistency of thought and action.

Carefulness
Avoid careless errors and negligence; carefully and critically examine your own work and the work of your peers. Keep good records of research activities, such as data collection, research design, and correspondence with agencies or journals.

Share data, results, ideas, tools, resources. Be open to criticism and new ideas.
Transparency
Disclose methods, materials, assumptions, analyses, and other information needed to evaluate your research.

Accountability
Take responsibility for your part in research and be prepared to give an account (i.e. an explanation or justification) of what you did on a research project and why.

Intellectual Property
Honor patents, copyrights, and other forms of intellectual property. Do not use unpublished data, methods, or results without permission. Give proper acknowledgement or credit for all contributions to research. Never plagiarize.

Confidentiality
Protect confidential communications, such as papers or grants submitted for publication, personnel records, trade or military secrets, and patient records.

Responsible Publication
Publish in order to advance research and scholarship, not to advance just your own career. Avoid wasteful and duplicative publication.

Responsible Mentoring
Help to educate, mentor, and advise students. Promote their welfare and allow them to make their own decisions.

Respect for Colleagues
Respect your colleagues and treat them fairly.

Social Responsibility
Strive to promote social good and prevent or mitigate social harms through research, public education, and advocacy.

Non-Discrimination
Avoid discrimination against colleagues or students on the basis of sex, race, ethnicity, or other factors not related to scientific competence and integrity.
Maintain and improve your own professional competence and expertise through lifelong education and learning; take steps to promote competence in science as a whole.

Know and obey relevant laws and institutional and governmental policies.

Animal Care
Show proper respect and care for animals when using them in research. Do not conduct unnecessary or poorly designed animal experiments.

Human Subjects protection
When conducting research on human subjects, minimize harms and risks and maximize benefits; respect human dignity, privacy, and autonomy; take special precautions with vulnerable populations; and strive to distribute the benefits and burdens of research fairly.
* Adapted from Shamoo A and Resnik D. 2015. Responsible Conduct of Research, 3rd ed. (New York: Oxford University Press).
Ethical Decision Making in Research
Although codes, policies, and principles are very important and useful, like any set of rules, they do not cover every situation, they often conflict, and they require interpretation. It is therefore important for researchers to learn how to interpret, assess, and apply various research rules and how to make decisions and act ethically in various situations. The vast majority of decisions involve the straightforward application of ethical rules. For example, consider the following case:
The research protocol for a study of a drug on hypertension requires the administration of the drug at different doses to 50 laboratory mice, with chemical and behavioral tests to determine toxic effects. Tom has almost finished the experiment for Dr. Q. He has only 5 mice left to test. However, he really wants to finish his work in time to go to Florida on spring break with his friends, who are leaving tonight. He has injected the drug in all 50 mice but has not completed all of the tests. He therefore decides to extrapolate from the 45 completed results to produce the 5 additional results.
Many different research ethics policies would hold that Tom has acted unethically by fabricating data. If this study were sponsored by a federal agency, such as the NIH, his actions would constitute a form of research misconduct , which the government defines as "fabrication, falsification, or plagiarism" (or FFP). Actions that nearly all researchers classify as unethical are viewed as misconduct. It is important to remember, however, that misconduct occurs only when researchers intend to deceive : honest errors related to sloppiness, poor record keeping, miscalculations, bias, self-deception, and even negligence do not constitute misconduct. Also, reasonable disagreements about research methods, procedures, and interpretations do not constitute research misconduct. Consider the following case:
Dr. T has just discovered a mathematical error in his paper that has been accepted for publication in a journal. The error does not affect the overall results of his research, but it is potentially misleading. The journal has just gone to press, so it is too late to catch the error before it appears in print. In order to avoid embarrassment, Dr. T decides to ignore the error.
Dr. T's error is not misconduct nor is his decision to take no action to correct the error. Most researchers, as well as many different policies and codes would say that Dr. T should tell the journal (and any coauthors) about the error and consider publishing a correction or errata. Failing to publish a correction would be unethical because it would violate norms relating to honesty and objectivity in research.
There are many other activities that the government does not define as "misconduct" but which are still regarded by most researchers as unethical. These are sometimes referred to as " other deviations " from acceptable research practices and include:
- Publishing the same paper in two different journals without telling the editors
- Submitting the same paper to different journals without telling the editors
- Not informing a collaborator of your intent to file a patent in order to make sure that you are the sole inventor
- Including a colleague as an author on a paper in return for a favor even though the colleague did not make a serious contribution to the paper
- Discussing with your colleagues confidential data from a paper that you are reviewing for a journal
- Using data, ideas, or methods you learn about while reviewing a grant or a papers without permission
- Trimming outliers from a data set without discussing your reasons in paper
- Using an inappropriate statistical technique in order to enhance the significance of your research
- Bypassing the peer review process and announcing your results through a press conference without giving peers adequate information to review your work
- Conducting a review of the literature that fails to acknowledge the contributions of other people in the field or relevant prior work
- Stretching the truth on a grant application in order to convince reviewers that your project will make a significant contribution to the field
- Stretching the truth on a job application or curriculum vita
- Giving the same research project to two graduate students in order to see who can do it the fastest
- Overworking, neglecting, or exploiting graduate or post-doctoral students
- Failing to keep good research records
- Failing to maintain research data for a reasonable period of time
- Making derogatory comments and personal attacks in your review of author's submission
- Promising a student a better grade for sexual favors
- Using a racist epithet in the laboratory
- Making significant deviations from the research protocol approved by your institution's Animal Care and Use Committee or Institutional Review Board for Human Subjects Research without telling the committee or the board
- Not reporting an adverse event in a human research experiment
- Wasting animals in research
- Exposing students and staff to biological risks in violation of your institution's biosafety rules
- Sabotaging someone's work
- Stealing supplies, books, or data
- Rigging an experiment so you know how it will turn out
- Making unauthorized copies of data, papers, or computer programs
- Owning over $10,000 in stock in a company that sponsors your research and not disclosing this financial interest
- Deliberately overestimating the clinical significance of a new drug in order to obtain economic benefits
These actions would be regarded as unethical by most scientists and some might even be illegal in some cases. Most of these would also violate different professional ethics codes or institutional policies. However, they do not fall into the narrow category of actions that the government classifies as research misconduct. Indeed, there has been considerable debate about the definition of "research misconduct" and many researchers and policy makers are not satisfied with the government's narrow definition that focuses on FFP. However, given the huge list of potential offenses that might fall into the category "other serious deviations," and the practical problems with defining and policing these other deviations, it is understandable why government officials have chosen to limit their focus.
Finally, situations frequently arise in research in which different people disagree about the proper course of action and there is no broad consensus about what should be done. In these situations, there may be good arguments on both sides of the issue and different ethical principles may conflict. These situations create difficult decisions for research known as ethical or moral dilemmas . Consider the following case:
Dr. Wexford is the principal investigator of a large, epidemiological study on the health of 10,000 agricultural workers. She has an impressive dataset that includes information on demographics, environmental exposures, diet, genetics, and various disease outcomes such as cancer, Parkinson’s disease (PD), and ALS. She has just published a paper on the relationship between pesticide exposure and PD in a prestigious journal. She is planning to publish many other papers from her dataset. She receives a request from another research team that wants access to her complete dataset. They are interested in examining the relationship between pesticide exposures and skin cancer. Dr. Wexford was planning to conduct a study on this topic.
Dr. Wexford faces a difficult choice. On the one hand, the ethical norm of openness obliges her to share data with the other research team. Her funding agency may also have rules that obligate her to share data. On the other hand, if she shares data with the other team, they may publish results that she was planning to publish, thus depriving her (and her team) of recognition and priority. It seems that there are good arguments on both sides of this issue and Dr. Wexford needs to take some time to think about what she should do. One possible option is to share data, provided that the investigators sign a data use agreement. The agreement could define allowable uses of the data, publication plans, authorship, etc. Another option would be to offer to collaborate with the researchers.
The following are some step that researchers, such as Dr. Wexford, can take to deal with ethical dilemmas in research:
What is the problem or issue?
It is always important to get a clear statement of the problem. In this case, the issue is whether to share information with the other research team.
What is the relevant information?
Many bad decisions are made as a result of poor information. To know what to do, Dr. Wexford needs to have more information concerning such matters as university or funding agency or journal policies that may apply to this situation, the team's intellectual property interests, the possibility of negotiating some kind of agreement with the other team, whether the other team also has some information it is willing to share, the impact of the potential publications, etc.
What are the different options?
People may fail to see different options due to a limited imagination, bias, ignorance, or fear. In this case, there may be other choices besides 'share' or 'don't share,' such as 'negotiate an agreement' or 'offer to collaborate with the researchers.'
How do ethical codes or policies as well as legal rules apply to these different options?
The university or funding agency may have policies on data management that apply to this case. Broader ethical rules, such as openness and respect for credit and intellectual property, may also apply to this case. Laws relating to intellectual property may be relevant.
Are there any people who can offer ethical advice?
It may be useful to seek advice from a colleague, a senior researcher, your department chair, an ethics or compliance officer, or anyone else you can trust. In the case, Dr. Wexford might want to talk to her supervisor and research team before making a decision.
After considering these questions, a person facing an ethical dilemma may decide to ask more questions, gather more information, explore different options, or consider other ethical rules. However, at some point he or she will have to make a decision and then take action. Ideally, a person who makes a decision in an ethical dilemma should be able to justify his or her decision to himself or herself, as well as colleagues, administrators, and other people who might be affected by the decision. He or she should be able to articulate reasons for his or her conduct and should consider the following questions in order to explain how he or she arrived at his or her decision:
- Which choice will probably have the best overall consequences for science and society?
- Which choice could stand up to further publicity and scrutiny?
- Which choice could you not live with?
- Think of the wisest person you know. What would he or she do in this situation?
- Which choice would be the most just, fair, or responsible?
After considering all of these questions, one still might find it difficult to decide what to do. If this is the case, then it may be appropriate to consider others ways of making the decision, such as going with a gut feeling or intuition, seeking guidance through prayer or meditation, or even flipping a coin. Endorsing these methods in this context need not imply that ethical decisions are irrational, however. The main point is that human reasoning plays a pivotal role in ethical decision-making but there are limits to its ability to solve all ethical dilemmas in a finite amount of time.
Promoting Ethical Conduct in Science
Do U.S. research institutions meet or exceed federal mandates for instruction in responsible conduct of research? A national survey
Read about U.S. research instutuins follow federal manadates for ethics in research
Learn more about NIEHS Research
Most academic institutions in the US require undergraduate, graduate, or postgraduate students to have some education in the responsible conduct of research (RCR) . The NIH and NSF have both mandated training in research ethics for students and trainees. Many academic institutions outside of the US have also developed educational curricula in research ethics
Those of you who are taking or have taken courses in research ethics may be wondering why you are required to have education in research ethics. You may believe that you are highly ethical and know the difference between right and wrong. You would never fabricate or falsify data or plagiarize. Indeed, you also may believe that most of your colleagues are highly ethical and that there is no ethics problem in research..
If you feel this way, relax. No one is accusing you of acting unethically. Indeed, the evidence produced so far shows that misconduct is a very rare occurrence in research, although there is considerable variation among various estimates. The rate of misconduct has been estimated to be as low as 0.01% of researchers per year (based on confirmed cases of misconduct in federally funded research) to as high as 1% of researchers per year (based on self-reports of misconduct on anonymous surveys). See Shamoo and Resnik (2015), cited above.
Clearly, it would be useful to have more data on this topic, but so far there is no evidence that science has become ethically corrupt, despite some highly publicized scandals. Even if misconduct is only a rare occurrence, it can still have a tremendous impact on science and society because it can compromise the integrity of research, erode the public’s trust in science, and waste time and resources. Will education in research ethics help reduce the rate of misconduct in science? It is too early to tell. The answer to this question depends, in part, on how one understands the causes of misconduct. There are two main theories about why researchers commit misconduct. According to the "bad apple" theory, most scientists are highly ethical. Only researchers who are morally corrupt, economically desperate, or psychologically disturbed commit misconduct. Moreover, only a fool would commit misconduct because science's peer review system and self-correcting mechanisms will eventually catch those who try to cheat the system. In any case, a course in research ethics will have little impact on "bad apples," one might argue.
According to the "stressful" or "imperfect" environment theory, misconduct occurs because various institutional pressures, incentives, and constraints encourage people to commit misconduct, such as pressures to publish or obtain grants or contracts, career ambitions, the pursuit of profit or fame, poor supervision of students and trainees, and poor oversight of researchers (see Shamoo and Resnik 2015). Moreover, defenders of the stressful environment theory point out that science's peer review system is far from perfect and that it is relatively easy to cheat the system. Erroneous or fraudulent research often enters the public record without being detected for years. Misconduct probably results from environmental and individual causes, i.e. when people who are morally weak, ignorant, or insensitive are placed in stressful or imperfect environments. In any case, a course in research ethics can be useful in helping to prevent deviations from norms even if it does not prevent misconduct. Education in research ethics is can help people get a better understanding of ethical standards, policies, and issues and improve ethical judgment and decision making. Many of the deviations that occur in research may occur because researchers simply do not know or have never thought seriously about some of the ethical norms of research. For example, some unethical authorship practices probably reflect traditions and practices that have not been questioned seriously until recently. If the director of a lab is named as an author on every paper that comes from his lab, even if he does not make a significant contribution, what could be wrong with that? That's just the way it's done, one might argue. Another example where there may be some ignorance or mistaken traditions is conflicts of interest in research. A researcher may think that a "normal" or "traditional" financial relationship, such as accepting stock or a consulting fee from a drug company that sponsors her research, raises no serious ethical issues. Or perhaps a university administrator sees no ethical problem in taking a large gift with strings attached from a pharmaceutical company. Maybe a physician thinks that it is perfectly appropriate to receive a $300 finder’s fee for referring patients into a clinical trial.
If "deviations" from ethical conduct occur in research as a result of ignorance or a failure to reflect critically on problematic traditions, then a course in research ethics may help reduce the rate of serious deviations by improving the researcher's understanding of ethics and by sensitizing him or her to the issues.
Finally, education in research ethics should be able to help researchers grapple with the ethical dilemmas they are likely to encounter by introducing them to important concepts, tools, principles, and methods that can be useful in resolving these dilemmas. Scientists must deal with a number of different controversial topics, such as human embryonic stem cell research, cloning, genetic engineering, and research involving animal or human subjects, which require ethical reflection and deliberation.
Ethical considerations in research: Best practices and examples

To conduct responsible research, you’ve got to think about ethics. They protect participants’ rights and their well-being - and they ensure your findings are valid and reliable. This isn’t just a box for you to tick. It’s a crucial consideration that can make all the difference to the outcome of your research.
In this article, we'll explore the meaning and importance of research ethics in today's research landscape. You'll learn best practices to conduct ethical and impactful research.
Examples of ethical considerations in research
As a researcher, you're responsible for ethical research alongside your organization. Fulfilling ethical guidelines is critical. Organizations must ensure employees follow best practices to protect participants' rights and well-being.
Keep these things in mind when it comes to ethical considerations in research:
Voluntary participation
Voluntary participation is key. Nobody should feel like they're being forced to participate or pressured into doing anything they don't want to. That means giving people a choice and the ability to opt out at any time, even if they've already agreed to take part in the study.
Informed consent
Informed consent isn't just an ethical consideration. It's a legal requirement as well. Participants must fully understand what they're agreeing to, including potential risks and benefits.
The best way to go about this is by using a consent form. Make sure you include:
- A brief description of the study and research methods.
- The potential benefits and risks of participating.
- The length of the study.
- Contact information for the researcher and/or sponsor.
- Reiteration of the participant’s right to withdraw from the research project at any time without penalty.
Anonymity means that participants aren't identifiable in any way. This includes:
- Email address
- Photographs
- Video footage
You need a way to anonymize research data so that it can't be traced back to individual participants. This may involve creating a new digital ID for participants that can’t be linked back to their original identity using numerical codes.
Confidentiality
Information gathered during a study must be kept confidential. Confidentiality helps to protect the privacy of research participants. It also ensures that their information isn't disclosed to unauthorized individuals.
Some ways to ensure confidentiality include:
- Using a secure server to store data.
- Removing identifying information from databases that contain sensitive data.
- Using a third-party company to process and manage research participant data.
- Not keeping participant records for longer than necessary.
- Avoiding discussion of research findings in public forums.
Potential for harm
The potential for harm is a crucial factor in deciding whether a research study should proceed. It can manifest in various forms, such as:
- Psychological harm
- Social harm
- Physical harm
Conduct an ethical review to identify possible harms. Be prepared to explain how you’ll minimize these harms and what support is available in case they do happen.
Fair payment
One of the most crucial aspects of setting up a research study is deciding on fair compensation for your participants. Underpayment is a common ethical issue that shouldn't be overlooked. Properly rewarding participants' time is critical for boosting engagement and obtaining high-quality data. While Prolific requires a minimum payment of £6.00 / $8.00 per hour, there are other factors you need to consider when deciding on a fair payment.
First, check your institution's reimbursement guidelines to see if they already have a minimum or maximum hourly rate. You can also use the national minimum wage as a reference point.
Next, think about the amount of work you're asking participants to do. The level of effort required for a task, such as producing a video recording versus a short survey, should correspond with the reward offered.
You also need to consider the population you're targeting. To attract research subjects with specific characteristics or high-paying jobs, you may need to offer more as an incentive.
We recommend a minimum payment of £9.00 / $12.00 per hour, but we understand that payment rates can vary depending on a range of factors. Whatever payment you choose should reflect the amount of effort participants are required to put in and be fair to everyone involved.
Ethical research made easy with Prolific
At Prolific, we believe in making ethical research easy and accessible. The findings from the Fairwork Cloudwork report speak for themselves. Prolific was given the top score out of all competitors for minimum standards of fair work.
With over 25,000 researchers in our community, we're leading the way in revolutionizing the research industry. If you're interested in learning more about how we can support your research journey, sign up to get started now.
You might also like

High-quality human data to deliver world-leading research and AIs.

Follow us on
All Rights Reserved Prolific 2024
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih clinical research trials and you, guiding principles for ethical research.
Pursuing Potential Research Participants Protections

“When people are invited to participate in research, there is a strong belief that it should be their choice based on their understanding of what the study is about, and what the risks and benefits of the study are,” said Dr. Christine Grady, chief of the NIH Clinical Center Department of Bioethics, to Clinical Center Radio in a podcast.
Clinical research advances the understanding of science and promotes human health. However, it is important to remember the individuals who volunteer to participate in research. There are precautions researchers can take – in the planning, implementation and follow-up of studies – to protect these participants in research. Ethical guidelines are established for clinical research to protect patient volunteers and to preserve the integrity of the science.
NIH Clinical Center researchers published seven main principles to guide the conduct of ethical research:
Social and clinical value
Scientific validity, fair subject selection, favorable risk-benefit ratio, independent review, informed consent.
- Respect for potential and enrolled subjects
Every research study is designed to answer a specific question. The answer should be important enough to justify asking people to accept some risk or inconvenience for others. In other words, answers to the research question should contribute to scientific understanding of health or improve our ways of preventing, treating, or caring for people with a given disease to justify exposing participants to the risk and burden of research.
A study should be designed in a way that will get an understandable answer to the important research question. This includes considering whether the question asked is answerable, whether the research methods are valid and feasible, and whether the study is designed with accepted principles, clear methods, and reliable practices. Invalid research is unethical because it is a waste of resources and exposes people to risk for no purpose
The primary basis for recruiting participants should be the scientific goals of the study — not vulnerability, privilege, or other unrelated factors. Participants who accept the risks of research should be in a position to enjoy its benefits. Specific groups of participants (for example, women or children) should not be excluded from the research opportunities without a good scientific reason or a particular susceptibility to risk.
Uncertainty about the degree of risks and benefits associated with a clinical research study is inherent. Research risks may be trivial or serious, transient or long-term. Risks can be physical, psychological, economic, or social. Everything should be done to minimize the risks and inconvenience to research participants to maximize the potential benefits, and to determine that the potential benefits are proportionate to, or outweigh, the risks.
To minimize potential conflicts of interest and make sure a study is ethically acceptable before it starts, an independent review panel should review the proposal and ask important questions, including: Are those conducting the trial sufficiently free of bias? Is the study doing all it can to protect research participants? Has the trial been ethically designed and is the risk–benefit ratio favorable? The panel also monitors a study while it is ongoing.
Potential participants should make their own decision about whether they want to participate or continue participating in research. This is done through a process of informed consent in which individuals (1) are accurately informed of the purpose, methods, risks, benefits, and alternatives to the research, (2) understand this information and how it relates to their own clinical situation or interests, and (3) make a voluntary decision about whether to participate.
Respect for potential and enrolled participants
Individuals should be treated with respect from the time they are approached for possible participation — even if they refuse enrollment in a study — throughout their participation and after their participation ends. This includes:
- respecting their privacy and keeping their private information confidential
- respecting their right to change their mind, to decide that the research does not match their interests, and to withdraw without a penalty
- informing them of new information that might emerge in the course of research, which might change their assessment of the risks and benefits of participating
- monitoring their welfare and, if they experience adverse reactions, unexpected effects, or changes in clinical status, ensuring appropriate treatment and, when necessary, removal from the study
- informing them about what was learned from the research
More information on these seven guiding principles and on bioethics in general
This page last reviewed on March 16, 2016
Connect with Us
- More Social Media from NIH
- Lehigh Home
- Research Home
Search form
- Ethical Issues in Research
You are here
Both students and faculty at Lehigh University are encouraged to become involved in the research life of the University. Departmental honors and capstone courses, as well as a number of campus fellowships and programs, offer opportunities for students to learn the skills of research and present their results. Frequently, these research projects involve interactions with and/or identifiable data about human beings as participants (or “subjects”).
Some research activities that involve people require approval by the Institutional Review Board (IRB), and others do not. The IRB is a federally mandated committee that reviews human subjects research protocols. Regardless of whether a research project is subject to IRB review, the rights and welfare of any human participants involved in the project must be protected.
The first section of this document provides guidance to students and their faculty mentors on how to incorporate human subjects protections into student research activities. This advice applies to all student research projects, including both those that are subject to IRB review and those that are not because they are chiefly learning activities. The second section of the document discusses what types of projects may be subject to review by Lehigh’s IRB.
What are key features of protecting participants in research?
Excellent human participant protection includes:
• Minimizing the risks of research to participants. • Protecting individuals who are members of a group that may be vulnerable to coercion or undue influence, as it relates to providing informed consent. • Ensuring that research subjects’ participation is informed and voluntary.
1. Minimizing the risks of research
In all aspects of the research, from recruiting subjects to collecting and storing data to reporting results, risks to research participants must be minimized.
Students are strongly encouraged to design their projects so that they are “ minimal risk ” research. As defined in the federal regulations, “minimal risk” means that participants will encounter no harms or discomforts greater than those that are a normal part of their daily lives. Faculty advisors and research program staff are asked to guide students in developing minimal risk projects. If, in the opinion of the student or faculty advisor, an intended project might be greater than minimal risk, the student or faculty advisor must seek the advice of the Research Integrity office .
What risks can arise in or result from research?
• Disclosure of identifiable sensitive information : Recording and storing individual-level identifiable information can pose risks if the data are sensitive, in the sense that disclosure could lead to harm for a research participant. Some examples of sensitive data include:
- Information about criminal behavior
- Information about work-related actions that if known could damage the individual’s employment
- Information that if widely known could engender stigma or shunning
- Information beyond the very general about the respondent’s health (which may also be subject to other privacy regulations, e.g. HIPAA)
- Information about financial or legal aspects of an individual’s life which if publicly known might enable identity theft or fraud
- Data can be sensitive in one context and not in another (e.g., certain political opinions are risky under politically repressive regimes).
These types of data only present risks if they are identifiable, that is, if linked to names, Social Security numbers, or other identifiable information, or if recorded using audio or video media (with recognizable voices or faces). To protect research participants, researchers should take steps to minimize the risk of inadvertent disclosure of identifiers and research data. It is also wise to only gather sensitive information if absolutely necessary for the research.
Good research practices include: using password protection (at a minimum) and encryption (preferred) for computer files and digitized audio or video files; using removable storage devices (thumb or flash drives) that are encrypted and password protected; locking filing cabinets where paper files are stored; and quickly transcribing unprotected, taped interviews and notes on paper so they can then be destroyed.
• Emotional or psychological trauma is a risk when respondents are asked to describe a painful event or a stigmatized identity that they do not usually discuss otherwise. Personal experiences of war, of refugee flight, of being assaulted, or of serious illness or injury are among the many potentially traumatizing topics of interview. One risk-minimizing strategy is to interview individuals who already talk publicly or frequently about a past trauma or a stigmatized identity.
Students with limited experience and training in sensitive interviewing are strongly discouraged from trying to interview research participants about painful topics. Interviewers who do conduct emotionally sensitive interviews should plan to provide subjects with a list of local counseling resources. Faculty advisors and student investigators should be aware that interviewing participants regarding emotional or psychological trauma, especially when the interviewer is inexperienced and not sufficiently trained, presents greater than minimal risk to the participants. Reminder: if an intended project might be greater than minimal risk, the student or faculty advisor must seek the advice of the Research Integrity office .
• Potential for other types of greater than minimal risks arise if individuals are asked to do anything that they would not normally do in the course of daily life which could jeopardize (i) their physical safety, (ii) their physical health, (iii) their emotional well-being, (iv) their academic standing, (v) their legal standing, (vi) their financial or employment security, or (vii) their reputation in any context. For example, asking individuals for interviews when engaging in such an interview might put them at risk of retribution for “snitching” (e.g., individuals engaged in criminal activity). Other examples include asking participants to engage in unaccustomed physical activity in which they could experience strain or injury; asking them to substantially change their diet over more than a very brief period; asking them to interact socially in unusual ways, to spy on others, or to deceive others; and so forth. Reminder: if an intended project might be greater than minimal risk, the student or faculty advisor must seek the advice of the Research Integrity office .
• Deception : Avoid deceiving research participants unless clearly necessary and no greater than minimal risk; debrief as soon as possible afterwards . Research that involves actively deceiving participants about research activities presents ethical problems. A student whose proposed project includes active deception should work with his/her faculty advisor to ensure that the overall level of risk to participants is minimal and that other IRB requirements for use of deception, e.g., an appropriate debriefing process, are included.
2. Protecting individuals who are members of a vulnerable group
“Vulnerable populations” in IRB parlance are categories of individuals whose capacity to give voluntary informed consent is likely to be impaired in some way. They may not be capable of fully assessing the risks of research participation. They may feel compelled to participate in research because of their relationship to the researcher or because their freedom is curtailed. Fully informed consent may not be possible for them because the consequences of their research participation are unpredictable.
Prisoners are vulnerable to coercion and to penalties imposed by the prison system. Medical research on pregnant women can have unknown consequences for the woman or the fetus. Accordingly, federal regulations require heightened scrutiny of research involving prisoners and pregnant women. Research to be conducted with prisoners or with pregnant women as a target group must be submitted for IRB review . Federally-mandated requirements for such scrutiny will introduce substantial delays in the review process, and could put ultimate approval in jeopardy. Research on prisoners will also require the approval of prison or jail authorities. Parolees are an intermediate category almost as vulnerable as prisoners, as they can be re-incarcerated for many activities that are not illegal for non-parolees. Students are advised to consider a research topic that does not call for interviewing (as a target population) prisoners, parolees, or pregnant women .
Children are vulnerable because their cognitive and decision-making capacities are still developing. Federal regulations require in almost all cases parental consent (permission) for children to participate in research activities. In many cases, assent from the child will also be required. Anyone planning research activities with children must be aware of regulations regarding permissible research with children, including obtaining informed parental permission as well as child assent for the research . In addition, the IRB strongly recommends that undergraduates who plan to interview or interact with children do not include activities or interview questions that could be controversial. At all times, the interaction must be conducted in a manner that protects the child .
Other vulnerable populations : Cognitively impaired individuals might not have the intellectual capacity to consent to research participation. Other groups are vulnerable because any harm that might arise from research would be particularly consequential for them. For example, undocumented residents whose status was revealed outside the research could be deported, a grave risk. Residents in homeless shelters, nursing homes and half way houses have limited autonomy with respect to housing and are vulnerable to the authority of house managers. They, as well as people who have experienced major injury, illness or disability that interferes with the quality of their lives , might be traumatized by unskillful interviewing.
The IRB strongly recommends that an undergraduate student who wishes to study a vulnerable population turn to group spokespeople, group representatives, expert informants, and professionals working with the population if they wish to learn sensitive information about the population . Members of vulnerable groups – excepting those who are identified as spokespeople – should not be asked sensitive questions, by which we mean questions that could re-traumatize them or that, if responses were revealed outside the research, could put respondents at risk.
3. Ensuring that research subjects’ participation is informed and voluntary
Even when research activities do not require IRB review, they should include an informed consent process that: (a) identifies the researcher; (b) describes what is being requested of the person (i.e., what participation in the project will require); (c) clarifies that he/she does not have to participate; (d) explains any risks or discomforts of the research; (e) explains any potential benefits to the participant, the community, and/or scientific knowledge; and (f) provides contact information for the researcher(s) and for the Lehigh IRB. (The latter contact information should be omitted if the project has not been reviewed by the IRB.) The IRB website has several examples of consent documents.
The standard process of informed consent includes a written (signed) document. However, an oral (unsigned) consent process is acceptable for a minimal-risk project not submitted for IRB review, and may be acceptable for an IRB-reviewed project as well, as long as justification for not seeking signed consent is included in the application. When oral consent is used, it is good practice for the researcher to give participants a document for their future reference stating what they were told (i.e., including all the consent elements above).
What types of research activities require IRB approval ?
Lehigh’s IRB is required to review all projects that are considered human subjects research under the federal regulatory definition of research: “a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge.” (45 CFR 46.102(d)).
A “ systematic investigation ” is a study or examination that involves a methodical procedure and plan, is theoretically grounded, specifies a focused and well-defined research problem or question, is informed by the empirical findings of others, is analytically robust, and provides a detailed and complete description of data collection methods.
“ Generalizable knowledge ” is conclusions, facts, or principles derived from particulars (e.g., individual subjects, medical records) that are applicable to or affect a whole category (members of a class, kind, or group, a field of knowledge, etc.) and enhance scientific or academic understanding. (Note that publication or other dissemination of findings does not in and of itself make the activity human subjects research.)
The experience of the IRB has been that many student-initiated or class-related research activities do not meet the federal regulatory criteria for IRB jurisdiction. However, the IRB will review any student-initiated or class-related human subjects project if the student or faculty advisor believes, and justifies briefly in the writing to the Research Integrity office, that the research falls under the regulatory jurisdiction of the IRB.
Students planning a project with human participants are encouraged to start by referring to the IRB website for information on What Types of Activities Require IRB Review , and to consult with their faculty advisor or the Research Integrity office to determine if they need IRB approval .
1. Some research activities may require IRB review, others may not. Regardless of whether or not the project requires such review, the rights and welfare of the human participants involved in the project must be protected.
2. The IRB strongly recommends that students design minimal-risk research activities. Most IRB-approved research at Lehigh is minimal risk research, and student-initiated research should, in general, be minimal risk as well. The standard of minimal risk for research is that it does not expose participants to risks greater than those they are likely to encounter in their daily lives.
3. Special attention should be paid to the potential for risks in research involving certain activities, e.g., disclosure of identifiable sensitive information, interviewing on topics of emotional or psychological trauma, and deception.
4. Students who wish to gather information about a vulnerable population should consider interviewing spokespeople and expert informants instead of members of the vulnerable group.
5. Federal law requires that research projects that involve prisoners or pregnant women must receive heightened review scrutiny. Federal regulations also require (with a few exceptions) parental consent (permission) for children to participate in research activities.
6. Research should include a process for informed consent, which can be oral (supplemented by a document) rather than signed. The process should include all the elements of informed consent.
7. Student-initiated or class-related research activities engaged in as part of an educational process usually do not require IRB review, unless the project appears to the student or faculty advisor to fit the regulatory definition of “human subjects research”: “a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge” (45 CFR 46.102(d)).
In all cases, students undertaking research activities are encouraged to first consult with their faculty advisors, using this document, along with Research Design Guidance and other resources on the IRB website , to develop meaningful and ethical research projects.
This guidance was adapted, with permission, from U.C. Berkley Human Research Protections Program’s “Ethical Issues in Undergraduate Research Activities with Human Participants” guidance .
Popular Searches
- Commencement
- Securing Our Future
- Marquette 2031
Arts & Sciences
Researching the promise, perils and ethical dimensions of technology’s relationship with mental health
From developing peer support apps to investigating social media users’ perceptions of mental health and offering ethical leadership about privacy concerns, faculty and students in the Klingler College of Arts and Sciences are finding insights at this intersection.
- By Claire Curry
- August 22, 2024
- 6 min. read

With nearly one in five U.S. adults living with mental illness, communities across the nation are struggling to meet the care and treatment needs of their residents, especially the most vulnerable. Faculty members and students in the Klingler College of Arts and Sciences are exploring the role technology may play in this area. Can it help improve diagnoses, access to care or peer support, and even flag individuals who are experiencing serious mental health crises? Could technology and social media promote openness and reduce the stigma surrounding mental health, or might they trivialize or glamorize serious conditions? Across the college, questions like these are driving vital discussions and research leadership on the ethical dimensions involved when mental health meets technology.
Peer-to-peer mental health support — in an app
One team of researchers is focusing on U.S. military veterans who are known to be at higher risk for mental health disorders. According to the National Institute of Mental Health, more than 1.7 million veterans receive treatment at VA mental health specialty programs, and organizations like Dryhootch, a nonprofit with coffeehouses and resource centers for military veterans in Milwaukee and Madison, are aiding veterans who are struggling by providing peer support.
“Veterans don’t often willingly seek out assistance from health care professionals about anything related to mental health and PTSD,” says Dr. Praveen Madiraju, professor of computer science. “They feel more at ease and open when talking to their peers. So Dryhootch started that program where veterans can go get a coffee and have that really cool, no-pressure atmosphere where they can sit and chat with other veterans.”
“Marquette was brought in to offer technological expertise — to help bridge the gap between trauma and peer mentorship.” Dr. Praveen Madiraju
Leveraging that success, Marquette faculty, working in partnership with Dryhootch, have co-created a telehealth app called BattlePeer that brings the support of peers — akin to the “battle buddies” who had their backs in wartime — directly to veterans on their mobile phones.
“Marquette was brought in to offer technological expertise — to help bridge the gap between trauma and peer mentorship,” Madiraju says. Marquette faculty, including Madiraju, and Dr. Iqbal Ahamed, Wehr Professor of Computer Science, collaborated with Dryhootch founder Bob Curry, a combat veteran, and Dr. Zeno Franco, associate professor at the Medical College of Wisconsin and psychologist at the U.S. Department of Veteran Affairs, to develop the app that matches veteran mentors with mentees, sends weekly check-ins to assess mental health and offers private and group chat features.
The team continues to refine the app and plans to expand its use to support first responders and people with cancer and other chronic diseases. “Sometimes you just need a bridge through whatever you’re going through,” Curry says. “This technology can be the bridge that gets you through to the other side.”
So far, the app has put peer support in the hands of hundreds and has the potential to reach many more, thanks to a recent licensing agreement that now makes BattlePeer available in Apple and Google app stores.
“This has been more than a decade in the making,” says Madiraju. “With the licensing, we have a massive scale advantage. Potentially, [BattlePeer] can reach hundreds of thousands of veterans across the nation.”
Online storytelling communities help new mothers
Dr. Sabirat Rubya, Northwestern Mutual Data Science Institute Assistant Professor, who contributed to developing BattlePeer, is also exploring how technology can support another at-risk population: new and expecting moms. According to Rubya, one woman in seven encounters postpartum depression, and many turn to online communities for information and advice.
“Think of it as a curated space for sharing and finding support through powerful stories.” Dr. Sabirat Rubya
Women are at times reluctant to talk about their challenges as soon-to-be and new parents, even though this type of information sharing offers valuable emotional support, says Rubya. Many women aren’t sharing their problems directly with one another because of the stigma around mental health issues related to pregnancy and new motherhood.
Rubya and graduate student Farhat Tasnim Progga analyzed three online venues — Reddit, What to Expect and BabyCenter — and concluded that online storytelling is an effective way to foster support for perinatal mental health. Their findings inspired them to develop “Mom Stories,” a web-based application where women can find stories on a range of topics of interest to new and expecting moms, from depression and baby blues to breastfeeding and newborn health. “Think of it as a curated space for sharing and finding support through powerful stories,” Rubya says about the application, which is set to launch in late 2024.
Risks and ethical questions for data use
“Is there not an ethical obligation to use every tool, every piece of data at their disposal, to attempt to save lives and help improve public health outcomes?” Dr. Michael Zimmer
While technology is making inroads in mental health research and treatment, health care professionals and scholars, including those at Marquette, are identifying ethical issues raised by these applications of technology. Collecting and accessing large data sets to advance research may compete with the goals of protecting patient privacy, for example. And deploying AI bots to provide real-time medical advice risks overlooking how biased and insufficiently trained the bots may be.
Dr. Michael Zimmer, director of the Center for Data, Ethics, and Society at Marquette and professor and vice chair of the Department of Computer Science, shared his thoughts on these ethical tensions in a June webinar hosted by the Center for Suicide Research and Prevention, joined by experts from Harvard Medical School and Northwestern University.
In his presentation, Zimmer pointed to work being done at the Smoller Laboratory at Massachusetts General Hospital, where researchers are using large data sets to help develop suicide risk prediction models. The researchers built a sound predictive model, he says, and are now exploring ways to enhance it by tapping public data sources. While the ultimate goal is to improve health outcomes and save lives, using public data for this purpose raises ethical questions.
Public data and prediction models — a step too far?
“Imagine you had access to a hundred thousand people’s health records,” says Zimmer, who served as a consultant on the project. “You knew which 10,000 had made a suicide attempt at some point and you started looking at their records to see what was unique compared to everyone else.” Such records might reveal, for example, whether an individual had an interaction with law enforcement or a bankruptcy — information that Zimmer says could lead to “unintended consequences.”
Using such data in the prediction model could lead to the presumption that those who had an interaction with law enforcement or experienced a bankruptcy are at risk of suicide — even though many would not be. And reaching out to those “at risk” individuals the model identifies based on such criteria could possibly help avert tragedies, while also potentially representing yet another breach of privacy.
“In the health setting, there’s a different kind of ethical calculus at play because these are folks who are trying to find ways to do good things with technology,” he explains. “Is there not an ethical obligation to use every tool, every piece of data at their disposal, to attempt to save lives and help improve public health outcomes?”
At the same time, it’s critical to look beyond how valuable the data is and recognize that the facts and figures represent real people and, often, vulnerable populations. “Things are moving quickly, but in the mental health space, everyone recognizes there are risks of moving too fast,” Zimmer says. “If we want to do good, we have to get this right.”
Student researchers investigate how social media users perceive mental health
In addition to faculty, Marquette students and alumni are conducting research on technology and mental health. Psychology major Iza Guzek, Arts ’23, was part of a team under the guidance of Dr. Stephen Saunders, professor of psychology, that investigated whether social media has a larger role in helping students open up about their mental health — or leads to students trivializing, or even glorifying, mental illness. The students surveyed more than a hundred 18- to 28-year-olds to learn how users of TikTok and Instagram perceive people posting on these venues about mental illness. The majority of respondents described them using terms such as “admirable,” “cool,” “brave” and “strong.”
The increasing use of social media to discuss mental health issues has helped to reduce stigma, Saunders and Guzek agree, but the pendulum may have swung a bit too far. “From our findings, we were glad to see that people disagree with the notion that the individuals [posting about mental health issues] come off as ‘scary’ or ‘dangerous,’” Guzek explains. “This shows that they do not view them in the typical ‘stigmatizing way’ so to speak. But what was surprising, yet supporting our hypothesis, was how a lot of participants strongly agreed to mental illness being portrayed as something ‘cool’ or ‘admirable.’” Early results suggest that this is particularly true of the social media platform TikTok.
“Getting students involved also shows them, hopefully, that anything about which they are curious can be studied.” Dr. Stephen Saunders
The team, which included Shea O’Connor, Arts ’24, and Christina Schmidt, Arts ’23, presented its research poster at the Wisconsin Psychological Association and the Marquette Undergraduate Research Symposium and has continued work on the project and corresponding paper. The goal is to present it at the Association for Psychological Science for the 2024 Global Psychological Science Summit in October. Guzek is committed to carrying the research forward and building upon it in her future career.
“At Marquette, we are taught cura personalis , which means care for the whole person,” Guzek says. “We are advised to Be The Difference. Research such as this is one of the ways I can care for others and make a difference. Even after graduating, I feel it is my mission.”
The Guzek-O’Connor-Schmidt team was one of four that conducted independent research under Saunders’ mentorship last year.
Another group studied the associations of prosocial and antisocial behavior with mental health both on and offline. Conducted by Liam Pyne, ’24, and Pat Swanson, a rising junior psychology and economics major, the study examined the social media behaviors and reactions of 275 survey participants and concluded that prosocial behavior leads to increases in mental health and self-esteem, especially among people who know each other, while antisocial behavior leads to negative feelings — especially among strangers online.
Saunders says that in addition to learning about the scientific process, students learn about themselves and what they may want to pursue as a career. “Getting students involved also shows them, hopefully, that anything about which they are curious can be studied.”
Related Articles

Stories at MU
Class of 2024 gives advice to incoming first-year students

MU+ Milwaukee & Beyond, Stories at MU
Food for thought

Getting to Know Keyes Dean of the College of Business Administration Andrew DeGuire
- You are here:
- American Chemical Society
- Discover Chemistry
- Tiny Matters

Pig hearts in people: Xenotransplantation's long history, current promise, and the ethical use of brain-dead people in research
In the early hours of January 7, 2022, David Bennett was out of options. At just 57 years old, he was bedridden, on life support, and in desperate need of a heart transplant for which he was ineligible. Yet Bennett would go on to live for two more months — not with a human heart, but with a heart from a pig. David Bennett was the first case of a pig heart being transplanted into a human, an example of xenotransplantation — when the cells, tissues or organs from one species are transplanted into another. In the United States, over 100,000 kids and adults are currently on the national transplant waiting list, and every day around 17 people on that list die while waiting.
In today's episode, we cover the science that made Bennett’s transplant possible, and what doctors learned from him that helped the next heart xenotransplant recipient, Lawrence Faucette, live even longer. We also get into some of the ethics conversations surrounding xenotransplantation work — not just questions about the use of animals like pigs and baboons, but experiments with recently deceased, i.e. brain dead, people.
Transcript of this Episode
Sam Jones: In the early hours of January 7, 2022, David Bennett was out of options. At just 57 years old, he was bedridden, on life support, and in desperate need of a heart transplant for which he was ineligible. Yet Bennett would go on to live for two more months — not with a human heart, but with a heart from a pig.
Welcome to Tiny Matters, I’m Sam Jones and today I’m joined by my co-host, science communicator and producer, George Zaidan. George, welcome to Tiny Matters!
George Zaidan: Thanks so much for having me! I’m especially glad to be here because this is such a fascinating story. David Bennett was the first case of a pig heart being transplanted into a human, an example of xenotransplantation — when the cells, tissues or organs from one species are transplanted into another. In the United States, over 100,000 kids and adults are currently on the national transplant waiting list, and every day around 17 people on that list die while waiting.
Sam: So today on the show we’re going to talk about the science and history that made Bennett’s transplant possible, and what doctors learned from him that helped the next heart xenotransplant recipient, Lawrence Faucette, live even longer. We’ll also get into some of the ethics conversations surrounding xenotransplantation work — not just questions about the use of animals like pigs and baboons, but experiments with recently deceased people.
Throughout history, you’ll find stories of human-beast hybrids, for instance the ancient Egyptian god Anubis — body of a man with the head of a dog — or the sphinx in Ancient Greece, who was part woman, part bird, part lion. Starting centuries ago, there are records of taking the blood and skin from other animals and using them in humans.
Muhammad Mohiuddin: Even in the early 1600s, they tried to put a dog skull in a nobleman just to repair a defect there. However, the church disallowed it and they took it out and the nobleman died.
George: That’s Muhammad Mohiuddin, a professor of surgery and the Director of the Cardiac Xenotransplantation Program at the University of Maryland School of Medicine. He co-led the team that performed both David Bennett and Lawrence Faucette’s surgeries.
He told us that in the early 1900s, there was a rise in xenotransplantation attempts using organs from a number of species, but the survival rate was low — like hours, not even days. That’s not surprising given what we now know about the immune system, and the role it plays in an organ being rejected by a transplant recipient’s body after what may have looked like a successful surgery.
Muhammad has dedicated his life to understanding the immune response to xenotransplantation and how to temper it. And we’re going to get into that a bit later in this episode. But first let’s talk about a few milestones in the xenotransplantation world. Because immunosuppressant drugs weren’t available in the early 1900s, doctors were at a loss, and by the mid 1920s many had moved away from xenotransplantation. And it stayed that way for decades.
Sam: A big turning point came in 1963, when surgeon Keith Reemtsma at Tulane University transplanted the kidneys of chimpanzees and, in one case, a rhesus monkey, into people. One of the chimpanzee kidney recipients survived an astonishing 9 months. That huge jump in survival time was attributed to new immunosuppressive drugs that kept the immune system from immediately flaring up and rejecting the organ. Unfortunately, the other xenotransplant recipients died within a couple of months, either due to immune rejection or because their immune system was so depleted that they developed an infection they would have typically be able to fight off.
George: A year later, in 1964, a doctor tried the first cardiac xenotransplantation in humans, using a chimpanzee heart. Unfortunately, the patient died within a couple of hours. But twenty years later, Baby Fae really put cardiac xenotransplantation on the map. In 1984, a surgeon named Leonard Bailey at Loma Linda University Medical Center in California transplanted a baboon heart into 12-day-old Stephanie Fae Beauclair, better known as Baby Fae.
Baby Fae was born with hypoplastic left heart syndrome. This is a condition where the left side of the heart is so underdeveloped that it has trouble pumping blood. In Baby Fae’s case it was so severe that she wouldn’t have survived. As her heart failed, Bailey performed the surgery. Just hours later, her new baboon heart began beating. Sadly, just a few weeks after that, Baby Fae’s immune system rejected the heart and she passed away. But in the years since then, researchers have made huge strides in immunosuppression medications, and treatment approaches and have also moved away from using organs from non-human primates.
Muhammad Mohiuddin: We found out that chimpanzees or baboons, though very similar to humans, there are several disadvantages of transplanting their organs.
Sam: One disadvantage is that they carry diseases that can easily transmit to us, including simian immunodeficiency viruses or SIV, notorious for crossing into humans and causing HIV. Muhammad told us the focus soon began to shift to pigs.
Muhammad Mohiuddin: They are domestic animals raised well in captivity, they grow very fast. So for a human of about 80 kilograms, you need a pig of only one year of age, and that heart or other organs will be compatible with human organ size.
Sam: Researchers also know a lot about the pig genome, which means we can tinker with their genetics.
Muhammad Mohiuddin: So with the technology now we have to modify genes, we can alter their genes and take out the genes that are immunogenic to humans and then put in some human genes to make them more compatible to human.
Sam: This is a huge deal, because it means pig heart xenotransplant recipients are no longer fully reliant on immunosuppressants. Researchers are able to remove the genes in pigs that code for the production of molecules that trigger the human immune system. At the same time, researchers can now insert genes that make a pig’s heart appear to be more human to our immune system.
George: This is possible thanks to cloning. The company Muhammad and his colleagues work with is called Revivicor, which is a spinoff of PPL Therapeutics, which is the company that cloned Dolly the sheep.
Revivicor retrieves eggs from the ovaries of female pigs, removes the DNA and replaces it with new DNA. And in that new DNA, the researchers removed three genes that are responsible for rejection of pig organs by human immune systems. The gene for a growth hormone receptor was also removed to prevent the pig heart from growing too much once transplanted.
Sam: Six human genes were also inserted into the new DNA, which would help with immune acceptance. They then placed the eggs, now fertilized, back in the pig’s uterus where they developed into embryos. There can still be some variation in genes even with these genetic modifications, but the team is ultimately working to create a stable breeding line where pigs who show stable genetics would then be bred with each other so you’d always get these 10 desired genetic mutations in their offspring. You’d no longer need cloning.
So by 2021, Muhammad and his colleagues had not only genetically modified pigs but were using better immunosuppressants, including a new anti-CD40 antibody, which targets an incredibly important immune pathway in humans.
Muhammad Mohiuddin: So at that time, we thought that this is the right time to take this to humans and save millions of people throughout the world who cannot get a human heart either because of the shortage or because of certain conditions these patients have, which make them ineligible for a human heart.
George: So they approached the FDA. And although xenotransplantation surgery is not yet approved, it falls under “compassionate use” rules for emergency situations, similar to how new cancer drugs that are not FDA approved can be used in a terminal patient, with their consent of course. And that brings us back to David Bennett. Muhammad told us that, after going back and forth several times with the FDA, they were granted compassionate use approval.
Muhammad Mohiuddin: And then we presented this idea to Mr. Bennett and he graciously accepted it saying that even if it doesn't help me, it may help other people. So he volunteered his life for this purpose.
George: On January 7th, 2022, cardiothoracic surgeon Bartley Griffith, alongside Muhammad and the rest of the team at the University of Maryland Medical Center, performed the first successful xenotransplantation surgery placing a genetically modified pig heart into a person.
Muhammad Mohiuddin: When we were doing this transplant, nobody knew what to expect because there was no precedence. So we even told the patient, and the patient understood that there is not even a guarantee that he will recover from this transplant. Even wake up. So every day from that point on, we took it as success. And finally he lived for 60 days.
George: Now for context, the first person to receive a heart transplant from another human only lived for 18 days. Over the course of David Bennett’s 60 days before his immune system ultimately rejected the pig heart he not only got more time with his family — Muhammad and the team were also learning from him.
Muhammad Mohiuddin: At one point we had to stop one of the major immunosuppressive drugs for a little bit. We did not know what levels of the CD40 that we used very successfully in baboons is enough for this particular patient, because of course he’s not a baboon. And also there were so many other issues going on simultaneously that we had difficulty maintaining the levels of that drug.
Sam: At one point David Bennett’s immune system took such a dip that they actually needed to give him intravenous immunoglobulins or IVIG, which is an antibody serum from healthy volunteers.
Muhammad Mohiuddin: But what we didn't realize at that time, that pool serum also had antibodies against pigs. So we believe that those antibodies kind of attack the pig heart and caused the graft to fail.
Sam: In addition, the pig heart David Bennett received was unknowingly infected with a latent virus called CMV.
Muhammad Mohiuddin: We do look for the viruses in these donors. However, we were not able to detect this virus because it was very deep seated. Since this patient, we have developed a lot of new techniques to detect even these deep-seated viruses. And in the second case, we were able to screen that virus out, so we didn’t see any issue with any virus in the second case.
So if you say, what were the reasons the first patient lived for only 60 days, not a hundred days? I would say the number one was his own condition, a very vulnerable condition where we could not maintain the immunosuppression that we wanted to give to protect the heart from rejection. Number two was the IVIG that we gave acted against the heart. And number three, the virus may have caused some kind of initial damage or immune reaction that may have caused the destruction of the heart cells, causing rejection or graft failure.
Sam: Right now, the team at the University of Maryland is continuing to evaluate patients for future pig heart transplants while also optimizing their approach.
Muhammad Mohiuddin: Every transplant, we will learn something, but we want to improve and not repeat. Everything that we learned in the first transplant that we thought that had gone wrong, we never repeated it.
Sam: The second patient, 58 year old Lawrence Faucette, received a genetically modified pig heart on September 20, 2023 and lived for nearly 6 weeks before his body rejected it. Faucette, a retired U.S. Navy veteran and histology technician at the NIH, was able to spend that time with family members and even begin physical therapy.
George: There has been so much work to get to this point, and people like David Bennett and Lawrence Faucette have been invaluable in that progress. But there are also many other species, including pigs but also many non-human primates, that have played an essential role in understanding immune rejection. One of the main reasons the FDA granted compassionate use approval for David Bennett’s surgery was a landmark study done by Muhammad and his team, in which a pig heart was transplanted into a baboon who went on to survive for nearly for 3 more years.
Sam with Muhammad Mohiuddin: Xenotransplantation is, in my opinion, really important, but it's not like you can just go from pig to human and not do a lot of things in between. And a pig heart, it's still a pig. And some people might get upset that it's a pig. And so, how do you navigate those conversations surrounding, ‘is it ethical to have all of these pigs that are being raised for this purpose or working with baboons?’ I’m just kind of curious how you manage that or how you view that in your work.
Muhammad Mohiuddin: Every single drug that we use these days, or every single procedure, has been tested in an animal before we used it. So it is unfortunate, we all love animals and we don't want to use them for this purpose, but we don't have any computational models or anything else to replace a live human biology. And I've been doing it for the past 33 years. We do receive a lot of, you'll say hate mails or we've been questioned a lot. But I was very surprised when we did these two humans — 99% of the mail or the communication I received was very positive. A lot of people said, “where were you 10 years ago when we lost our dear one?” It is unfortunate that to keep one human alive, we have to kill one pig. But again, 90,000 pigs are killed per day in the United States for our dietary needs. That's one of the reasons that pigs were chosen because they are already being sacrificed every day for other purposes. There are about 105 products that we use — even maybe the makeup you're using — was derived from pig products. To me, saving one life takes precedence over everything. And just imagine if this becomes a routine. Every 80 minutes a patient dies waiting for an organ. So you can save millions of lives throughout the world, just within a year.
George: But baboons and other non-human primates are not the only option for studying xenotransplant rejection. Another approach is experimenting in people who are recently deceased. In 2022, surgeons at NYU made headlines when they transplanted pig hearts with the same 10 genetic changes as David Bennett’s donor pig heart into two recently deceased people who were then monitored for three days.
Sam: I came across this side of xenotransplantation research in a story titled, “The Allure and Dangers of Experimenting With Brain-Dead Bodies,” written by Jyoti Madhusoodanan, who is a freelance science journalist based in Portland, Oregon. A couple years before writing the story, Jyoti was working on an article about xenotransplantation for the Journal of the American Medical Association. David Bennett had just received his pig heart transplant.
Jyoti Madhusoodanan: There was a lot of news and excitement about it, and I was speaking with researchers about not just the transplant itself, but this massive body of work they had done leading up to that moment. And in the course of that conversation, it came about that some of that research had been done in people who were recently deceased.
George: Recently deceased people are sometimes referred to as brain dead people or decedents. And although they’re legally dead, machines keep their blood pumping and air flowing into and out of their lungs. What Jyoti soon learned was that using recently deceased people opens up a massive can of worms when it comes to regulation. In the U.S., since 1991 we’ve had the Federal Policy for the Protection of Human Subjects which is also known as the “Common Rule.”
Jyoti Madhusoodanan: And the Common Rule is basically a set of federal policies that are meant to protect people who participate in scientific research. So the common rule covers things like making sure that protected classes of people like children or communities that are especially vulnerable, like people who are in prison or pregnant people, are protected from experiments that could be harmful to them or that might in some way violate their freedoms, for instance.
George: And over time the Common Rule has expanded and shifted to be more encompassing of different kinds of research.
Jyoti Madhusoodanan: It also covers biospecimens, which are things like blood or tissue or organs. And essentially for all of these things that are done with people who are living, whether they're minors or not, or whether they're tissue samples or not, you have things like informed consent, meaning no one can use your tissue, a blood sample from you for a genetic test or whatever, without your consent. There's also institutional review boards which offer oversight within institutions.
Sam: Researchers proposing to do work with living people have to get approval from an institutional review board or IRB before moving ahead with a project.
Jyoti Madhusoodanan: And there's also another set of rules about research involving tissues or bodies of people who are deceased. But what I discovered while reporting this is that recently deceased people, people who've been declared brain dead are in this gray area. So there's not a lot of regulation about how to do research with recently deceased subjects. There are groups of researchers and ethicists who've developed guidance to help the community, but none of that is formal regulation per se.
Sam: And what that does is open things up to a range of treatment, both good and bad.
Jyoti Madhusoodanan: There were some truly wonderful stories from the U.S. actually, where it was moving to see how much researchers cared about doing things the right way. They sort of adhered to the highest standards they could find because there weren't any other standards for them, which was really heartwarming and wonderful to see. At the same time, there was this one instance from India that really stood out. It started out as a U.S.-based company that wanted to conduct experiments with trying to revive brain dead subjects, and they didn't get the consent they needed in the U.S. So then they moved out of the U.S. to, they say, a few different countries, and didn't really get off the ground because of the pandemic. But there is one institute in India where the researcher says they have been continuing that sort of work on their own without the US company being involved, and they are using a combination of stem cells and other treatments to literally revive brain activity in people who've suffered brain injuries during traffic accidents.
Sam: Although they’re not working in the xenotransplantation space, at least to our knowledge, it gives you a sense of how so much gray area surrounding this regulation means things can get dicey real fast.
Jyoti Madhusoodanan: All the researchers that I spoke with about that work described it as premature. Ethicists have published review articles, opinion pieces, describing how that work is essentially exploitative of grieving families by giving them false hope that their loved ones might come back to life. And if you contrast that with the xenotransplantation work, where there has been decades of work in animal models to see what needs to be done to make that process feasible for humans. And then they carried out the work in recently deceased subjects and then went into a living human, which is a very methodical, systematic way of bringing the research to a point where it's acceptable to experiment on a human being.
George: The 2022 NYU study where pig hearts were transplanted into two recently deceased people was a great example of decedent work being done ethically. One of the people in that study was a woman named Alva Capuano.
Jyoti Madhusoodanan: Alva Capuano had dealt with so many health issues over the course of her life that really epitomized the need for xenotransplant research.
George: In her reporting, Jyoti had the opportunity to speak with Alva’s son Tim.
Jyoti Madhusoodanan: The conversation I had with Tim really framed for me how when research is done well, how it can really build trust with people who participate. His mom had signed up to donate her own organs because of her complicated life experience and knowing the value of a donated organ. And unfortunately, it turned out that because of her complicated medical history, when they were trying to arrange this gift at the end of her life, the family kept running into rejection of people telling them they can't use this organ or that organ or the other. And it was this really traumatizing, grueling process for them. And they were really reaching the end of it, end of that process when they heard about the possibility of her participating in this study, in this experiment.
George: The medical team at NYU explained the process to the Capuano family and they decided it was the right move. Alva wanted to contribute to research that could ultimately save the lives of people like her who were in need of a transplant.
Jyoti Madhusoodanan: And apparently, Tim said during our interview, that at the time, during those few days that they were conducting the experiment, the researchers would call them. So they had frequent updates about how things were going, what the researchers were learning from what they were doing, and things like that, which is just a really sweet example of how science that engages the people that it hopes to help can do so much more when it's done well.
Sam: In this country, every 8 minutes someone is added to the transplant waiting list. As of March of this year over 3,000 children and adults were waiting for a new heart. And now, cardiac xenotransplantation is no longer some sci-fi pipe dream. There are a lot of patients and doctors out there with a lot of hope.
Let's tiny show-and-tell.
George: All right, let's do it.
Sam: What do you think, George? First tiny show-and-tell.
George: Yeah, I know. Does that mean I should go first or second?
Sam: You decide.
George: Normally I do rock, paper, scissors, but I'll just go first.
Sam: Okay, go for it.
George: My tiny show-and-tell has to do with a disease called progeria. Have you ever heard of it?
Sam: I've heard of it, but I can't quite remember, so remind me.
George: So it's basically... It's kids with super accelerated aging. So it's like a 10-year-old who looks like a 50-year-old, a 27-year-old who looks like an 85-year-old, that kind of thing. And interestingly, I didn't know this, but it's caused by a single-point mutation in one gene. It's a really, really rare disease. It only affects... I think there's only 18 living patients in the US.
And the thing that was highlighted by this article that I was reading about this is that there are about 7,000 genetic disorders for which we know the mutation. 85% of those disorders are super, super rare, and only a few hundred of the 7,000 currently have any sort of treatment, and progeria is one of those. There was no treatment. So researchers created a protein that actually fixes this point mutation. They tested it in mice. It showed a lot of promise. And this is where you get to guess. Can you guess how they created this protein that fixed the problem in mice?
Sam: How they created it? It's like an enzyme? Did they do something in pigs?
George: I actually don't know what animal they did it in. So this is actually... Maybe you're the wrong person to ask because you know about these things, but I feel like most people would just be like, "CRISPR. They used CRISPR, right?" And the shocker is they did not. They used directed evolution. So not all work being done in genetics and proteins is CRISPR, which I thought was cool.
So the next step is to do a clinical trial in humans, which they want to do in the next two years. And the NIH director, he's one of the labs that did this work. So I thought that was also very, very cool. And that's the limit of my... I'm a chemist by training, so that's... Everything I just told you is the limit of my biology knowledge.
Sam: That's really fascinating. In the episode description, we always link to the article or the paper so that if someone is listening and they want to really deep dive, then they know where to go for it.
George: Great. It's a nature paper, so it'll be fun.
Sam: Today I have something very different for you. I have a cool cicada fact for you that was actually brought to my attention by a colleague's five-year-old daughter named Ellie. So thank you, Ellie. Before I get to Ellie's fact, I'm going to talk a little bit about cicadas. So just bear with me, George. I know you're not a big fan.
George: Yeah, I'm not. Insects are not my jam. But...
George: Go ahead.
Sam: Well, you're going to have to suck it up for a sec. All right. There's of course been a lot of cicada talk in recent years with people particularly excited about the magic cicada genus. Those are the ones that hang out underground in their nymphal stage for up to 17 years and then have this big emergence. They're what are called periodical cicadas, and groups of them called broods will emerge all at once in a specific area and year based on a very predictable cycle of development, which is kind of cool that you can say, "Okay, they're back underground, but they're actually going to come out now in 13 years or 15 years or whatever it may be."
So after female cicadas mate, they go to lay their eggs. And when they do that, they use something called an ovipositor to cut through wood, typically trees, where they then lay those eggs. So this ovipositor kind of looks like a serrated sword and it sticks out the female cicadas abdomen.
George: Love it.
Sam: Yeah. It's a great visual. And you would think to cut through wood, it must be pretty strong, right? So a few years back, researchers hypothesized that it might contain different inorganic elements to make it strong, including different metals. So they used a couple different techniques. They used energy dispersive, X-ray spectroscopy and electron microscopy to identify and quantify the elements that were actually present in the ovipositor and then be able to map their locations as well. And so they found 14 inorganic elements including silicon, iron, and zinc. So cicadas are part metal, and that was Ellie's fact.
George: That's amazing.
Sam: And then I went a little bit deeper, but don't worry, I'm almost done with these insects. So something else that I really found fascinating was that a lot of these, what are called cuticles on insects, so this is technically what it’s called. The ovipositor is a cuticle. A lot of them are reinforced with metal, including spider fangs,
George: Oh no.
Sam: Insect mandibles, which are the appendages that are near the mouth that help them crush or bite or cut things, and also, the jaws of marine polychaetes, which are these very creepy-looking worms that you find in the water. So just a fun little fact. I hope you sleep well tonight, George.
George: I guarantee you I will not. Thanks, Sam.
Thanks for tuning in to this week’s episode of Tiny Matters, a production of the American Chemical Society. This week’s script was written by Sam, who is also our executive producer, and was edited by me, George Zaidan, and by Michael David. It was fact-checked by Michelle Boucher. The Tiny Matters theme and episode sound design is by Michael Simonelli and the Charts & Leisure team.
Sam: Thanks so much to Muhammad Mohiuddin and Jyoti Madhusoodanan for joining us. To be featured in our bonus series, “Tiny Show and Tell Us,” write in to tinymatters@acs.org with science news you’re itching to share, a science factoid you love telling friends about, or maybe even a personal science story. We want to hear about it! And while you’re at it, subscribe to our newsletter! I’ve put links in the episode description. See ya next time!
George: Please don’t share insect stories anymore.
Sam: Only insect tiny show and tells from now on.
George: No insect stories…
Listen and subscribe
iHeartRadio
Accept & Close The ACS takes your privacy seriously as it relates to cookies. We use cookies to remember users, better understand ways to serve them, improve our value proposition, and optimize their experience. Learn more about managing your cookies at Cookies Policy .
1155 Sixteenth Street, NW, Washington, DC 20036, USA | service@acs.org | 1-800-333-9511 (US and Canada) | 614-447-3776 (outside North America)
- Terms of Use
- Accessibility
Copyright © 2024 American Chemical Society
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Dilemmas and solutions for sustainability-based engineering ethics: lessons learned from the collapse of a self-built house in changsha, hunan, china.

1. Introduction
2. materials and the self-built house collapse accident in changsha, 2.1. safety status in the field of housing and municipal engineering in china, 2.2. process of the self-built house collapse accident in changsha, 2.3. causes of the self-built house collapse accident in changsha.
- The original five-story building constructed by the owner, who violated laws and regulations, had inherent deficiencies in its quality. In 2003, the owner built a three-story house. In July 2012, the three-story building was demolished and replaced with a five-story (partially six-story) building, without specific location details, which are not provided in Figure 3 a. However, the involved owner, without fulfilling any approval procedures or obtaining any permissions, hired a retired construction worker from a building company to hand-draw the design drawings and personally procured construction materials. Moreover, the construction was carried out by an unqualified and mobile construction team. In the construction process, self-mixed concrete with high levels of sand and silt content and low strength was used, particularly the minimum compressive strength of the concrete used in the three columns on the east side of the second floor, which was only 4.3 MPa, significantly lower than the required 20 MPa [ 75 ]. The compressive strength of the mortar used in the masonry of the walls on the first and second floors was only 0.4 MPa, which fell far below the required 2.5 MPa [ 76 ]. The building adopted a masonry structure, in which the walls and columns constructed with solid blocks and mortar served as the primary load-bearing components. While the first floor had solid walls, the walls from the second to fifth floor improperly used hollow or cavity walls, which had low load-bearing capacity and were no longer in compliance with the Code [ 76 ].
2.4. Rescue of the Self-Built House Collapse Accident in Changsha
3. dilemmas of engineering ethics, 3.1. identification of ethical dilemmas, 3.2. ethical dilemmas faced by engineers, 3.2.1. dilemma of technological ethics, 3.2.2. dilemma of interest ethics, 3.2.3. dilemma of responsibility ethics, 3.3. the dilemma of government credibility deficiency, 3.3.1. lack of public trust in engineering quality, 3.3.2. the decline of government credibility, 3.4. the dilemma of engineering ethics education, 3.4.1. insufficient emphasis on the interdisciplinary nature of engineering ethics, 3.4.2. detachment between theory and practice in engineering ethics education, 3.5. the collapse of the condominium building in florida, us, 4. solutions of engineering ethics, 4.1. enhancing the ethical perspectives of engineers, 4.1.1. enhancing public participation in engineering decision-making, 4.1.2. effective implementation of technical assessment in engineering, 4.1.3. establishing a sound legal and ethical framework for engineering, 4.2. promoting credibility of government, 4.2.1. deepen administrative system reform and establish a system of government credibility, 4.2.2. actively mobilize the power of the media and create a healthy ethical discourse environment in engineering, 4.2.3. adhere to the concept of public nature and service and establish a people-centered philosophy, 4.3. strengthening engineering ethics education, 4.3.1. adding engineering ethics-related courses to the curriculum, 4.3.2. strengthening engineering ethics education in engineering practice, 4.3.3. strengthening professional ethics training for practitioners, 4.4. solutions taken after the collapse accidents, 4.4.1. the self-built house collapse accident in changsha, 4.4.2. the condominium building collapse in florida, us, 4.5. the ethical analysis and decision-making model for engineering failures, 5. conclusions, author contributions, data availability statement, acknowledgments, conflicts of interest.
- Xu, F.Y.; Zhang, M.J.; Wang, L.; Zhang, J.R. Recent highway bridge collapses in China: Review and discussion. J. Perform. Constr. Facil. 2016 , 30 , 04016030. [ Google Scholar ] [ CrossRef ]
- Lu, Y.E.; Zhang, L.M. Progressive collapse of a drilled-shaft bridge foundation under vessel impact. Ocean Eng. 2013 , 66 , 101–112. [ Google Scholar ] [ CrossRef ]
- Shi, X.F.; Zhou, Z.J.; Ruan, X. Forensic diagnosis on the overall collapse of a composite box-girder bridge. Struct. Eng. Int. 2018 , 28 , 51–59. [ Google Scholar ] [ CrossRef ]
- Zhao, X.H.; Cheng, W.C.; Shen, J.S.; Arulrajah, A. Platform collapse incident of a power plant in Jiangxi, China. Nat. Hazards 2017 , 87 , 1259–1265. [ Google Scholar ] [ CrossRef ]
- Tan, J.-S.; Elbaz, K.; Wang, Z.-F.; Shen, J.S.; Chen, J. Lessons learnt from bridge collapse: A view of sustainable management. Sustainability 2020 , 12 , 1205. [ Google Scholar ] [ CrossRef ]
- Chen, X.; Qiao, W. A hybrid STAMP-fuzzy DEMATEL-ISM approach for analyzing the factors influencing building collapse accidents in China. Sci. Rep. 2023 , 13 , 19745. [ Google Scholar ] [ CrossRef ]
- Wang, Y.N.; Chen, Q.; Peng, J.-R.; Chen, J. A brief report on the collapse of self-built houses on 29 April 2022, in Changsha, China. Int. J. Environ. Res. Public Health 2023 , 20 , 61. [ Google Scholar ] [ CrossRef ]
- Huang, M.S.; Gül, M.; Zhu, H.P. Vibration-based structural damage identification under varying temperature effects. J. Aerosp. Eng. 2018 , 31 , 4018014. [ Google Scholar ] [ CrossRef ]
- Deng, Z.H.; Huang, M.S.; Wan, N.; Zhang, J.W. The current development of structural health monitoring for bridges: A review. Buildings 2023 , 13 , 1360. [ Google Scholar ] [ CrossRef ]
- Huang, M.S.; Zhang, J.W.; Hu, J.L.; Deng, Z.H.; Wan, N. Nonlinear modeling of temperature-induced bearing displacement of long-span single-pier rigid frame bridge based on DCNN-LSTM. Case Stud. Therm. Eng. 2024 , 53 , 103897. [ Google Scholar ] [ CrossRef ]
- Huang, M.S.; Ling, Z.Z.; Sun, C.; Lei, Y.Z.; Xiang, C.Y.; Wan, Z.H.; Gu, J.F. Two-stage damage identification for bridge bearings based on sailfish optimization and element relative modal strain energy. Struct. Eng. Mech. 2023 , 86 , 715–730. [ Google Scholar ] [ CrossRef ]
- Huang, M.S.; Zhang, J.W.; Li, J.; Deng, Z.; Luo, J. Damage identification of steel bridge based on data augmentation and adaptive optimization neural network. Struct. Health Monit. 2024 . [ Google Scholar ] [ CrossRef ]
- Zhang, J.W.; Huang, M.S.; Wan, N.; Deng, Z.; He, Z.; Luo, J. Missing measurement data recovery in structural health monitoring: The state and challenges. Measurement 2024 , 231 , 114528. [ Google Scholar ] [ CrossRef ]
- Pfatteicher, S.K.A. “The Hyatt Horror”: Failure and Responsibility in American Engineering. J. Perform. Constr. Facil. 2000 , 14 , 62–66. [ Google Scholar ] [ CrossRef ]
- Zheng, Z.; Liao, W.J.; Lin, J.R.; Zhou, Y.C.; Zhang, C.; Lu, X.Z. Digital twin-based investigation of a building collapse accident. Adv. Civ. Eng. 2022 , 2022 , 9568967. [ Google Scholar ] [ CrossRef ]
- Yan, X.L.; Kim, Y.-C. A conceptual framework of ITSMCA for a building collapse accident. Eng. Constr. Archit. Manag. 2018 , 25 , 721–737. [ Google Scholar ] [ CrossRef ]
- Ma, D.L.; Zhang, C.H.; Zhao, L.; Huang, Q.J.; Liu, B.Z. An analysis of the evolution of public sentiment and spatio-temporal dynamics regarding building collapse accidents based on Sina Weibo data. ISPRS Int. J. Geo.-Inf. 2023 , 12 , 388. [ Google Scholar ] [ CrossRef ]
- Dutta, S. Triple bottom line reporting: An Indian perspective. Interdiscipl. J. Contemp Res. Bus. 2012 , 3 , 652–658. [ Google Scholar ]
- Michelfelder, D.; Jones, S.A. Sustaining engineering codes of ethics for the twenty-first century. Sci. Eng. Ethics 2013 , 19 , 237–258. [ Google Scholar ] [ CrossRef ]
- Tziner, A.; Persoff, M. The interplay between ethics, justice, corporate social responsibility, and performance management sustainability. Front Psychol. 2024 , 15 , 1323910. [ Google Scholar ] [ CrossRef ]
- Brauer, C.S. Just sustainability? Sustainability and social justice in professional codes of ethics for engineers. Sci. Eng. Ethics 2013 , 19 , 875–891. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Miller, G.R.; Brumbelow, K. Attitudes of incoming civil engineering students toward sustainability as an engineering ethic. J. Prof. Issues Eng. Educ. Pract. 2017 , 143 , D4016002. [ Google Scholar ] [ CrossRef ]
- Mares-Nasarre, P.; Martinez-Ibanez, V.; Sanz-Benlloch, A. Analyzing sustainability awareness and professional ethics of civil engineering bachelor’s degree students. Sustainability 2023 , 15 , 6263. [ Google Scholar ] [ CrossRef ]
- Boateng, F.G. Exploring the collapse of buildings in urban settings. Proc. Inst. Civ. Eng.-Munic. Eng. 2020 , 173 , 187–195. [ Google Scholar ] [ CrossRef ]
- Chin, Y.-T.; Shen, S.-L.; Zhou, A.-N.; Chen, J. Foundation pit collapse on 8 June 2019 in Nanning, China: A brief report. Safety 2019 , 5 , 68. [ Google Scholar ] [ CrossRef ]
- Mentis, A.-F.; Papadopulos, J. Near-collapse buildings and unsafe sidewalks as neglected urban & public health issue: A qualitative study. Urban Sci. 2021 , 5 , 47. [ Google Scholar ] [ CrossRef ]
- Shakib, H.; Pirizadeh, M.; Dardaei, S.; Zakersalehi, M. Technical and administrative assessment of Plasco building incident. Int. J. Civ. Eng. 2018 , 16 , 1227–1239. [ Google Scholar ] [ CrossRef ]
- Ayodeji, O. An examination of the causes and effects of building collapse in Nigeria. J. Des. Built Environ. 2011 , 9 , 37–48. [ Google Scholar ]
- Ferjencik, M. Engineers need RUDENESS: An extension of Trevor Kletz’s approach to accident investigations. Process Saf. Prog. 2012 , 31 , 315–318. [ Google Scholar ] [ CrossRef ]
- Haghighattalab, S.; Chen, A.; Fan, Y.X.; Mohammadi, R. Engineering ethics within accident analysis models. Accid. Anal. Prev. 2019 , 129 , 119–125. [ Google Scholar ] [ CrossRef ]
- Sulaima, M.F.; Lew, H.S.; Lau, C.Y.; Lim, C.K.Y.; Azily, A.T. A case study of engineering ethics: Lesson learned from building collapse disaster toward Malaysian engineers. Eurasian J. Sci. Technol. 2014 , 3 , 21–30. [ Google Scholar ]
- Basart, J.M.; Serra, M. Engineering ethics beyond engineers’ ethics. Sci. Eng. Ethics 2013 , 19 , 179–187. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Li, D. Weakening and Reconstruction of the Local Government Credibility in China. Ph.D. Thesis, Wuhan University, Wuhan, China, 2011. (In Chinese). [ Google Scholar ]
- Lee, Y.S. Credibility of government’s commitment and aggregate productivity. J. Econ. Stud. 2017 , 35 , 221–238. [ Google Scholar ] [ CrossRef ]
- Newberry, B. The dilemma of ethics in engineering education. Sci. Eng. Ethics 2004 , 10 , 343–351. [ Google Scholar ] [ CrossRef ]
- Colby, A.; Sullivan, W.M. Ethics teaching in undergraduate engineering education. J. Eng. Educ. 2008 , 97 , 327–338. [ Google Scholar ] [ CrossRef ]
- Woo, J.J. Engineer’s social responsibility on engineering ethics―real lecture method. J. Humanit. Stud. 2010 , 37 , 251–281. [ Google Scholar ]
- Lovrin, N.; Vrcan, Z. Some considerations about engineering ethics. Strojarstvo 2009 , 51 , 239–248. [ Google Scholar ]
- Geistauts, G.; Baker, E.; Eschenbach, T. Grunwald proposed a frame of reference to makes it possible to elaborate in a transparent manner goals for analysis of the scope of ethics in engineering. Eng. Manag. J. 2008 , 20 , 21–28. [ Google Scholar ] [ CrossRef ]
- Abdul-Rahman, H.; Wang, C.; Saimon, M.A. Clients’ perspectives of professional ethics for civil engineers. J. S. Afr. Inst. Civ. Eng. 2011 , 53 , 2–6. Available online: https://hdl.handle.net/10520/EJC27067 (accessed on 2 July 2024).
- Grunwald, A. The application of ethics to engineering and the engineer’s moral responsibility: Perspectives for a research agenda. Sci. Eng. Ethics 2001 , 7 , 415–428. [ Google Scholar ] [ CrossRef ]
- Sobrino, J.A. Less and better. elements to achieve excellence in bridge design. Struct. Eng. Int. 2021 , 31 , 610–613. [ Google Scholar ] [ CrossRef ]
- Tscheon, R.T. A survey on the engineer’s sense of value. J. Eng. Edu. Res. 2009 , 12 , 21–30. (In Korean) [ Google Scholar ] [ CrossRef ]
- Baxter, J. How ethics can help professional engineers deliver a better service to the public. Proc. Inst. Civ. Eng.-Civ. Eng. 2019 , 172 , 148. [ Google Scholar ] [ CrossRef ]
- Sheen, G.C.-H.; Tung, H.H.; Wu, W.-C. Citizen journalism reduces the credibility deficit of authoritarian government in risk communication amid COVID-19 outbreaks. PLoS ONE 2021 , 16 , e0260961. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Koh, J.-S. A study on the effects of government policy PR on the credibility and fairness of public policies: With the focus on the government’s COVID-19 vaccination policy. Episteme 2021 , 26 , 83–113. [ Google Scholar ] [ CrossRef ]
- Xiang, P.C.; Guo, J.; Liu, Q.Q. How government credibility and social morality work in a public health emergency. a study of public quarantine willingness in COVID-19. Soc. Psychol. Study Soc. Issues 2020 , 20 , 443–461. [ Google Scholar ] [ CrossRef ]
- Ku, G. A study of the impact of government news credibility on government trust. J. Soc. Sci. 2014 , 53 , 173–190. (In Korean) [ Google Scholar ]
- Mishra, S.; Alowaidi, M.A.; Sharma, S.K. Impact of security standards and policies on the credibility of e-government. J. Ambient. Intell. Humaniz. Comput. 2021 . [ Google Scholar ] [ CrossRef ]
- Sohn, A. The relationship between government credibility and risk perception of the mad cow disease. Korean Public Health Res. 2010 , 36 , 27–34. (In Korean) [ Google Scholar ]
- Jung, S.H. Study about the impacts of the individual department’s brand on the formation of government’s credibility. J. Korea Contents Assoc. 2020 , 20 , 601–615. [ Google Scholar ] [ CrossRef ]
- Li, Z.G.; Wang, M.J.; Zhong, J.L.; Ren, Y.L. Improving the communication and credibility of government media in response to public health emergencies: Analysis of Tweets from the WeChat official accounts of 10 Chinese health commissioners. Front. Public Health 2022 , 10 , 900776. [ Google Scholar ] [ CrossRef ]
- Fan, Z.H.; Kim, Y.W. An analysis about the effects of media types and source types on Chinese publics’ credibility of news focusing on differences between government and private media, opinion leaders and ordinary people sources. Korean J. Commun. Inform. 2021 , 108 , 30–57. [ Google Scholar ] [ CrossRef ]
- Billington, D.P. Teaching ethics in engineering education through historical analysis. Sci. Eng. Ethics 2006 , 12 , 205–222. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Simpson, Z.; Bester, J.; Swanepoel, D.; Westman, C. Ethical demand and first-year civil engineering study: Applying virtue ethics. J. Prof. Issues Eng. Educ. Pract. 2018 , 144 , 05018006. [ Google Scholar ] [ CrossRef ]
- Bairaktarova, D.; Woodcock, A. Engineering ethics education: Aligning practice and outcomes. IEEE Commun. Mag. 2015 , 53 , 11–18. [ Google Scholar ] [ CrossRef ]
- Morrison, A.; Wallace, C. Making it strange: Disrupting assumptions about technology and ethics in engineering and computing education. IEEE Technol. Soc. Mag. 2022 , 41 , 81–90. [ Google Scholar ] [ CrossRef ]
- Atesh, M.H. Assessing Ethics Education Effectiveness in Engineering Programmes: A Multi-Phase Approach. PhD Thesis, The University of York, York, UK, 2019. [ Google Scholar ]
- Bird, S.J.; Sieber, J.E. Teaching ethics in science and engineering: Effective online education. Sci. Eng. Ethics 2005 , 11 , 323–328. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Li, J.; Fu, S. A systematic approach to engineering ethics education. Sci. Eng. Ethics 2012 , 18 , 339–349. [ Google Scholar ] [ CrossRef ]
- Martin, D.A.; Conlon, E.; Bowe, B. A multi-level review of engineering ethics education: Towards a socio-technical orientation of engineering education for ethics. Sci. Eng. Ethics 2021 , 27 , 60. [ Google Scholar ] [ CrossRef ]
- Huaquisto-Cáceres, S.; Hurtado-Chávez, E.V.; Chambilla-Flores, I.G.; Barrientos-Paredes, K.N. Environmental education and ethics in civil engineering study programs in the Puno region, Peru. Dyna 2022 , 89 , 18–27. [ Google Scholar ] [ CrossRef ]
- Haws, D.R. The importance of meta-ethics in engineering education. Sci. Eng. Ethics 2004 , 10 , 204–210. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chung, C. Comparison of cross culture engineering ethics training using the simulator for engineering ethics education. Sci. Eng. Ethics 2015 , 21 , 471–478. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sochacka, N.W.; Walther, J.; Pawley, A.L. Ethical validation: Reframing research ethics in engineering education research to improve research quality. J. Eng. Edu. 2018 , 107 , 362–379. [ Google Scholar ] [ CrossRef ]
- Swartz, B. Ethics in engineering education 4.0: The educator’s perspective. SAIEE Afr. Res. J. 2021 , 112 , 181–188. [ Google Scholar ]
- Bielefeldt, A.R.; Polmear, M.; Knight, D.; Swan, C.; Canney, N. Intersections between engineering ethics and diversity issues in engineering education. J. Prof. Issues Eng. Educ. Pract. 2018 , 144 , 04017017. [ Google Scholar ] [ CrossRef ]
- Bielefeldt, A.R.; Polmear, M.; Canney, N.; Swan, C.; Knight, D. Ethics education of undergraduate and graduate students in environmental engineering and related disciplines. Environ. Eng. Sci. 2018 , 35 , 684–695. [ Google Scholar ] [ CrossRef ]
- Bielefeldt, A.R.; Polmear, M.; Knight, D.; Canney, N.; Swan, C. Disciplinary variations in ethics and societal impact topics taught in courses for engineering students. J. Prof. Issues Eng. Educ. Pract. 2019 , 145 , 04019007. [ Google Scholar ] [ CrossRef ]
- Bielefeldt, A.R.; Lewis, J.; Polmear, M.; Knight, D.; Canney, N.; Swan, C. Educating civil engineering students about ethics and societal impacts via cocurricular activities. J. Civ. Eng. Edu. 2020 , 146 , 04020007. [ Google Scholar ] [ CrossRef ]
- Yin, S.; Zhang, N. Enhancing engineering ethics education (EEE) for green intelligent manufacturing: Implementation performance evaluation of core mechanism of green intelligence EEE. Front. Psychol. 2022 , 13 , 926133. [ Google Scholar ] [ CrossRef ]
- Zhong, B.T.; Xing, X.J.; Jiao, L.; Wu, H.T.; Sun, J. Situation of engineering ethics education of postgraduates in China: A preliminary investigation. Int. J. Eng. Edu. 2023 , 39 , 1154–1166. [ Google Scholar ]
- Ministry of Housing and Urban-Rural Development of the People’s Republic of China. Available online: https://zlaq.mohurd.gov.cn/fwmh/bjxcjgl/fwmh/pages/default/index.html (accessed on 2 July 2024).
- Ministry of Emergency Management of the People’s Republic of China. Available online: https://www.mem.gov.cn/gk/sgcc/tbzdsgdcbg/2023dcbg_5532/202305/P020230521599708081558.pdf (accessed on 23 January 2024).
- GB 50010-2010 ; Code for Design of Concrete Structures. Ministry of Housing and Urban Rural Development of the People’s Republic of China: Beijing, China, 2015.
- GB 50003-2011 ; Code for Design of Masonry Structures. Ministry of Housing and Urban Rural Development of the People’s Republic of China: Beijing, China, 2011.
- GB 50292-2015 ; Standard for Appraisal of Reliability of Civil Buildings. Ministry of Housing and Urban Rural Development of the People’s Republic of China: Beijing, China, 2015.
- Lu, X.; Guan, H.; Sun, H.; Li, Y.; Zheng, Z.; Fei, Y.; Yang, Z. A preliminary analysis and discussion of the condominium building collapse in surfside, Florida, US, June 24, 2021. Front. Struct. Civ. Eng. 2021 , 15 , 1097–1110. [ Google Scholar ] [ CrossRef ]
- Parkinson, R.W. Speculation on the role of sea-level rise in the tragic collapse of the Surfside condominium (Miami Beach, Florida, USA) was a bellwether moment for coastal zone management practitioners. Ocean Coast. Manag. 2021 , 215 , 105968. [ Google Scholar ] [ CrossRef ]
- ACI-318 ; Building Code Requirements for Structural Concrete. American Concrete Institute: Farmington Hills, MI, USA, 2019.
- Kong, X.X.; Smyl, D. Investigation of the condominium building collapse in Surfside, Florida: A video feature tracking approach. Structures 2022 , 43 , 533–545. [ Google Scholar ] [ CrossRef ]
- Smith, N.M.; Zhu, Q.; Smith, J.M.; Mitcham, C. Enhancing engineering ethics: Role ethics and corporate social responsibility. Sci. Eng. Ethics 2021 , 27 , 28. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mitcham, C. The true grand challenge for engineering: Self-knowledge. Issues Sci. Technol. 2014 , 31 , 19–22. [ Google Scholar ]
- The Legislative Affairs Commission of the Standing Committee of the National People’s Congress of the People’s Republic of China. The Civil Code of the People’s Republic of China ; China Law Press: Beijing, China, 2021.
- Wang, H.F.; Xu, Z.W.; Wang, H. The research and decision-making model of engineering ethics based on the WSR methodology. Ind. Innov. 2021 , 2 , 104–106. Available online: https://qikan.cqvip.com/Qikan/Article/Detail?id=7103758732 (accessed on 2 July 2024). (In Chinese).
Click here to enlarge figure
| Year | Number of Accidents | Number of Deaths | Number of Major Accidents * | Number of Deaths in Major Accidents |
|---|---|---|---|---|
| 2015 | 442 | 554 | 22 | 85 |
| 2016 | 634 | 735 | 27 | 94 |
| 2017 | 692 | 807 | 23 | 90 |
| 2018 | 735 | 841 | 22 | 87 |
| 2019 | 786 | 921 | 24 | 110 |
| 2020 | 695 | 798 | 22 | 89 |
| 2021 | 736 | 823 | 16 | 68 |
| 2022 | 564 | 640 | 12 | 52 |
| Date | Building Name | Place | Fatalities /Injuries | Cause of Collapse |
|---|---|---|---|---|
| 29 December 2014 | Gymnasium of High School affiliated to Tsinghua University | Beijing | 10/4 | Construction mistakes |
| 16 May 2019 | Factory 1#, 148 Zhaohua Road | Shanghai | 12/13 | Design errors, Construction mistakes |
| 20 May 2019 | Steel building | Baise, Guangxi | 6/87 | Illegal contracting, Design errors, Construction mistakes, Rain and wind |
| 27 June 2019 | Building 7#, Lotus Riverside View Garden | Shanghai | 1/0 | Construction mistakes |
| 8 July 2019 | Shenzhen Sports Center | Shenzhen, Guangdong | 3/3 | Construction mistakes |
| 7 March 2020 | Xinjia Hotel | Quanzhou, Fujian | 29/42 | Construction mistakes (illegal enlargement) |
| 29 August 2020 | Juxian Restaurant | Linfen, Shanxi | 29/28 | No professional design, illegal enlargement |
| 19 June 2021 | Self-built house | Chenzhou, Hunan | 5/7 | No professional design, Construction mistakes |
| 12 July 2021 | Four Seasons Open Source Hotel | Suzhou, Jiangsu | 17/5 | Construction mistakes |
| 16 July 2021 | Rest Hall | Yongan, Fujian | 8/2 | Design errors, Construction mistakes |
| 23 November 2021 | Lakeside Hotel | Jinhua, Zhejiang | 6/6 | Design errors, Construction mistakes |
| 29 April 2022 | Self-built house | Changsha, Hunan | 54/9 | No professional design, Illegal enlargement |
| 23 July 2023 | Gymnasium of No. 34 Middle School | Qiqihaer, Heilongjiang | 11/0 | Construction mistakes |
| Date | Time | Description |
|---|---|---|
| 28 April 2022 | 20:00 p.m. | On the second floor, the staff of the restaurant noticed that a concrete column on the eastern side, as well as the adjacent wall tiles, had become detached. The plaster on the wall had cracked, and the concrete at the base of the column had been crushed, with exposed and bent reinforcing bars. |
| 29 April 2022 | 10:15 a.m. | A supporting U-steel beam on the second floor (purchased by the owner in July 2019 to reinforce the column that had developed cracks) had undergone severe deformation, creating a gap of approximately 50 mm from the wall. |
| 29 April 2022 | 11:50 a.m. | The owner went out to purchase construction materials in preparation for further reinforcement. |
| 29 April 2022 | 12:19 p.m. | The exterior wall at the southeast corner, where the first and second floor ring beams meet, exhibited peeling plaster, exposed bricks, and outward bulging, signifying the onset of wall deformation. Neighbors and the village group leader present at the scene advised the owner to evacuate, but their attempts to persuade were unsuccessful. |
| 29 April 2022 | 12:21 p.m. | The eastern wall of the restaurant on the second floor made abnormal noises, and objects fell from the ceiling and the eastern exterior wall. The restaurant manager promptly urged two staff members and three diners to leave. |
| 29 April 2022 | 12:24 p.m. | The entire building collapsed in a sink-like manner, taking approximately 4 s. |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Tang, D.; Huang, M. Dilemmas and Solutions for Sustainability-Based Engineering Ethics: Lessons Learned from the Collapse of a Self-Built House in Changsha, Hunan, China. Buildings 2024 , 14 , 2581. https://doi.org/10.3390/buildings14082581
Tang D, Huang M. Dilemmas and Solutions for Sustainability-Based Engineering Ethics: Lessons Learned from the Collapse of a Self-Built House in Changsha, Hunan, China. Buildings . 2024; 14(8):2581. https://doi.org/10.3390/buildings14082581
Tang, Dina, and Minshui Huang. 2024. "Dilemmas and Solutions for Sustainability-Based Engineering Ethics: Lessons Learned from the Collapse of a Self-Built House in Changsha, Hunan, China" Buildings 14, no. 8: 2581. https://doi.org/10.3390/buildings14082581
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Ethical Issues in Research: Perceptions of Researchers, Research Ethics Board Members and Research Ethics Experts
- Published: 12 August 2022
- Volume 21 , pages 269–292, ( 2023 )
Cite this article

- Marie-Josée Drolet ORCID: orcid.org/0000-0001-8384-4193 1 ,
- Eugénie Rose-Derouin 2 ,
- Julie-Claude Leblanc 2 ,
- Mélanie Ruest 2 &
- Bryn Williams-Jones 3
33k Accesses
11 Citations
4 Altmetric
Explore all metrics
In the context of academic research, a diversity of ethical issues, conditioned by the different roles of members within these institutions, arise. Previous studies on this topic addressed mainly the perceptions of researchers. However, to our knowledge, no studies have explored the transversal ethical issues from a wider spectrum, including other members of academic institutions as the research ethics board (REB) members, and the research ethics experts. The present study used a descriptive phenomenological approach to document the ethical issues experienced by a heterogeneous group of Canadian researchers, REB members, and research ethics experts. Data collection involved socio-demographic questionnaires and individual semi-structured interviews. Following the triangulation of different perspectives (researchers, REB members and ethics experts), emerging ethical issues were synthesized in ten units of meaning: (1) research integrity, (2) conflicts of interest, (3) respect for research participants, (4) lack of supervision and power imbalances, (5) individualism and performance, (6) inadequate ethical guidance, (7) social injustices, (8) distributive injustices, (9) epistemic injustices, and (10) ethical distress. This study highlighted several problematic elements that can support the identification of future solutions to resolve transversal ethical issues in research that affect the heterogeneous members of the academic community.
Similar content being viewed by others

Ethical Research? Examining Knotty, Moment-to-Moment Challenges Throughout the Research Process

Approaching Research in a Prepared, Mindful and Ethical Manner
Conceptualising Ethical Issues in the Conduct of Research: Results from a Critical and Systematic Literature Review
Explore related subjects.
- Artificial Intelligence
- Medical Ethics
Avoid common mistakes on your manuscript.
Introduction
Research includes a set of activities in which researchers use various structured methods to contribute to the development of knowledge, whether this knowledge is theoretical, fundamental, or applied (Drolet & Ruest, accepted ). University research is carried out in a highly competitive environment that is characterized by ever-increasing demands (i.e., on time, productivity), insufficient access to research funds, and within a market economy that values productivity and speed often to the detriment of quality or rigour – this research context creates a perfect recipe for breaches in research ethics, like research misbehaviour or misconduct (i.e., conduct that is ethically questionable or unacceptable because it contravenes the accepted norms of responsible conduct of research or compromises the respect of core ethical values that are widely held by the research community) (Drolet & Girard, 2020 ; Sieber, 2004 ). Problematic ethics and integrity issues – e.g., conflicts of interest, falsification of data, non-respect of participants’ rights, and plagiarism, to name but a few – have the potential to both undermine the credibility of research and lead to negative consequences for many stakeholders, including researchers, research assistants and personnel, research participants, academic institutions, and society as a whole (Drolet & Girard, 2020 ). It is thus evident that the academic community should be able to identify these different ethical issues in order to evaluate the nature of the risks that they pose (and for whom), and then work towards their prevention or management (i.e., education, enhanced policies and procedures, risk mitigation strategies).
In this article, we define an “ethical issue” as any situation that may compromise, in whole or in part, the respect of at least one moral value (Swisher et al., 2005 ) that is considered socially legitimate and should thus be respected. In general, ethical issues occur at three key moments or stages of the research process: (1) research design (i.e., conception, project planning), (2) research conduct (i.e., data collection, data analysis) and (3) knowledge translation or communication (e.g., publications of results, conferences, press releases) (Drolet & Ruest, accepted ). According to Sieber ( 2004 ), ethical issues in research can be classified into five categories, related to: (a) communication with participants and the community, (b) acquisition and use of research data, (c) external influence on research, (d) risks and benefits of the research, and (e) selection and use of research theories and methods. Many of these issues are related to breaches of research ethics norms, misbehaviour or research misconduct. Bruhn et al., ( 2002 ) developed a typology of misbehaviour and misconduct in academia that can be used to judge the seriousness of different cases. This typology takes into consideration two axes of reflection: (a) the origin of the situation (i.e., is it the researcher’s own fault or due to the organizational context?), and (b) the scope and severity (i.e., is this the first instance or a recurrent behaviour? What is the nature of the situation? What are the consequences, for whom, for how many people, and for which organizations?).
A previous detailed review of the international literature on ethical issues in research revealed several interesting findings (Beauchemin et al., 2021 ). Indeed, the current literature is dominated by descriptive ethics, i.e., the sharing by researchers from various disciplines of the ethical issues they have personally experienced. While such anecdotal documentation is relevant, it is insufficient because it does not provide a global view of the situation. Among the reviewed literature, empirical studies were in the minority (Table 1 ) – only about one fifth of the sample (n = 19) presented empirical research findings on ethical issues in research. The first of these studies was conducted almost 50 years ago (Hunt et al., 1984 ), with the remainder conducted in the 1990s. Eight studies were conducted in the United States (n = 8), five in Canada (n = 5), three in England (n = 3), two in Sweden (n = 2) and one in Ghana (n = 1).
Further, the majority of studies in our sample (n = 12) collected the perceptions of a homogeneous group of participants, usually researchers (n = 14) and sometimes health professionals (n = 6). A minority of studies (n = 7) triangulated the perceptions of diverse research stakeholders (i.e., researchers and research participants, or students). To our knowledge, only one study has examined perceptions of ethical issues in research by research ethics board members (REB; Institutional Review Boards [IRB] in the USA), and none to date have documented the perceptions of research ethics experts. Finally, nine studies (n = 9) adopted a qualitative design, seven studies (n = 7) a quantitative design, and three (n = 3) a mixed-methods design.
More studies using empirical research methods are needed to better identify broader trends, to enrich discussions on the values that should govern responsible conduct of research in the academic community, and to evaluate the means by which these values can be supported in practice (Bahn, 2012 ; Beauchemin et al., 2021 ; Bruhn et al., 2002 ; Henderson et al., 2013 ; Resnik & Elliot, 2016; Sieber 2004 ). To this end, we conducted an empirical qualitative study to document the perceptions and experiences of a heterogeneous group of Canadian researchers, REB members, and research ethics experts, to answer the following broad question: What are the ethical issues in research?
Research Methods
Research design.
A qualitative research approach involving individual semi-structured interviews was used to systematically document ethical issues (De Poy & Gitlin, 2010 ; Hammell et al., 2000 ). Specifically, a descriptive phenomenological approach inspired by the philosophy of Husserl was used (Husserl, 1970 , 1999 ), as it is recommended for documenting the perceptions of ethical issues raised by various practices (Hunt & Carnavale, 2011 ).
Ethical considerations
The principal investigator obtained ethics approval for this project from the Research Ethics Board of the Université du Québec à Trois-Rivières (UQTR). All members of the research team signed a confidentiality agreement, and research participants signed the consent form after reading an information letter explaining the nature of the research project.
Sampling and recruitment
As indicated above, three types of participants were sought: (1) researchers from different academic disciplines conducting research (i.e., theoretical, fundamental or empirical) in Canadian universities; (2) REB members working in Canadian organizations responsible for the ethical review, oversight or regulation of research; and (3) research ethics experts, i.e., academics or ethicists who teach research ethics, conduct research in research ethics, or are scholars who have acquired a specialization in research ethics. To be included in the study, participants had to work in Canada, speak and understand English or French, and be willing to participate in the study. Following Thomas and Polio’s (2002) recommendation to recruit between six and twelve participants (for a homogeneous sample) to ensure data saturation, for our heterogeneous sample, we aimed to recruit approximately twelve participants in order to obtain data saturation. Having used this method several times in related projects in professional ethics, data saturation is usually achieved with 10 to 15 participants (Drolet & Goulet, 2018 ; Drolet & Girard, 2020 ; Drolet et al., 2020 ). From experience, larger samples only serve to increase the degree of data saturation, especially in heterogeneous samples (Drolet et al., 2017 , 2019 ; Drolet & Maclure, 2016 ).
Purposive sampling facilitated the identification of participants relevant to documenting the phenomenon in question (Fortin, 2010 ). To ensure a rich and most complete representation of perceptions, we sought participants with varied and complementary characteristics with regards to the social roles they occupy in research practice (Drolet & Girard, 2020 ). A triangulation of sources was used for the recruitment (Bogdan & Biklen, 2006 ). The websites of Canadian universities and Canadian health institution REBs, as well as those of major Canadian granting agencies (i.e., the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, and the Social Sciences and Humanities Research Council of Canada, Fonds de recherche du Quebec), were searched to identify individuals who might be interested in participating in the study. Further, people known by the research team for their knowledge and sensitivity to ethical issues in research were asked to participate. Research participants were also asked to suggest other individuals who met the study criteria.
Data Collection
Two tools were used for data collecton: (a) a socio-demographic questionnaire, and (b) a semi-structured individual interview guide. English and French versions of these two documents were used and made available, depending on participant preferences. In addition, although the interview guide contained the same questions, they were adapted to participants’ specific roles (i.e., researcher, REB member, research ethics expert). When contacted by email by the research assistant, participants were asked to confirm under which role they wished to participate (because some participants might have multiple, overlapping responsibilities) and they were sent the appropriate interview guide.
The interview guides each had two parts: an introduction and a section on ethical issues. The introduction consisted of general questions to put the participant at ease (i.e., “Tell me what a typical day at work is like for you”). The section on ethical issues was designed to capture the participant’s perceptions through questions such as: “Tell me three stories you have experienced at work that involve an ethical issue?” and “Do you feel that your organization is doing enough to address, manage, and resolve ethical issues in your work?”. Although some interviews were conducted in person, the majority were conducted by videoconference to promote accessibility and because of the COVID-19 pandemic. Interviews were digitally recorded so that the verbatim could be transcribed in full, and varied between 40 and 120 min in duration, with an average of 90 min. Research assistants conducted the interviews and transcribed the verbatim.
Data Analysis
The socio-demographic questionnaires were subjected to simple descriptive statistical analyses (i.e., means and totals), and the semi-structured interviews were subjected to qualitative analysis. The steps proposed by Giorgi ( 1997 ) for a Husserlian phenomenological reduction of the data were used. After collecting, recording, and transcribing the interviews, all verbatim were analyzed by at least two analysts: a research assistant (2nd author of this article) and the principal investigator (1st author) or a postdoctoral fellow (3rd author). The repeated reading of the verbatim allowed the first analyst to write a synopsis, i.e., an initial extraction of units of meaning. The second analyst then read the synopses, which were commented and improved if necessary. Agreement between analysts allowed the final drafting of the interview synopses, which were then analyzed by three analysts to generate and organize the units of meaning that emerged from the qualitative data.
Participants
Sixteen individuals (n = 16) participated in the study, of whom nine (9) identified as female and seven (7) as male (Table 2 ). Participants ranged in age from 22 to 72 years, with a mean age of 47.5 years. Participants had between one (1) and 26 years of experience in the research setting, with an average of 14.3 years of experience. Participants held a variety of roles, including: REB members (n = 11), researchers (n = 10), research ethics experts (n = 4), and research assistant (n = 1). As mentioned previously, seven (7) participants held more than one role, i.e., REB member, research ethics expert, and researcher. The majority (87.5%) of participants were working in Quebec, with the remaining working in other Canadian provinces. Although all participants considered themselves to be francophone, one quarter (n = 4) identified themselves as belonging to a cultural minority group.
With respect to their academic background, most participants (n = 9) had a PhD, three (3) had a post-doctorate, two (2) had a master’s degree, and two (2) had a bachelor’s degree. Participants came from a variety of disciplines: nine (9) had a specialty in the humanities or social sciences, four (4) in the health sciences and three (3) in the natural sciences. In terms of their knowledge of ethics, five (5) participants reported having taken one university course entirely dedicated to ethics, four (4) reported having taken several university courses entirely dedicated to ethics, three (3) had a university degree dedicated to ethics, while two (2) only had a few hours or days of training in ethics and two (2) reported having no knowledge of ethics.
- Ethical issues
As Fig. 1 illustrates, ten units of meaning emerge from the data analysis, namely: (1) research integrity, (2) conflicts of interest, (3) respect for research participants, (4) lack of supervision and power imbalances, (5) individualism and performance, (6) inadequate ethical guidance, (7) social injustices, (8) distributive injustices, (9) epistemic injustices, and (10) ethical distress. To illustrate the results, excerpts from verbatim interviews are presented in the following sub-sections. Most of the excerpts have been translated into English as the majority of interviews were conducted with French-speaking participants.
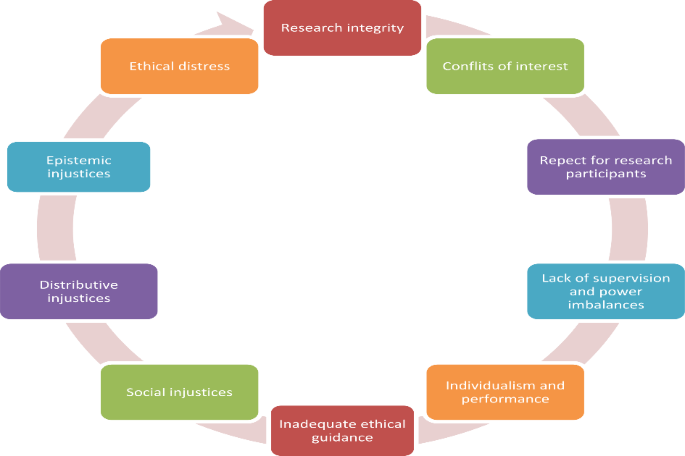
Ethical issues in research according to the participants
Research Integrity
The research environment is highly competitive and performance-based. Several participants, in particular researchers and research ethics experts, felt that this environment can lead both researchers and research teams to engage in unethical behaviour that reflects a lack of research integrity. For example, as some participants indicated, competition for grants and scientific publications is sometimes so intense that researchers falsify research results or plagiarize from colleagues to achieve their goals.
Some people will lie or exaggerate their research findings in order to get funding. Then, you see it afterwards, you realize: “ah well, it didn’t work, but they exaggerated what they found and what they did” (participant 14). Another problem in research is the identification of authors when there is a publication. Very often, there are authors who don’t even know what the publication is about and that their name is on it. (…) The time that it surprised me the most was just a few months ago when I saw someone I knew who applied for a teaching position. He got it I was super happy for him. Then I looked at his publications and … there was one that caught my attention much more than the others, because I was in it and I didn’t know what that publication was. I was the second author of a publication that I had never read (participant 14). I saw a colleague who had plagiarized another colleague. [When the colleague] found out about it, he complained. So, plagiarism is a serious [ethical breach]. I would also say that there is a certain amount of competition in the university faculties, especially for grants (…). There are people who want to win at all costs or get as much as possible. They are not necessarily going to consider their colleagues. They don’t have much of a collegial spirit (participant 10).
These examples of research misbehaviour or misconduct are sometimes due to or associated with situations of conflicts of interest, which may be poorly managed by certain researchers or research teams, as noted by many participants.
Conflict of interest
The actors and institutions involved in research have diverse interests, like all humans and institutions. As noted in Chap. 7 of the Canadian Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans (TCPS2, 2018),
“researchers and research students hold trust relationships, either directly or indirectly, with participants, research sponsors, institutions, their professional bodies and society. These trust relationships can be put at risk by conflicts of interest that may compromise independence, objectivity or ethical duties of loyalty. Although the potential for such conflicts has always existed, pressures on researchers (i.e., to delay or withhold dissemination of research outcomes or to use inappropriate recruitment strategies) heighten concerns that conflicts of interest may affect ethical behaviour” (p. 92).
The sources of these conflicts are varied and can include interpersonal conflicts, financial partnerships, third-party pressures, academic or economic interests, a researcher holding multiple roles within an institution, or any other incentive that may compromise a researcher’s independence, integrity, and neutrality (TCPS2, 2018). While it is not possible to eliminate all conflicts of interest, it is important to manage them properly and to avoid temptations to behave unethically.
Ethical temptations correspond to situations in which people are tempted to prioritize their own interests to the detriment of the ethical goods that should, in their own context, govern their actions (Swisher et al., 2005 ). In the case of researchers, this refers to situations that undermine independence, integrity, neutrality, or even the set of principles that govern research ethics (TCPS2, 2018) or the responsible conduct of research. According to study participants, these types of ethical issues frequently occur in research. Many participants, especially researchers and REB members, reported that conflicts of interest can arise when members of an organization make decisions to obtain large financial rewards or to increase their academic profile, often at the expense of the interests of members of their research team, research participants, or even the populations affected by their research.
A company that puts money into making its drug work wants its drug to work. So, homeopathy is a good example, because there are not really any consequences of homeopathy, there are not very many side effects, because there are no effects at all. So, it’s not dangerous, but it’s not a good treatment either. But some people will want to make it work. And that’s a big issue when you’re sitting at a table and there are eight researchers, and there are two or three who are like that, and then there are four others who are neutral, and I say to myself, this is not science. I think that this is a very big ethical issue (participant 14). There are also times in some research where there will be more links with pharmaceutical companies. Obviously, there are then large amounts of money that will be very interesting for the health-care institutions because they still receive money for clinical trials. They’re still getting some compensation because its time consuming for the people involved and all that. The pharmaceutical companies have money, so they will compensate, and that is sometimes interesting for the institutions, and since we are a bit caught up in this, in the sense that we have no choice but to accept it. (…) It may not be the best research in the world, there may be a lot of side effects due to the drugs, but it’s good to accept it, we’re going to be part of the clinical trial (participant 3). It is integrity, what we believe should be done or said. Often by the pressure of the environment, integrity is in tension with the pressures of the environment, so it takes resistance, it takes courage in research. (…) There were all the debates there about the problems of research that was funded and then the companies kept control over what was written. That was really troubling for a lot of researchers (participant 5).
Further, these situations sometimes have negative consequences for research participants as reported by some participants.
Respect for research participants
Many research projects, whether they are psychosocial or biomedical in nature, involve human participants. Relationships between the members of research teams and their research participants raise ethical issues that can be complex. Research projects must always be designed to respect the rights and interests of research participants, and not just those of researchers. However, participants in our study – i.e., REB members, researchers, and research ethics experts – noted that some research teams seem to put their own interests ahead of those of research participants. They also emphasized the importance of ensuring the respect, well-being, and safety of research participants. The ethical issues related to this unit of meaning are: respect for free, informed and ongoing consent of research participants; respect for and the well-being of participants; data protection and confidentiality; over-solicitation of participants; ownership of the data collected on participants; the sometimes high cost of scientific innovations and their accessibility; balance between the social benefits of research and the risks to participants (particularly in terms of safety); balance between collective well-being (development of knowledge) and the individual rights of participants; exploitation of participants; paternalism when working with populations in vulnerable situations; and the social acceptability of certain types of research. The following excerpts present some of these issues.
Where it disturbs me ethically is in the medical field – because it’s more in the medical field that we’re going to see this – when consent forms are presented to patients to solicit them as participants, and then [these forms] have an average of 40 pages. That annoys me. When they say that it has to be easy to understand and all that, adapted to the language, and then the hyper-technical language plus there are 40 pages to read, I don’t understand how you’re going to get informed consent after reading 40 pages. (…) For me, it doesn’t work. I read them to evaluate them and I have a certain level of education and experience in ethics, and there are times when I don’t understand anything (participant 2). There is a lot of pressure from researchers who want to recruit research participants (…). The idea that when you enter a health care institution, you become a potential research participant, when you say “yes to a research, you check yes to all research”, then everyone can ask you. I think that researchers really have this fantasy of saying to themselves: “as soon as people walk through the door of our institution, they become potential participants with whom we can communicate and get them involved in all projects”. There’s a kind of idea that, yes, it can be done, but it has to be somewhat supervised to avoid over-solicitation (…). Researchers are very interested in facilitating recruitment and making it more fluid, but perhaps to the detriment of confidentiality, privacy, and respect; sometimes that’s what it is, to think about what type of data you’re going to have in your bank of potential participants? Is it just name and phone number or are you getting into more sensitive information? (participant 9).
In addition, one participant reported that their university does not provide the resources required to respect the confidentiality of research participants.
The issue is as follows: researchers, of course, commit to protecting data with passwords and all that, but we realize that in practice, it is more difficult. It is not always as protected as one might think, because professor-researchers will run out of space. Will the universities make rooms available to researchers, places where they can store these things, especially when they have paper documentation, and is there indeed a guarantee of confidentiality? Some researchers have told me: “Listen; there are even filing cabinets in the corridors”. So, that certainly poses a concrete challenge. How do we go about challenging the administrative authorities? Tell them it’s all very well to have an ethics committee, but you have to help us, you also have to make sure that the necessary infrastructures are in place so that what we are proposing is really put into practice (participant 4).
If the relationships with research participants are likely to raise ethical issues, so too are the relationships with students, notably research assistants. On this topic, several participants discussed the lack of supervision or recognition offered to research assistants by researchers as well as the power imbalances between members of the research team.
Lack of Supervision and Power Imbalances
Many research teams are composed not only of researchers, but also of students who work as research assistants. The relationship between research assistants and other members of research teams can sometimes be problematic and raise ethical issues, particularly because of the inevitable power asymmetries. In the context of this study, several participants – including a research assistant, REB members, and researchers – discussed the lack of supervision or recognition of the work carried out by students, psychological pressure, and the more or less well-founded promises that are sometimes made to students. Participants also mentioned the exploitation of students by certain research teams, which manifest when students are inadequately paid, i.e., not reflective of the number of hours actually worked, not a fair wage, or even a wage at all.
[As a research assistant], it was more of a feeling of distress that I felt then because I didn’t know what to do. (…) I was supposed to get coaching or be supported, but I didn’t get anything in the end. It was like, “fix it by yourself”. (…) All research assistants were supposed to be supervised, but in practice they were not (participant 1). Very often, we have a master’s or doctoral student that we put on a subject and we consider that the project will be well done, while the student is learning. So, it happens that the student will do a lot of work and then we realize that the work is poorly done, and it is not necessarily the student’s fault. He wasn’t necessarily well supervised. There are directors who have 25 students, and they just don’t supervise them (participant 14). I think it’s really the power relationship. I thought to myself, how I saw my doctorate, the beginning of my research career, I really wanted to be in that laboratory, but they are the ones who are going to accept me or not, so what do I do to be accepted? I finally accept their conditions [which was to work for free]. If these are the conditions that are required to enter this lab, I want to go there. So, what do I do, well I accepted. It doesn’t make sense, but I tell myself that I’m still privileged, because I don’t have so many financial worries, one more reason to work for free, even though it doesn’t make sense (participant 1). In research, we have research assistants. (…). The fact of using people… so that’s it, you have to take into account where they are, respect them, but at the same time they have to show that they are there for the research. In English, we say “carry” or take care of people. With research assistants, this is often a problem that I have observed: for grant machines, the person is the last to be found there. Researchers, who will take, use student data, without giving them the recognition for it (participant 5). The problem at our university is that they reserve funding for Canadian students. The doctoral clientele in my field is mostly foreign students. So, our students are poorly funded. I saw one student end up in the shelter, in a situation of poverty. It ended very badly for him because he lacked financial resources. Once you get into that dynamic, it’s very hard to get out. I was made aware of it because the director at the time had taken him under her wing and wanted to try to find a way to get him out of it. So, most of my students didn’t get funded (participant 16). There I wrote “manipulation”, but it’s kind of all promises all the time. I, for example, was promised a lot of advancement, like when I got into the lab as a graduate student, it was said that I had an interest in [this particular area of research]. I think there are a lot of graduate students who must have gone through that, but it is like, “Well, your CV has to be really good, if you want to do a lot of things and big things. If you do this, if you do this research contract, the next year you could be the coordinator of this part of the lab and supervise this person, get more contracts, be paid more. Let’s say: you’ll be invited to go to this conference, this big event”. They were always dangling something, but you have to do that first to get there. But now, when you’ve done that, you have to do this business. It’s like a bit of manipulation, I think. That was very hard to know who is telling the truth and who is not (participant 1).
These ethical issues have significant negative consequences for students. Indeed, they sometimes find themselves at the mercy of researchers, for whom they work, struggling to be recognized and included as authors of an article, for example, or to receive the salary that they are due. For their part, researchers also sometimes find themselves trapped in research structures that can negatively affect their well-being. As many participants reported, researchers work in organizations that set very high productivity standards and in highly competitive contexts, all within a general culture characterized by individualism.
Individualism and performance
Participants, especially researchers, discussed the culture of individualism and performance that characterizes the academic environment. In glorifying excellence, some universities value performance and productivity, often at the expense of psychological well-being and work-life balance (i.e., work overload and burnout). Participants noted that there are ethical silences in their organizations on this issue, and that the culture of individualism and performance is not challenged for fear of retribution or simply to survive, i.e., to perform as expected. Participants felt that this culture can have a significant negative impact on the quality of the research conducted, as research teams try to maximize the quantity of their work (instead of quality) in a highly competitive context, which is then exacerbated by a lack of resources and support, and where everything must be done too quickly.
The work-life balance with the professional ethics related to work in a context where you have too much and you have to do a lot, it is difficult to balance all that and there is a lot of pressure to perform. If you don’t produce enough, that’s it; after that, you can’t get any more funds, so that puts pressure on you to do more and more and more (participant 3). There is a culture, I don’t know where it comes from, and that is extremely bureaucratic. If you dare to raise something, you’re going to have many, many problems. They’re going to make you understand it. So, I don’t talk. It is better: your life will be easier. I think there are times when you have to talk (…) because there are going to be irreparable consequences. (…) I’m not talking about a climate of terror, because that’s exaggerated, it’s not true, people are not afraid. But people close their office door and say nothing because it’s going to make their work impossible and they’re not going to lose their job, they’re not going to lose money, but researchers need time to be focused, so they close their office door and say nothing (participant 16).
Researchers must produce more and more, and they feel little support in terms of how to do such production, ethically, and how much exactly they are expected to produce. As this participant reports, the expectation is an unspoken rule: more is always better.
It’s sometimes the lack of a clear line on what the expectations are as a researcher, like, “ah, we don’t have any specific expectations, but produce, produce, produce, produce.” So, in that context, it’s hard to be able to put the line precisely: “have I done enough for my work?” (participant 3).
Inadequate ethical Guidance
While the productivity expectation is not clear, some participants – including researchers, research ethics experts, and REB members – also felt that the ethical expectations of some REBs were unclear. The issue of the inadequate ethical guidance of research includes the administrative mechanisms to ensure that research projects respect the principles of research ethics. According to those participants, the forms required for both researchers and REB members are increasingly long and numerous, and one participant noted that the standards to be met are sometimes outdated and disconnected from the reality of the field. Multicentre ethics review (by several REBs) was also critiqued by a participant as an inefficient method that encumbers the processes for reviewing research projects. Bureaucratization imposes an ever-increasing number of forms and ethics guidelines that actually hinder researchers’ ethical reflection on the issues at stake, leading the ethics review process to be perceived as purely bureaucratic in nature.
The ethical dimension and the ethical review of projects have become increasingly bureaucratized. (…) When I first started working (…) it was less bureaucratic, less strict then. I would say [there are now] tons of forms to fill out. Of course, we can’t do without it, it’s one of the ways of marking out ethics and ensuring that there are ethical considerations in research, but I wonder if it hasn’t become too bureaucratized, so that it’s become a kind of technical reflex to fill out these forms, and I don’t know if people really do ethical reflection as such anymore (participant 10). The fundamental structural issue, I would say, is the mismatch between the normative requirements and the real risks posed by the research, i.e., we have many, many requirements to meet; we have very long forms to fill out but the research projects we evaluate often pose few risks (participant 8). People [in vulnerable situations] were previously unable to participate because of overly strict research ethics rules that were to protect them, but in the end [these rules] did not protect them. There was a perverse effect, because in the end there was very little research done with these people and that’s why we have very few results, very little evidence [to support practices with these populations] so it didn’t improve the quality of services. (…) We all understand that we have to be careful with that, but when the research is not too risky, we say to ourselves that it would be good because for once a researcher who is interested in that population, because it is not a very popular population, it would be interesting to have results, but often we are blocked by the norms, and then we can’t accept [the project] (participant 2).
Moreover, as one participant noted, accessing ethics training can be a challenge.
There is no course on research ethics. […] Then, I find that it’s boring because you go through university and you come to do your research and you know how to do quantitative and qualitative research, but all the research ethics, where do you get this? I don’t really know (participant 13).
Yet, such training could provide relevant tools to resolve, to some extent, the ethical issues that commonly arise in research. That said, and as noted by many participants, many ethical issues in research are related to social injustices over which research actors have little influence.
Social Injustices
For many participants, notably researchers, the issues that concern social injustices are those related to power asymmetries, stigma, or issues of equity, diversity, and inclusion, i.e., social injustices related to people’s identities (Blais & Drolet, 2022 ). Participants reported experiencing or witnessing discrimination from peers, administration, or lab managers. Such oppression is sometimes cross-sectional and related to a person’s age, cultural background, gender or social status.
I have my African colleague who was quite successful when he arrived but had a backlash from colleagues in the department. I think it’s unconscious, nobody is overtly racist. But I have a young person right now who is the same, who has the same success, who got exactly the same early career award and I don’t see the same backlash. He’s just as happy with what he’s doing. It’s normal, they’re young and they have a lot of success starting out. So, I think there is discrimination. Is it because he is African? Is it because he is black? I think it’s on a subconscious level (participant 16).
Social injustices were experienced or reported by many participants, and included issues related to difficulties in obtaining grants or disseminating research results in one’s native language (i.e., even when there is official bilingualism) or being considered credible and fundable in research when one researcher is a woman.
If you do international research, there are things you can’t talk about (…). It is really a barrier to research to not be able to (…) address this question [i.e. the question of inequalities between men and women]. Women’s inequality is going to be addressed [but not within the country where the research takes place as if this inequality exists elsewhere but not here]. There are a lot of women working on inequality issues, doing work and it’s funny because I was talking to a young woman who works at Cairo University and she said to me: “Listen, I saw what you had written, you’re right. I’m willing to work on this but guarantee me a position at your university with a ticket to go”. So yes, there are still many barriers [for women in research] (participant 16).
Because of the varied contextual characteristics that intervene in their occurrence, these social injustices are also related to distributive injustices, as discussed by many participants.
Distributive Injustices
Although there are several views of distributive justice, a classical definition such as that of Aristotle ( 2012 ), describes distributive justice as consisting in distributing honours, wealth, and other social resources or benefits among the members of a community in proportion to their alleged merit. Justice, then, is about determining an equitable distribution of common goods. Contemporary theories of distributive justice are numerous and varied. Indeed, many authors (e.g., Fraser 2011 ; Mills, 2017 ; Sen, 2011 ; Young, 2011 ) have, since Rawls ( 1971 ), proposed different visions of how social burdens and benefits should be shared within a community to ensure equal respect, fairness, and distribution. In our study, what emerges from participants’ narratives is a definite concern for this type of justice. Women researchers, francophone researchers, early career researchers or researchers belonging to racialized groups all discussed inequities in the distribution of research grants and awards, and the extra work they need to do to somehow prove their worth. These inequities are related to how granting agencies determine which projects will be funded.
These situations make me work 2–3 times harder to prove myself and to show people in power that I have a place as a woman in research (participant 12). Number one: it’s conservative thinking. The older ones control what comes in. So, the younger people have to adapt or they don’t get funded (participant 14).
Whether it is discrimination against stigmatized or marginalized populations or interest in certain hot topics, granting agencies judge research projects according to criteria that are sometimes questionable, according to those participants. Faced with difficulties in obtaining funding for their projects, several strategies – some of which are unethical – are used by researchers in order to cope with these situations.
Sometimes there are subjects that everyone goes to, such as nanotechnology (…), artificial intelligence or (…) the therapeutic use of cannabis, which are very fashionable, and this is sometimes to the detriment of other research that is just as relevant, but which is (…), less sexy, less in the spirit of the time. (…) Sometimes this can lead to inequities in the funding of certain research sectors (participant 9). When we use our funds, we get them given to us, we pretty much say what we think we’re going to do with them, but things change… So, when these things change, sometimes it’s an ethical decision, but by force of circumstances I’m obliged to change the project a little bit (…). Is it ethical to make these changes or should I just let the money go because I couldn’t use it the way I said I would? (participant 3).
Moreover, these distributional injustices are not only linked to social injustices, but also epistemic injustices. Indeed, the way in which research honours and grants are distributed within the academic community depends on the epistemic authority of the researchers, which seems to vary notably according to their language of use, their age or their gender, but also to the research design used (inductive versus deductive), their decision to use (or not use) animals in research, or to conduct activist research.
Epistemic injustices
The philosopher Fricker ( 2007 ) conceptualized the notions of epistemic justice and injustice. Epistemic injustice refers to a form of social inequality that manifests itself in the access, recognition, and production of knowledge as well as the various forms of ignorance that arise (Godrie & Dos Santos, 2017 ). Addressing epistemic injustice necessitates acknowledging the iniquitous wrongs suffered by certain groups of socially stigmatized individuals who have been excluded from knowledge, thus limiting their abilities to interpret, understand, or be heard and account for their experiences. In this study, epistemic injustices were experienced or reported by some participants, notably those related to difficulties in obtaining grants or disseminating research results in one’s native language (i.e., even when there is official bilingualism) or being considered credible and fundable in research when a researcher is a woman or an early career researcher.
I have never sent a grant application to the federal government in English. I have always done it in French, even though I know that when you receive the review, you can see that reviewers didn’t understand anything because they are English-speaking. I didn’t want to get in the boat. It’s not my job to translate, because let’s be honest, I’m not as good in English as I am in French. So, I do them in my first language, which is the language I’m most used to. Then, technically at the administrative level, they are supposed to be able to do it, but they are not good in French. (…) Then, it’s a very big Canadian ethical issue, because basically there are technically two official languages, but Canada is not a bilingual country, it’s a country with two languages, either one or the other. (…) So I was not funded (participant 14).
Researchers who use inductive (or qualitative) methods observed that their projects are sometimes less well reviewed or understood, while research that adopts a hypothetical-deductive (or quantitative) or mixed methods design is better perceived, considered more credible and therefore more easily funded. Of course, regardless of whether a research project adopts an inductive, deductive or mixed-methods scientific design, or whether it deals with qualitative or quantitative data, it must respect a set of scientific criteria. A research project should achieve its objectives by using proven methods that, in the case of inductive research, are credible, reliable, and transferable or, in the case of deductive research, generalizable, objective, representative, and valid (Drolet & Ruest, accepted ). Participants discussing these issues noted that researchers who adopt a qualitative design or those who question the relevance of animal experimentation or are not militant have sometimes been unfairly devalued in their epistemic authority.
There is a mini war between quantitative versus qualitative methods, which I think is silly because science is a method. If you apply the method well, it doesn’t matter what the field is, it’s done well and it’s perfect ” (participant 14). There is also the issue of the place of animals in our lives, because for me, ethics is human ethics, but also animal ethics. Then, there is a great evolution in society on the role of the animal… with the new law that came out in Quebec on the fact that animals are sensitive beings. Then, with the rise of the vegan movement, [we must ask ourselves]: “Do animals still have a place in research?” That’s a big question and it also means that there are practices that need to evolve, but sometimes there’s a disconnection between what’s expected by research ethics boards versus what’s expected in the field (participant 15). In research today, we have more and more research that is militant from an ideological point of view. And so, we have researchers, because they defend values that seem important to them, we’ll talk for example about the fight for equality and social justice. They have pressure to defend a form of moral truth and have the impression that everyone thinks like them or should do so, because they are defending a moral truth. This is something that we see more and more, namely the lack of distance between ideology and science (participant 8).
The combination or intersectionality of these inequities, which seems to be characterized by a lack of ethical support and guidance, is experienced in the highly competitive and individualistic context of research; it provides therefore the perfect recipe for researchers to experience ethical distress.
Ethical distress
The concept of “ethical distress” refers to situations in which people know what they should do to act ethically, but encounter barriers, generally of an organizational or systemic nature, limiting their power to act according to their moral or ethical values (Drolet & Ruest, 2021 ; Jameton, 1984 ; Swisher et al., 2005 ). People then run the risk of finding themselves in a situation where they do not act as their ethical conscience dictates, which in the long term has the potential for exhaustion and distress. The examples reported by participants in this study point to the fact that researchers in particular may be experiencing significant ethical distress. This distress takes place in a context of extreme competition, constant injunctions to perform, and where administrative demands are increasingly numerous and complex to complete, while paradoxically, they lack the time to accomplish all their tasks and responsibilities. Added to these demands are a lack of resources (human, ethical, and financial), a lack of support and recognition, and interpersonal conflicts.
We are in an environment, an elite one, you are part of it, you know what it is: “publish or perish” is the motto. Grants, there is a high level of performance required, to do a lot, to publish, to supervise students, to supervise them well, so yes, it is clear that we are in an environment that is conducive to distress. (…). Overwork, definitely, can lead to distress and eventually to exhaustion. When you know that you should take the time to read the projects before sharing them, but you don’t have the time to do that because you have eight that came in the same day, and then you have others waiting… Then someone rings a bell and says: “ah but there, the protocol is a bit incomplete”. Oh yes, look at that, you’re right. You make up for it, but at the same time it’s a bit because we’re in a hurry, we don’t necessarily have the resources or are able to take the time to do things well from the start, we have to make up for it later. So yes, it can cause distress (participant 9). My organization wanted me to apply in English, and I said no, and everyone in the administration wanted me to apply in English, and I always said no. Some people said: “Listen, I give you the choice”, then some people said: “Listen, I agree with you, but if you’re not [submitting] in English, you won’t be funded”. Then the fact that I am young too, because very often they will look at the CV, they will not look at the project: “ah, his CV is not impressive, we will not finance him”. This is complete nonsense. The person is capable of doing the project, the project is fabulous: we fund the project. So, that happened, organizational barriers: that happened a lot. I was not eligible for Quebec research funds (…). I had big organizational barriers unfortunately (participant 14). At the time of my promotion, some colleagues were not happy with the type of research I was conducting. I learned – you learn this over time when you become friends with people after you enter the university – that someone was against me. He had another candidate in mind, and he was angry about the selection. I was under pressure for the first three years until my contract was renewed. I almost quit at one point, but another colleague told me, “No, stay, nothing will happen”. Nothing happened, but these issues kept me awake at night (participant 16).
This difficult context for many researchers affects not only the conduct of their own research, but also their participation in research. We faced this problem in our study, despite the use of multiple recruitment methods, including more than 200 emails – of which 191 were individual solicitations – sent to potential participants by the two research assistants. REB members and organizations overseeing or supporting research (n = 17) were also approached to see if some of their employees would consider participating. While it was relatively easy to recruit REB members and research ethics experts, our team received a high number of non-responses to emails (n = 175) and some refusals (n = 5), especially by researchers. The reasons given by those who replied were threefold: (a) fear of being easily identified should they take part in the research, (b) being overloaded and lacking time, and (c) the intrusive aspect of certain questions (i.e., “Have you experienced a burnout episode? If so, have you been followed up medically or psychologically?”). In light of these difficulties and concerns, some questions in the socio-demographic questionnaire were removed or modified. Talking about burnout in research remains a taboo for many researchers, which paradoxically can only contribute to the unresolved problem of unhealthy research environments.
Returning to the research question and objective
The question that prompted this research was: What are the ethical issues in research? The purpose of the study was to describe these issues from the perspective of researchers (from different disciplines), research ethics board (REB) members, and research ethics experts. The previous section provided a detailed portrait of the ethical issues experienced by different research stakeholders: these issues are numerous, diverse and were recounted by a range of stakeholders.
The results of the study are generally consistent with the literature. For example, as in our study, the literature discusses the lack of research integrity on the part of some researchers (Al-Hidabi et al., 2018 ; Swazey et al., 1993 ), the numerous conflicts of interest experienced in research (Williams-Jones et al., 2013 ), the issues of recruiting and obtaining the free and informed consent of research participants (Provencher et al., 2014 ; Keogh & Daly, 2009 ), the sometimes difficult relations between researchers and REBs (Drolet & Girard, 2020 ), the epistemological issues experienced in research (Drolet & Ruest, accepted; Sieber 2004 ), as well as the harmful academic context in which researchers evolve, insofar as this is linked to a culture of performance, an overload of work in a context of accountability (Berg & Seeber, 2016 ; FQPPU; 2019 ) that is conducive to ethical distress and even burnout.
If the results of the study are generally in line with those of previous publications on the subject, our findings also bring new elements to the discussion while complementing those already documented. In particular, our results highlight the role of systemic injustices – be they social, distributive or epistemic – within the environments in which research is carried out, at least in Canada. To summarize, the results of our study point to the fact that the relationships between researchers and research participants are likely still to raise worrying ethical issues, despite widely accepted research ethics norms and institutionalized review processes. Further, the context in which research is carried out is not only conducive to breaches of ethical norms and instances of misbehaviour or misconduct, but also likely to be significantly detrimental to the health and well-being of researchers, as well as research assistants. Another element that our research also highlighted is the instrumentalization and even exploitation of students and research assistants, which is another important and worrying social injustice given the inevitable power imbalances between students and researchers.
Moreover, in a context in which ethical issues are often discussed from a micro perspective, our study helps shed light on both the micro- and macro-level ethical dimensions of research (Bronfenbrenner, 1979 ; Glaser 1994 ). However, given that ethical issues in research are not only diverse, but also and above all complex, a broader perspective that encompasses the interplay between the micro and macro dimensions can enable a better understanding of these issues and thereby support the identification of the multiple factors that may be at their origin. Triangulating the perspectives of researchers with those of REB members and research ethics experts enabled us to bring these elements to light, and thus to step back from and critique the way that research is currently conducted. To this end, attention to socio-political elements such as the performance culture in academia or how research funds are distributed, and according to what explicit and implicit criteria, can contribute to identifying the sources of the ethical issues described above.
Contemporary culture characterized by the social acceleration
The German sociologist and philosopher Rosa (2010) argues that late modernity – that is, the period between the 1980s and today – is characterized by a phenomenon of social acceleration that causes various forms of alienation in our relationship to time, space, actions, things, others and ourselves. Rosa distinguishes three types of acceleration: technical acceleration , the acceleration of social changes and the acceleration of the rhythm of life . According to Rosa, social acceleration is the main problem of late modernity, in that the invisible social norm of doing more and faster to supposedly save time operates unchallenged at all levels of individual and collective life, as well as organizational and social life. Although we all, researchers and non-researchers alike, perceive this unspoken pressure to be ever more productive, the process of social acceleration as a new invisible social norm is our blind spot, a kind of tyrant over which we have little control. This conceptualization of the contemporary culture can help us to understand the context in which research is conducted (like other professional practices). To this end, Berg & Seeber ( 2016 ) invite faculty researchers to slow down in order to better reflect and, in the process, take care of their health and their relationships with their colleagues and students. Many women professors encourage their fellow researchers, especially young women researchers, to learn to “say No” in order to protect their mental and physical health and to remain in their academic careers (Allaire & Descheneux, 2022 ). These authors also remind us of the relevance of Kahneman’s ( 2012 ) work which demonstrates that it takes time to think analytically, thoroughly, and logically. Conversely, thinking quickly exposes humans to cognitive and implicit biases that then lead to errors in thinking (e.g., in the analysis of one’s own research data or in the evaluation of grant applications or student curriculum vitae). The phenomenon of social acceleration, which pushes the researcher to think faster and faster, is likely to lead to unethical bad science that can potentially harm humankind. In sum, Rosa’s invitation to contemporary critical theorists to seriously consider the problem of social acceleration is particularly insightful to better understand the ethical issues of research. It provides a lens through which to view the toxic context in which research is conducted today, and one that was shared by the participants in our study.
Clark & Sousa ( 2022 ) note, it is important that other criteria than the volume of researchers’ contributions be valued in research, notably quality. Ultimately, it is the value of the knowledge produced and its influence on the concrete lives of humans and other living beings that matters, not the quantity of publications. An interesting articulation of this view in research governance is seen in a change in practice by Australia’s national health research funder: they now restrict researchers to listing on their curriculum vitae only the top ten publications from the past ten years (rather than all of their publications), in order to evaluate the quality of contributions rather than their quantity. To create environments conducive to the development of quality research, it is important to challenge the phenomenon of social acceleration, which insidiously imposes a quantitative normativity that is both alienating and detrimental to the quality and ethical conduct of research. Based on our experience, we observe that the social norm of acceleration actively disfavours the conduct of empirical research on ethics in research. The fact is that researchers are so busy that it is almost impossible for them to find time to participate in such studies. Further, operating in highly competitive environments, while trying to respect the values and ethical principles of research, creates ethical paradoxes for members of the research community. According to Malherbe ( 1999 ), an ethical paradox is a situation where an individual is confronted by contradictory injunctions (i.e., do more, faster, and better). And eventually, ethical paradoxes lead individuals to situations of distress and burnout, or even to ethical failures (i.e., misbehaviour or misconduct) in the face of the impossibility of responding to contradictory injunctions.
Strengths and Limitations of the study
The triangulation of perceptions and experiences of different actors involved in research is a strength of our study. While there are many studies on the experiences of researchers, rarely are members of REBs and experts in research ethics given the space to discuss their views of what are ethical issues. Giving each of these stakeholders a voice and comparing their different points of view helped shed a different and complementary light on the ethical issues that occur in research. That said, it would have been helpful to also give more space to issues experienced by students or research assistants, as the relationships between researchers and research assistants are at times very worrying, as noted by a participant, and much work still needs to be done to eliminate the exploitative situations that seem to prevail in certain research settings. In addition, no Indigenous or gender diverse researchers participated in the study. Given the ethical issues and systemic injustices that many people from these groups face in Canada (Drolet & Goulet, 2018 ; Nicole & Drolet, in press ), research that gives voice to these researchers would be relevant and contribute to knowledge development, and hopefully also to change in research culture.
Further, although most of the ethical issues discussed in this article may be transferable to the realities experienced by researchers in other countries, the epistemic injustice reported by Francophone researchers who persist in doing research in French in Canada – which is an officially bilingual country but in practice is predominantly English – is likely specific to the Canadian reality. In addition, and as mentioned above, recruitment proved exceedingly difficult, particularly amongst researchers. Despite this difficulty, we obtained data saturation for all but two themes – i.e., exploitation of students and ethical issues of research that uses animals. It follows that further empirical research is needed to improve our understanding of these specific issues, as they may diverge to some extent from those documented here and will likely vary across countries and academic research contexts.
Conclusions
This study, which gave voice to researchers, REB members, and ethics experts, reveals that the ethical issues in research are related to several problematic elements as power imbalances and authority relations. Researchers and research assistants are subject to external pressures that give rise to integrity issues, among others ethical issues. Moreover, the current context of social acceleration influences the definition of the performance indicators valued in academic institutions and has led their members to face several ethical issues, including social, distributive, and epistemic injustices, at different steps of the research process. In this study, ten categories of ethical issues were identified, described and illustrated: (1) research integrity, (2) conflicts of interest, (3) respect for research participants, (4) lack of supervision and power imbalances, (5) individualism and performance, (6) inadequate ethical guidance, (7) social injustices, (8) distributive injustices, (9) epistemic injustices, and (10) ethical distress. The triangulation of the perspectives of different members (i.e., researchers from different disciplines, REB members, research ethics experts, and one research assistant) involved in the research process made it possible to lift the veil on some of these ethical issues. Further, it enabled the identification of additional ethical issues, especially systemic injustices experienced in research. To our knowledge, this is the first time that these injustices (social, distributive, and epistemic injustices) have been clearly identified.
Finally, this study brought to the fore several problematic elements that are important to address if the research community is to develop and implement the solutions needed to resolve the diverse and transversal ethical issues that arise in research institutions. A good starting point is the rejection of the corollary norms of “publish or perish” and “do more, faster, and better” and their replacement with “publish quality instead of quantity”, which necessarily entails “do less, slower, and better”. It is also important to pay more attention to the systemic injustices within which researchers work, because these have the potential to significantly harm the academic careers of many researchers, including women researchers, early career researchers, and those belonging to racialized groups as well as the health, well-being, and respect of students and research participants.
Al-Hidabi, Abdulmalek, M. D., & The, P. L. (2018). Multiple Publications: The Main Reason for the Retraction of Papers in Computer Science. In K. Arai, S. Kapoor, & R. Bhatia (eds), Future of Information and Communication Conference (FICC): Advances in Information and Communication, Advances in Intelligent Systems and Computing (AISC), Springer, vol. 886, pp. 511–526
Allaire, S., & Deschenaux, F. (2022). Récits de professeurs d’université à mi-carrière. Si c’était à refaire… . Presses de l’Université du Québec
Aristotle (2012). Aristotle’s Nicomachean Ethics . Chicago: The University of Chicago Press
Google Scholar
Bahn, S. (2012). Keeping Academic Field Researchers Safe: Ethical Safeguards. Journal of Academic Ethics , 10 , 83–91. https://doi.org/10.1007/s10805-012-9159-2
Article Google Scholar
Balk, D. E. (1995). Bereavement Research Using Control Groups: Ethical Obligations and Questions. Death Studies , 19 , 123–138
Beauchemin, É., Côté, L. P., Drolet, M. J., & Williams-Jones, B. (2021). Conceptualizing Ethical Issues in the Conduct of Research: Results from a Critical and Systematic Literature Review. Journal of Academic Ethics , Early Online. https://doi.org/10.1007/s10805-021-09411-7
Berg, M., & Seeber, B. K. (2016). The Slow Professor . University of Toronto Press
Birchley, G., Huxtable, R., Murtagh, M., Meulen, R. T., Flach, P., & Gooberman-Hill, R. (2017). Smart homes, private homes? An empirical study of technology researchers’ perceptions of ethical issues in developing smart-home health technologies. BMC Medical Ethics , 18 (23), 1–13. https://doi.org/10.1186/s12910-017-0183-z
Blais, J., & Drolet, M. J. (2022). Les injustices sociales vécues en camp de réfugiés: les comprendre pour mieux intervenir auprès de personnes ayant séjourné dans un camp de réfugiés. Recueil annuel belge d’ergothérapie , 14, 37–48
Bogdan, R. C., & Biklen, S. K. (2006). Qualitative research in education: An introduction to theory and methods . Allyn & Bacon
Bouffard, C. (2000). Le développement des pratiques de la génétique médicale et la construction des normes bioéthiques. Anthropologie et Sociétés , 24 (2), 73–90. https://doi.org/10.7202/015650ar
Bronfenbrenner, U. (1979). The Ecology of Human development. Experiments by nature and design . Harvard University Press
Bruhn, J. G., Zajac, G., Al-Kazemi, A. A., & Prescott, L. D. (2002). Moral positions and academic conduct: Parameters of tolerance for ethics failure. Journal of Higher Education , 73 (4), 461–493. https://doi.org/10.1353/jhe.2002.0033
Clark, A., & Sousa (2022). It’s time to end Canada’s obsession with research quantity. University Affairs/Affaires universitaires , February 14th. https://www.universityaffairs.ca/career-advice/effective-successfull-happy-academic/its-time-to-end-canadas-obsession-with-research-quantity/?utm_source=University+Affairs+e-newsletter&utm_campaign=276a847f 70-EMAIL_CAMPAIGN_2022_02_16&utm_medium=email&utm_term=0_314bc2ee29-276a847f70-425259989
Colnerud, G. (2015). Ethical dilemmas in research in relation to ethical review: An empirical study. Research Ethics , 10 (4), 238–253. DOI: https://doi.org/10.1177/1747016114552339
Davison, J. (2004). Dilemmas in Research: Issues of Vulnerability and Disempowerment for the Social Workers/Researcher. Journal of Social Work Practice , 18 (3), 379–393. https://doi.org/10.1080/0265053042000314447
DePoy, E., & Gitlin, L. N. (2010). Introduction to Research . St. Louis: Elsevier Mosby
Drolet, M. J., & Goulet, M. (2018). Travailler avec des patients autochtones du Canada ? Perceptions d’ergothérapeutes du Québec des enjeux éthiques de cette pratique. Recueil annuel belge francophone d’ergothérapie , 10 , 25–56
Drolet, M. J., & Girard, K. (2020). Les enjeux éthiques de la recherche en ergothérapie: un portrait préoccupant. Revue canadienne de bioéthique , 3 (3), 21–40. https://doi.org/10.7202/1073779ar
Drolet, M. J., Girard, K., & Gaudet, R. (2020). Les enjeux éthiques de l’enseignement en ergothérapie: des injustices au sein des départements universitaires. Revue canadienne de bioéthique , 3 (1), 22–36. https://www.erudit.org/fr/revues/bioethics/2020-v3-n1-bioethics05237/1068761ar/
Drolet, M. J., & Maclure, J. (2016). Les enjeux éthiques de la pratique de l’ergothérapie: perceptions d’ergothérapeutes. Revue Approches inductives , 3 (2), 166–196
Drolet, M. J., Pinard, C., & Gaudet, R. (2017). Les enjeux éthiques de la pratique privée: des ergothérapeutes du Québec lancent un cri d’alarme. Ethica – Revue interdisciplinaire de recherche en éthique , 21 (2), 173–209
Drolet, M. J., & Ruest, M. (2021). De l’éthique à l’ergothérapie: un cadre théorique et une méthode pour soutenir la pratique professionnelle . Québec: Presses de l’Université du Québec
Book Google Scholar
Drolet, M. J., & Ruest, M. (accepted). Quels sont les enjeux éthiques soulevés par la recherche scientifique? In M. Lalancette & J. Luckerhoff (dir). Initiation au travail intellectuel et à la recherche . Québec: Presses de l’Université du Québec, 18 p
Drolet, M. J., Sauvageau, A., Baril, N., & Gaudet, R. (2019). Les enjeux éthiques de la formation clinique en ergothérapie. Revue Approches inductives , 6 (1), 148–179. https://www.erudit.org/fr/revues/approchesind/2019-v6-n1-approchesind04618/1060048ar/
Fédération québécoise des professeures et des professeurs d’université (FQPPU). (2019). Enquête nationale sur la surcharge administrative du corps professoral universitaire québécois. Principaux résultats et pistes d’action . Montréal: FQPPU
Fortin, M. H. (2010). Fondements et étapes du processus de recherche. Méthodes quantitatives et qualitatives . Montréal, QC: Chenelière éducation
Fraser, D. M. (1997). Ethical dilemmas and practical problems for the practitioner researcher. Educational Action Research , 5 (1), 161–171
Fraser, N. (2011). Qu’est-ce que la justice sociale? Reconnaissance et redistribution . La Découverte
Fricker, M. (2007). Epistemic Injustice: Power and the Ethics of Knowing . Oxford University Press
Giorgi, A. (1997). De la méthode phénoménologique utilisée comme mode de recherche qualitative en sciences humaines: théories, pratique et évaluation. In J. Poupart, L. H. Groulx, J. P. Deslauriers, et al. (Eds.), La recherche qualitative: enjeux épistémologiques et méthodologiques (pp. 341–364). Boucherville, QC: Gaëtan Morin
Giorgini, V., Mecca, J. T., Gibson, C., Medeiros, K., Mumford, M. D., Connelly, S., & Devenport, L. D. (2016). Researcher Perceptions of Ethical Guidelines and Codes of Conduct. Accountability in Research , 22 (3), 123–138. https://doi.org/10.1080/08989621.2014.955607
Glaser, J. W. (1994). Three realms of ethics: Individual, institutional, societal. Theoretical model and case studies . Kansas Cuty, Sheed & Ward
Godrie, B., & Dos Santos, M. (2017). Présentation: inégalités sociales, production des savoirs et de l’ignorance. Sociologie et sociétés , 49 (1), 7. https://doi.org/10.7202/1042804ar
Hammell, K. W., Carpenter, C., & Dyck, I. (2000). Using Qualitative Research: A Practical Introduction for Occupational and Physical Therapists . Edinburgh: Churchill Livingstone
Henderson, M., Johnson, N. F., & Auld, G. (2013). Silences of ethical practice: dilemmas for researchers using social media. Educational Research and Evaluation , 19 (6), 546–560. https://doi.org/10.1080/13803611.2013.805656
Husserl, E. (1970). The crisis of European sciences and transcendental phenomenology . Evanston, IL: Northwestern University Press
Husserl, E. (1999). The train of thoughts in the lectures. In E. C. Polifroni, & M. Welch (Eds.), Perspectives on Philosophy of Science in Nursing . Philadelphia, PA: Lippincott. 247 – 62. 43
Hunt, S. D., Chonko, L. B., & Wilcox, J. B. (1984). Ethical problems of marketing researchers. Journal of Marketing Research , 21 , 309–324
Hunt, M. R., & Carnevale, F. A. (2011). Moral experience: A framework for bioethics research. Journal of Medical Ethics , 37 (11), 658–662. https://doi.org/10.1136/jme.2010.039008
Jameton, A. (1984). Nursing practice: The ethical issues . Englewood Cliffs, Prentice-Hall
Jarvis, K. (2017). Dilemmas in International Research and the Value of Practical Wisdom. Developing World Bioethics , 17 (1), 50–58. DOI: https://doi.org/10.1111/dewb.12121
Kahneman, D. (2012). Système 1, système 2: les deux vitesses de la pensée . Paris: Flammarion
Keogh, B., & Daly, L. (2009). The ethics of conducting research with mental health service users. British Journal of Nursing , 18 (5), 277–281. https://doi.org/10.12968/bjon.2009.18.5.40539
Lierville, A. L., Grou, C., & Pelletier, J. F. (2015). Enjeux éthiques potentiels liés aux partenariats patients en psychiatrie: État de situation à l’Institut universitaire en santé mentale de Montréal. Santé mentale au Québec , 40 (1), 119–134
Lynöe, N., Sandlund, M., & Jacobsson, L. (1999). Research ethics committees: A comparative study of assessment of ethical dilemmas. Scandinavian Journal of Public Health , 27 (2), 152–159
Malherbe, J. F. (1999). Compromis, dilemmes et paradoxes en éthique clinique . Anjou: Éditions Fides
McGinn, R. (2013). Discernment and denial: Nanotechnology researchers’ recognition of ethical responsibilities related to their work. NanoEthics , 7 , 93–105. https://doi.org/10.1007/s11569-013-0174-6
Mills, C. W. (2017). Black Rights / White rongs. The Critique of Racial Liberalism . Oxford University Press
Miyazaki, A. D., & Taylor, K. A. (2008). Researcher interaction biases and business ethics research: Respondent reactions to researcher characteristics. Journal of Business Ethics , 81 (4), 779–795. DOI https://doi.org/10.1007/s10551-007-9547-5
Mondain, N., & Bologo, E. (2009). L’intentionnalité du chercheur dans ses pratiques de production des connaissances: les enjeux soulevés par la construction des données en démographie et santé en Afrique. Cahiers de recherche sociologique , 48 , 175–204. https://doi.org/10.7202/039772ar
Nicole, M., & Drolet, M. J. (in press). Fitting transphobia and cisgenderism in occupational therapy, Occupational Therapy Now
Pope, K. S., & Vetter, V. A. (1992). Ethical dilemmas encountered by members of the American Psychological Association: A national survey. The American Psychologist , 47 (3), 397–411
Provencher, V., Mortenson, W. B., Tanguay-Garneau, L., Bélanger, K., & Dagenais, M. (2014). Challenges and strategies pertaining to recruitment and retention of frail elderly in research studies: A systematic review. Archives of Gerontology and Geriatrics , 59 (1), 18–24. https://doi.org/10.1016/j.archger.2014.03.006
Rawls, J. (1971). A Theory of Justice . Harvard University Press
Resnik, D. B., & Elliott, K. C. (2016). The Ethical Challenges of Socially Responsible Science. Accountability in Research , 23 (1), 31–46. https://doi.org/10.1080/08989621.2014.1002608
Rosa, H. (2010). Accélération et aliénation. Vers une théorie critique de la modernité tardive . Paris, Découverte
Sen, A. K. (2011). The Idea of Justice . The Belknap Press of Harvard University Press
Sen, A. K. (1995). Inegality Reexaminated . Oxford University Press
Sieber, J. E. (2004). Empirical Research on Research Ethics. Ethics & Behavior , 14 (4), 397–412. https://doi.org/10.1207/s15327019eb1404_9
Sigmon, S. T. (1995). Ethical practices and beliefs of psychopathology researchers. Ethics & Behavior , 5 (4), 295–309
Swazey, J. P., Anderson, M. S., & Lewis, K. S. (1993). Ethical Problems in Academic Research. American Scientist , 81 (6), 542–553
Swisher, L. L., Arsalanian, L. E., & Davis, C. M. (2005). The realm-individual-process-situation (RIPS) model of ethical decision-making. HPA Resource , 5 (3), 3–8. https://www-s3-live.kent.edu/s3fs-root/s3fs-public/file/RIPS_DecisionMaking_0.pdf
Tri-Council Policy Statement (TCPS2) (2018). Ethical Conduct for Research Involving Humans . Government of Canada, Secretariat on Responsible Conduct of Research. https://ethics.gc.ca/eng/documents/tcps2-2018-en-interactive-final.pdf
Thomas, S. P., & Pollio, H. R. (2002). Listening to Patients: A Phenomenological Approach to Nursing Research and Practice . New York: Springer Publishing Company
Wiegand, D. L., & Funk, M. (2012). Consequences of clinical situations that cause critical care nurses to experience moral distress. Nursing Ethics , 19 (4), 479–487. DOI https://doi.org/10.1177/0969733011429342
Williams-Jones, B., Potvin, M. J., Mathieu, G., & Smith, E. (2013). Barriers to research on research ethics review and conflicts of interest. IRB: Ethics & Human Research , 35 (5), 14–20
Young, I. M. (2011). Justice and the Politics of difference . Princeton University Press
Download references
Acknowledgements
The team warmly thanks the participants who took part in the research and who made this study possible. Marie-Josée Drolet thanks the five research assistants who participated in the data collection and analysis: Julie-Claude Leblanc, Élie Beauchemin, Pénéloppe Bernier, Louis-Pierre Côté, and Eugénie Rose-Derouin, all students at the Université du Québec à Trois-Rivières (UQTR), two of whom were active in the writing of this article. MJ Drolet and Bryn Williams-Jones also acknowledge the financial contribution of the Social Sciences and Humanities Research Council of Canada (SSHRC), which supported this research through a grant. We would also like to thank the reviewers of this article who helped us improve it, especially by clarifying and refining our ideas.
Author information
Authors and affiliations.
Department of Occupational Therapy (OT), Université du Québec à Trois-Rivières (UQTR), Trois-Rivières (Québec), Canada
Marie-Josée Drolet
Bachelor OT program, Université du Québec à Trois-Rivières (UQTR), Trois-Rivières (Québec), Canada
Eugénie Rose-Derouin, Julie-Claude Leblanc & Mélanie Ruest
Department of Social and Preventive Medicine, School of Public Health, Université de Montréal, Montréal (Québec), Canada
Bryn Williams-Jones
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marie-Josée Drolet .
Ethics declarations
Competing interests and funding.
As noted in the Acknowledgements, this research was supported financially by the Social Sciences and Humanities Research Council of Canada (SSHRC).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Drolet, MJ., Rose-Derouin, E., Leblanc, JC. et al. Ethical Issues in Research: Perceptions of Researchers, Research Ethics Board Members and Research Ethics Experts. J Acad Ethics 21 , 269–292 (2023). https://doi.org/10.1007/s10805-022-09455-3
Download citation
Received : 24 March 2022
Revised : 13 July 2022
Accepted : 13 July 2022
Published : 12 August 2022
Issue Date : June 2023
DOI : https://doi.org/10.1007/s10805-022-09455-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Researchers
- Research Ethics Board Members
- Research Ethics experts
- Find a journal
- Publish with us
- Track your research
- Clinical trials and evidence

Khunatorn - stock.adobe.com
Ethical Guidelines, Emerging Regulations in Octopus Research
Understanding octopus research guidelines is essential for ethical healthcare progress, ensuring breakthroughs align with moral standards and prioritize animal welfare..
- Alivia Kaylor, MSc
With their unique biological features, octopuses have become valuable subjects in medical research. Their extraordinary abilities, such as camouflage, regenerative capabilities, and highly developed nervous systems, make them captivating candidates for studies that could lead to innovative healthcare technology and medical research breakthroughs.
However, using octopuses as an animal model in research raises ethical concerns and regulatory challenges that must be addressed.
Ethical Oversight and Regulatory Framework
Ethical and regulatory oversight is crucial in the United States, where the exact number of octopuses used in biomedical research is not readily available. Research institutions must adhere to guidelines set forth by esteemed agencies like the National Institutes of Health (NIH) and the US Department of Agriculture (USDA). Institutional Animal Care and Use Committees (IACUCs) are also pivotal in reviewing and approving animal research protocols, ensuring they meet ethical standards and comply with applicable regulations.
Octopuses in the Laboratory
One area of research involving octopuses focuses on their unique ability to match their skin's color, pattern, and texture to their surroundings. This research, led by Roger Hanlon, PhD, a scientist at the Marine Biological Laboratory in Woods Hole, Massachusetts, revealed that the skins of cuttlefish and squid are full of light-detecting molecules, also known as opsins. These opsins are the same as those found in the animals’ retinas, suggesting they can perceive light through their skin. Research later confirmed that opsins are present in octopus skin.
Although these studies offer insights into biomimicry for military applications and medical devices, octopuses may not be the ideal animal model due to their high intelligence. Unlike rodents, octopuses are not as cooperative in controlled settings, leading to difficulties in certain types of studies.
The octopus surpasses the scope of [Hanlon’s] study. When placed in a tank, its immediate instinct is to thoroughly explore its surroundings, followed by attempts to break free, elucidated Amy Hancock-Ronemus, DVM, a former veterinarian at the University of Chicago’s Marine Biological Laboratory. Their focus isn't necessarily fixated on conforming to the tank's bottom, as their intelligence likely informs them that such conformity is unnecessary.
According to Hancock-Ronemus, the Marine Biological Laboratory’s policy is that all research animals are to be treated humanely. “Any lab animal veterinarian will tell you we need to give animals the benefit of the doubt,” she said to the American Veterinary Medical Association (AVMA). “We know any animal can feel stress and distress, and there’s really no good argument for not giving them the most humane care we know of.”
The Cost of Research Models
Octopuses, being more complex organisms, present challenges in terms of cost and maintenance compared to traditional laboratory animals like rodents. Rodents like rats have been widely used in research due to their availability, ease of handling, and lower costs.
Meanwhile, octopuses require specific environmental conditions and are generally more expensive to acquire and maintain. Researchers often choose models based on the relevance to their study, ethical considerations, and budget constraints.
Challenges in Aquarium Settings
Breeding octopuses in captivity is notoriously tricky, leading to most research subjects and aquarium displays being wild-caught. The challenges include creating modified tanks without internal vents or openings and providing secure lids to prevent escapes. Health issues, such as parasitic and bacterial infections, are common in captive octopuses, and addressing these concerns adds another layer of complexity to their care.
Octopuses, known for their high intelligence, require frequent mental stimulation in captivity. According to the AVMA, aquarium staff at Shedd Aquarium engage octopuses in training sessions to monitor their behavior and health. The staff noted that each octopus exhibits unique preferences and personalities, showcasing the need for specialized care and attention in research settings.
Each octopus has its own food preferences or favorite item or toy incorporated into the enrichment activities, as outlined by Eve Barrs, a former aquarist at Shedd Aquarium in Chicago. One octopus liked ice cube trays, while another was inseparable from a whiffle ball.
"He always kept it near, nestled in his tentacle," she reminisced. "He would bring it along during feedings and carefully carry it back to his den afterward."
Biomedical Breakthroughs from Octopus Research
Despite these mounting challenges, octopuses have contributed significantly to various biomedical studies.
Camouflage and Adaptive Coloration
Octopuses are masters of camouflage and can change the color and texture of their skin to blend into their surroundings. Researchers have studied the mechanisms behind this ability to develop a deception technology platform that is used in various fields, such as the military, medicine, robotics, and sustainable energy.
Regenerative Abilities
Octopuses have impressive regenerative abilities and can regrow arms that have been injured or amputated. Scientists are interested in understanding this regenerative capability's molecular and cellular processes, as it may provide insights into human regenerative medicine.
Neuroscience and Intelligence
Octopuses have highly developed nervous systems and complex behaviors. Studying their brains and nervous systems can provide insights into neurobiology and potentially inspire advancements in artificial intelligence .
Sucker Function
The suckers on an octopus's arms have a remarkable ability to manipulate objects with great dexterity. Researchers have examined the structure and function of these suckers to develop soft robotics and prosthetic limbs with improved gripping capabilities.
Venom Research
Octopus species possess venom that they use for predation or defense. Scientists have investigated the chemical composition of octopus venom for potential medical applications. For example, a team of Spanish and Australian researchers are studying the tumor-fighting properties of a group of synthetically produced venom compounds from various marine animals.
"The octopus peptide stops the proliferation of BRAF-mutated melanoma," said Maria Ikonomopoulousaid, PhD, the Institute for Molecular Bioscience at the University of Queensland, to Newsweek . "In addition, it is safe to be used at high doses; it is not toxic. Therefore, in combination with other FDA-approved melanoma drugs/management, treatments could potentially achieve better and safer patient outcomes."
While these studies have provided valuable insights and potential applications, the field of biomimicry, where nature's designs and processes inspire human innovation, is still ongoing, and many breakthroughs are in the earliest stages of development.
Recent Developments in Regulatory Oversight
In the US, cephalopods have been excluded from certain regulations covering laboratory animals due to their invertebrate status. However, recent initiatives by the NIH propose guidelines for the care and use of cephalopods in research. This marks a significant step toward ensuring ethical treatment and oversight, requiring researchers to obtain approval from IACUCs. The proposed guidance addresses factors such as justification for using cephalopods, sedation and anesthesia, and the impact of experimental procedures on the animals' well-being.
The Physicians Committee , alongside researchers, advocates, and Congress , has played a pivotal role in urging regulatory bodies to establish better protections for cephalopods used in research. The efforts to amend the definition of "animal" in the Public Health Service Policy on Humane Care and Use of Laboratory Animals (PHS Policy) to include cephalopods have gained momentum. While recently proposed guidance by the NIH is a positive step, ongoing advocacy work emphasizes the need for continuous efforts to ensure the humane treatment of cephalopods and the exploration of non-animal research methods.
As the healthcare technology industry evolves, striking a balance between scientific advancements and ethical treatment of research subjects, including octopuses, remains crucial for the future of medical breakthroughs.
Editor's Note: This article has been updated to note that Eve Barrs is a former Chicago's Shedd Aquarium employee and that Amy Hancock-Ronemus, DVM, is a former veterinarian at the University of Chicago’s Marine Biological Laboratory.
Dig Deeper on Clinical trials and evidence

WHO identifies first bird flu death in 59-year-old man

Octopus Deploy reels in Codefresh for GitOps expertise

Understanding the Pharmaceutical Drug Development Life Cycle

House of Representatives Votes to Declassify COVID-19 Origins
A national survey revealed that while many Americans are comfortable with artificial intelligence in healthcare, some have ...
AI revealed insights into the relationship between lung cancer therapy and heart complications, which could help minimize cardiac...
Houston Methodist has successfully piloted ambient clinical intelligence and AI tools to bolster efficiency and cost savings ...
Understanding the quality bonus payment program is critical to appreciating Medicare Advantage and discussing the calls for ...
Only 45% of individuals who received a surprise bill challenged it and only 43% of those who were denied coverage appealed the ...
Medicare includes four different segments that each insure a wide variety of services and supplies for enrollees.
Epic's goal to bring customers live on TEFCA by the end of 2025 complements Carequality's plan to align with TEFCA as the ...
Key considerations for selecting an EHR vendor include assessing practice needs, conducting a thorough market scan and evaluating...
The proposed rule, which is available for public comment until October 8, 2024, would require HHS contractors to use certified ...
NIST encouraged organizations to implement its three post-quantum cryptography standards to prepare for the emergence of powerful...
A healthcare data breach at Alabama Cardiovascular Group affected upwards of 280,000 individuals after an unauthorized party ...
Lawsuits often follow a healthcare data breach, but understanding what drives litigation trends can help healthcare organizations...
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Understanding Ethical Issues of Research Participation from the Perspective of Participating Children and Adolescents: A Systematic Review
Stacey crane.
Predoctoral Fellow, Indiana University School of Nursing, 1111 Middle Dr., NU345, Indianapolis, IN, 46202, 513-508-3936
Marion E. Broome
Ruby F. Wilson Distinguished Professor and Dean, Vice-Chancellor for Nursing Affairs, Duke University School of Nursing, 307 Trent Drive, Durham, NC, 27710, 919-684-9444
Associated Data
TABLE S2. Articles Included in Sample: Methodologies Used
TABLE S3. Articles Included in Sample: Demographics of Participating Children and Adolescents
The past twenty years have seen distinct shifts in the way the participation of children and adolescents in research is viewed. This has been emphasized by the growing pediatric research enterprise. Additional information on children’s and adolescents’ experiences during research participation is needed to better inform researchers on the ethical conduct of research with this vulnerable population.
The objective of this analysis was to examine ethical issues in research with children and adolescents from their perspective as participants, including: assent, parental consent, risk perception, impact of research participation, and incentives.
This systematic review was conducted per the Long et al. framework by means of an iterative searching process. Using the key words ‘research ethics’ and ‘child or pediatric or adolescent’, PubMed, CINAHL, and EBSCOhost databases were searched to identify articles. Limitations placed on the original searches were: English language, year of publication between 2003–2014, humans, abstract available, and age birth–18 years.
Twenty-three empiric studies were identified and formed the sample. Included studies represented a diverse range of areas of research, methods, settings, sample demographics, authors, and journals.
Even young children demonstrated the ability to understand essential elements of research, although there is variability in children’s level of understanding. Trust was a significant contributing factor to children’s and adolescents’ participation in research, and also shaped their assessments of risk. Research participation was mainly beneficial for children and adolescents. Incentives were mainly viewed positively, although concerns of possible undue influence were expressed.
Linking Evidence to Action
This systematic review highlights the importance of including the perspectives of children and adolescents and provides researchers and nurse clinicians with best practices for involving children in research.
Introduction
In 2004, the Institute of Medicine published a report, ‘Ethical Conduct of Clinical Research Involving Children’, the purpose of which was to review federal regulations, reports and research and make recommendations about ethical research involving children ( Institute of Medicine, 2004 ). Themes of the report included the need for:
- Well-designed and executed research with children to improve the health of children and future generations worldwide;
- Children to not be either burdened or excluded from participation in research;
- A robust system for protecting child and adolescent research participants, including additional resources like experts in physiology and development, to recognize and address unique ethical issues.
In the ensuing years, researchers have continued to recognize the need to balance the inherent vulnerability of children and adolescents with the necessity to research their unique needs and perspectives ( Broome, Kodish, Geller, & Siminoff, 2003 ; Hurst, 2008 ; Levine et al., 2004 ; Solomon, 2013 ). There have been new research investigations with child and adolescent participants, outside of traditional clinical research settings and those using more novel designs. More child/adolescent populations have been identified as vulnerable within the research context; indeed the current prevalence of vulnerable populations has compromised our understanding of the unique needs of any particular vulnerable population ( Levine et al., 2004 ). As the research enterprise continues to evolve it is important to better inform researchers about the unique needs that should inform the ethical conduct of research with children and adolescents.
Much of our understanding of the conduct of ethical research with children and adolescents has been formulated based on general ethical principles, without consideration of the heterogeneity of children and adolescents research participants ( Carter, 2009 ; Hurst, 2008 ; Levine et al., 2004 ). It is unclear what, if any, voice children and adolescents have had in the development of these ethical guidelines. The objective of this systematic review was to examine ethical issues surrounding research with children and adolescents from their perspective as participants. Specific questions that guided this review were:
- What research methods have been used to understand children’s and adolescents’ experiences of participating in research?
- What has been learned from children and adolescents about assent and parental consent for research participation?
- How do children and adolescents perceive the risks inherent with research participation?
- What impact have children and adolescents identified as a result of their research participation?
- What has been learned from child and adolescent research participants regarding the use of incentives?
This systematic review was conducted using the framework described by Long, Godfrey, Randall, Brettle, and Grant (2002) . An iterative searching process was used including three stages: scoping, refinement and confirmation ( Long et al., 2002 ). After a broad search and relevance check on initially identified studies, inclusion and exclusion criteria were refined and questions refocused. Searches were then rerun. References cited in included studies were reviewed to identify further relevant studies. A PRISMA flowchart was used to graphically represent search procedures ( Moher, Liberati, Tetzlaff, & Altman, 2009 ).
Search Methods
Using the key words ‘research ethics’ and ‘child or pediatric or adolescent’, PubMed, CINAHL, and EBSCOhost (including Academic Search Premier, Health Source, PsycINFO, SocINDEX, Family & Society Studies Worldwide, MasterFILE Premier, Biomedical Reference Collection, Applied Science & Technology Source, Historical Abstracts) databases were searched to identify potentially relevant published articles. Limitations placed on the original searches were: English language, year of publication between 2003 and 2014, humans, abstract available, and age birth – 18 years. Due to the high volume of articles initially retrieved (PubMed = 2,240 and EBSCOhost = 3,313) additional limitations were placed on searches. Explicitly, in PubMed a limitation was added for the MeSH search term ‘Ethics, research’ and in EBSCOhost a limitation was placed using ‘Research ethics’ as a major concept. Using this process, these searches yielded a combined total of 1,424 potentially relevant published articles (including 56 duplicates).
Search Outcomes
Articles were then reviewed to select those that met criteria for inclusion. Inclusion criteria included: 1) empiric research studies from the child/adolescent perspective; 2) articles considering ethical issues in research with children/adolescents or child/adolescent perspectives of research participation; and 3) ethical issues as the primary focus of the paper. Exclusion criteria included articles that focused solely on: 1) broad medical ethics or bioethics, or 2) research procedures or regulatory approval processes. From the original search 19 articles met these criteria. Manual searching yielded four further articles meeting the criteria for inclusion. In the end, 23 articles provided the sample for this analysis. Table 1 lists the included articles. Figure 1 illustrates the search results and screening procedures.

PRISMA Diagram of Search Results and Screening
Articles Included in Sample
| Article | Purpose/Aims |
|---|---|
| ( ) | To evaluate factors that would influence children and adolescents’ decision-making for research participation, in terms of the impact of monetary and other incentives. |
| ( ) | To describe the ethical challenges and acceptability of the cold pressor test from the perspective of researchers, children and parents. |
| ( ) | To determine adolescents’ perceptions of participation in research involving the collection of biomarkers via blood, saliva and/or urine samples. |
| ( ) | To examine the capacity of 4th, 7th, and 10th graders, as well as college students, to understand their rights in research and the extent to which this capacity can be enhanced following exposure to The Research Participants’ Bill of Rights. |
| ( ) | To maximize the amount of information children and adolescents understand about the risks and benefits associated with participation in a biomedical research study. |
| ( ) | To compare the effects of research participation on children who have experienced traumatic events with children who have not, in their perception of the risks and benefits of research participation and their understanding of assenting to participate. |
| ( ) | To explore the factors that influenced adolescents’ decisions to participate in an ED-based research study about youth violence, and to determine the feelings elicited by being a research subject. |
| ( ) | To evaluate children’s perceptions of completing a research survey about their exposure to violence. |
| ( ) | To describe the experiences and perspectives of homeless young people as participants in research, including their perspectives and advice on how to handle ethical challenges posed by such research. |
| ( ) | To define an appropriate process for providing research results to participants in pediatric oncology clinical trials, based on participants’ needs and attitudes. |
| ( ) | To empirically examine generational and ethnic variations about ethical issues in youth drug use and suicide survey research in order to: a) evaluate risks and benefits, b) establish guardian permission requirements, c) develop disclosure and confidentiality policies, and d) identify appropriate incentives for recruitment. |
| ( ) | To examine distress related to answering personal survey questions about drug use, suicidal behavior, and physical and sexual abuse in multiple convenience samples of adolescents. |
| ( ) | To investigate children’s and teachers’ perceptions of emotional responses to sociometric testing, and whether children understood their research rights as participants. Also to measure both quantitative and qualitative aspects of the sociometric experience. |
| ( ) | To determine older adolescents’ responses after learning that they were participants in a research study that involved identification of participants using Facebook. |
| ( ) | To explore parent and children’s views of anonymity and the intrinsic link to the ethic of confidentiality with the objective of questioning the taken- for-granted nature of the ethic of anonymity. |
| ( ) | To increase our understanding of how diabetic and at-risk adolescents (i.e., those who are obese and/or have a family history of diabetes) and their parents perceive risks and make decisions about research participation. |
| ( ) | To explore what views children 10–12 years of age express about medical research and participation in such research. |
| ( ) | To explore 10- to 13-year-old children’s views on medical research, trust, information, decision making, and their views on data sampling and risk identification. |
| ( ) | To examine factors influencing informed assent, initial involvement, and ongoing involvement in HIV- focused community based participatory research for African American children. |
| ( ) | To assess what children aged 7 to 18 with cancer understand about research, their research-related treatment, and their preferences for inclusion in decision-making. |
| ( ) | To examine the extent to which parents and adolescents participating in the Treatment for Adolescents With Depression Study understood key aspects of the study. |
| ( ) | To prospectively assess youths’ and their parents’ attitudes and experiences about participation in clinical treatment research. |
| ( ) | To detail how parents as well as children view and assess the risks to involving children in health research. This paper focuses on one of the factors, a matter of trust, that shaped Canadian parents’ and children’s perceptions and assessments of risk in child health research. |
Quality Appraisal
All articles in the sample were evaluated using an instrument to assess overall quality; the Evaluative Tool for Quantitative Research Studies ( Long et al., 2002 ) or the Critical Review Form for Qualitative Research ( Letts et al., 2007 ). Mixed methods studies were assessed using both instruments. These tools were used to ensure the overall quality of studies within the sample, to summarize study findings, and as a method for ensuring inter-rater agreement between the two authors. Both authors independently completed assessments of 14 articles in the sample, three articles at a time, comparing results until substantive agreement was achieved. The nine remaining articles were then assessed by the first author, with the second author performing a secondary confirmation. All articles included in the sample met a minimum of 80% of the instruments’ criteria. The potential for bias in the quality appraisal was minimal as both authors are trained in research ethics and experienced in conducting research with pediatric and adolescent participants.
Data Abstraction and Synthesis
Data abstracted from the articles included: journal, country of publication, purpose, approach, method, data collection techniques, research context, sample size, sample characteristics (ages, health, and research experience), method of child assent and parent consent, and findings.
For further details of the articles in the sample, including their findings, journal and country of publication, research methodologies used, and demographics of the children and adolescents studied in each article, see Tables S1 through S3 online.
Characteristics of Reviewed Studies
The sample reflected a variety of different methods and settings. Of the 23 articles, 11 used a descriptive, quantitative design, eight used a descriptive qualitative design, two used mixed methods, and two used a quantitative design that involved testing an intervention. Eleven of the articles involved retrospective reflection on a research experience and one involved a prospective, longitudinal design. The remaining 11 articles considered participants’ current views on research issues. In terms of setting, 10 of the articles involved studies conducted at or through a hospital, nine at schools, three were community based, and one did not indicate the study site.
Children and adolescents were asked to either reflect on their personal experience as a research participant, on research in general, or on a specific hypothetical research situation. Hypothetical scenarios reflected a variety of medical treatments, clinical trials, diagnostic procedures, collection of laboratory samples and/or descriptive research studies.. In other studies children were asked to reflect on their experiences as part of a study they just participated in including those studying exposure to violence, depression, oncology, pain, drug testing, sociometric testing, and health screening. In most cases these reflections were obtained at the end of their participation in the study. In five of the studies children were asked to reflect on their overall impressions of research participation.
Methods for data collection varied. Four of the studies involved either semi-structured or unstructured individual interviews, one involved a focus group, and two studies used a combination of focus groups and interviews. Eight of the studies used written instruments completed at home, school, hospital, or juvenile justice program settings. Seven studies involved structured quantitative instruments that were completed in individual interviews. One study involved a structured quantitative survey conducted orally in a classroom.
Obtaining Assent and Parental Consent
Per the Declaration of Helsinki, “when a potential research subject who is deemed incapable of giving informed consent is able to give assent to decisions about participation in research, the [researcher] must seek that assent in addition to the consent of the legally authorized representative” ( World Medical Association, 2013 ). When conducting research with children and adolescents, when and how to obtain assent versus informed consent (for adolescents) and parental consent has been ethically debated ( Giesbertz, Bredenoord, & van Delden, 2014 ; Lambert & Glacken, 2011 ). In general, literature and policies support researchers seeking assent from all child and adolescent participants in addition to parental consent. In this sample of 23 articles, seven indicated assent was obtained from the participating children/adolescents although the method was not discussed, seven obtained assent using a written form, and three obtained assent verbally. Two articles took the completion of written survey instruments as an indication of implied consent, and the remaining seven articles did not discuss assent procedures.
The majority of child and adolescent research participants were able to comprehend the purpose and nature of research, research risks and benefits, and the voluntary nature of research participation. Comprehension increased with grade level, with 15 – 16 year olds having a similar understanding of research as adults ( Bruzzese & Fisher, 2003 ; Unguru, Sill, & Kamani, 2010 ). However, while even young children could understand complex concepts like research risks and benefits, there remained a significant minority of children under around the age of 10 who had difficulties understanding research concepts ( Bruzzese & Fisher, 2003 ; Burke, Abramovitch, & Zlotkin, 2005 ). In addition, cultural factors, including race, influenced children’s interpretation of research information ( Traube, Cederbaum, Kerkorian, Bhupali, & McKay, 2013 ; Unguru et al., 2010 ).
Noteworthy challenges to children’s comprehension, including their inability to specify any risks associated with previously collected data or samples, were found in a multi-year longitudinal study. This highlights the need to view assent as an ongoing process to be reaffirmed in studies with research activities at more than one time point ( Swartling, Hansson, Ludvigsson, & Nordgren, 2011 ). In addition, challenges were found in children’s ability to understand clinical trials despite researchers’ explanations; with children’s expectations for clinical improvement as a result of clinical trial participation sometimes being unrealistically high ( Unguru et al., 2010 ; Wagner, Martinez, & Joiner, 2006 ).
Most children preferred a shared decision-making model when deciding to participate in research, where they were actively involved and supported by parents, doctors, and researchers ( Swartling, Helgesson, Ludvigsson, Hansson, & Nordgren, 2014 ; Unguru et al., 2010 ). One challenging situation, however, was indicated by children with cancer who did not feel free to dissent to clinical trial enrollment ( Unguru et al., 2010 ). In another, homeless adolescents felt strongly that they should be able to independently consent to participate in research, without requiring parental approval ( Ensign, 2006 ).
An important consideration is the type of parental consent processes that should be used in research with children and adolescents. Three studies specified that parental consent was obtained but did not indicate a method, eight of the articles obtained consent from parents using a written form, three obtained verbal parental consent, and three articles did not discuss parental consent processes. Other processes used included passive parental consent (1), implied parental consent (1), and not obtaining any parental consent (2). Of the two articles that did not obtain any parental consent one was conducted with homeless adolescents, and the other involved a survey completed at school ( Ellonen & Pösö, 2011 ; Ensign, 2006 ). For this latter study, the children aged 12–16 years decided whether they wished to participate in the study and parents were notified afterwards regarding their child’s participation. Participation rates were lower when active parental consent processes were used in school-based research ( Langhinrichsen-Rohling, Arata, O’Brien, Bowers, & Klibert, 2006 ). One article demonstrated that an active vs. passive parental consent procedure did not reduce the risk of adolescents completing a survey of high-risk behavior feeling upset ( Langhinrichsen-Rohling et al., 2006 ). However, other findings suggested that whether parents were present during the assent discussion impacted whether adolescents perceived their decision to participate in research to be autonomous ( Cohn, Ginsburg, Kassam-Adams, & Fein, 2005 ).
Specific suggestions from children and adolescents on improving assent processes included: for researchers to speak directly to children about research participation – not simply through their parents, ensuring written materials are written in a way that is appealing and understandable, and providing written information instead of using e-mails or websites ( Brawner, Volpe, Stewart, & Gomes, 2013 ; Burke et al., 2005 ; Swartling et al., 2011 ; Swartling et al., 2014 ; Unguru et al., 2010 ). Specific tools that were demonstrated to enhance children’s and adolescents’ comprehension of research included an assent quiz, and a specific lesson on research rights ( Bruzzese & Fisher, 2003 ; Chu, DePrince, & Weinzierl, 2008 ).
Perception of Research Risks
The presence or absence of trust was perceived by children as a contributing factor to being involved in research, and also shaped their assessments of risk ( Brawner et al., 2013 ; Traube et al., 2013 ; Woodgate & Edwards, 2010 ). Findings in the sample of articles suggested that children and adolescents are most willing to participate in research when they feel safe ( Brawner et al., 2013 ; O’Reilly, Karim, Taylor, & Dogra, 2012 ; Swartling et al., 2011 ; Traube et al., 2013 ). Most children and adolescents expected that researchers and their parents would protect them during their research participation ( Brawner et al., 2013 ; Woodgate & Edwards, 2010 ). Children tended to believe that if a researcher behaved unethically or caused harm, the researcher would suffer consequences professionally and personally ( Traube et al., 2013 ). When asked in one study to identify factors that shaped their perceptions and assessments of risks in research children identified: the potential for harm to the child; the potential for good for the child and children in general; the burden to the child and family; and the trust experienced by the child and their parents ( Woodgate & Edwards, 2010 ).
However, weighing of risks and benefits may be age dependent in children, with young children more likely to choose options they are familiar with, and older children paying more attention to the advantages and disadvantages of each option ( Burke et al., 2005 ). In addition, Traube et al. (2013) found that both race and relationship of the researchers to participants impacted children’s trust of researchers, with African-American children having more trust in researchers who weren’t from their own community, and the most trust in Caucasian researchers who had no connection to their community.
There was also evidence that research participants interpreted and used risk information subjectively, based on their personal experiences, and may overlook risk probability information ( Reynolds & Nelson, 2007 ). One article demonstrated that adolescents and adults evaluate risks using a similar process where first the magnitude of the risks are considered, followed by consideration of the probability of the risks ( Reynolds & Nelson, 2007 ). If the magnitude was acceptable, adolescents were willing to tolerate the stated or perceived risks of a research procedure, regardless of probability.
Adolescents were very concerned regarding how their information and samples would be used, and in particular whether information would be shared with their parents ( Brawner et al., 2013 ). Adolescents and parents were found to have different opinions about research disclosures; parents often wanted to receive their children’s research information, but adolescents reported wanting to withhold private and sensitive findings ( Brawner et al., 2013 ). Specific suggestions adolescents made to researchers included allowing their parents and/or friends to attend data collection visits, being able to participate in research along with their friends, and in research where blood, urine, or other biological samples are taken to explicitly inform the adolescent whether or whether not pregnancy, sexually transmitted disease, or drug testing would be performed ( Brawner et al., 2013 ).
Impact of Research Participation Experiences
Twelve studies examined children’s feelings about their own research participation. When asked how the participation affected them, overall the majority of ratings and reports were positive. Specific benefits reported by children/adolescents included: 1) learned something new, 2) helped others, 3) helped other people learn something new, 4) felt ‘empowered’, 5) liked talking about themselves to someone else, 6) enjoyed the procedures, 7) thought filling out forms was ‘fun’, 8) trusted in researchers, 9) thought they experienced ‘clinical improvement’, and 10) would be willing to participate in another study ( Bruzzese & Fisher, 2003 ; Chu et al., 2008 ; Ensign, 2006 ; Fernandez et al., 2009 ; Reynolds & Nelson, 2007 ; Swartling et al., 2014 ; Wagner et al., 2006 ).
In the studies asking about positive aspects of participation there were always some children who did not report positive experiences. The percentages in those studies who reported negative experiences ranged from 4% – 6.1% ( Cohn et al., 2005 ; Ellonen & Pösö, 2011 ). Negative reports associated with research participation included: anxiety, feeling upset, being bored, worry about being identified as high risk for disease, and inconvenient or painful (i.e. blood draws) procedures ( Bruzzese & Fisher, 2003 ; Wagner et al., 2006 ). In some cases, those who rated aspects of research experiences more negatively also rated other aspects positively, indicating an overall positive cost-benefit ratio of research participation ( Cohn et al., 2005 ). Interestingly, of the few studies that examined factors associated with negative or positive appraisals of research participation, only one found that a demographic variable, namely the child’s level of emotional problems, was associated with their appraisals (i.e. there was a positive association between emotional problems and negative feelings towards research participation) ( Cohn et al., 2005 ; Ellonen & Pösö, 2011 ; Swartling et al., 2011 ). No other demographic variables –including age, gender, data collection strategy, type of precipitating event that lead to inclusion in the study (i.e. violence), or anxiety - were reported as significantly associated with children’s appraisals.
Use of Incentives
In seven of the articles a cash incentive of between $10 and $50 was provided to participants. Other incentives used included: small tokens or prizes, $10 phone cards, movie gift certificates, psychology course credits, and a raffle for a gift certificate). Three articles did not provide incentive to participants. Twelve articles did not discuss whether participants were provided with incentives. One article where studies were conducted at schools provided the school with $1 per participant recruited to the study.
There was an interesting range of opinions expressed by children and adolescents about the usefulness of incentives. In five of the studies, at least some of the participants thought cash incentives were a preferred form of incentive ( Brawner et al., 2013 ; Bruzzese & Fisher, 2003 ; Ensign, 2006 ; Fernandez et al., 2009 ; Langhinrichsen-Rohling et al., 2006 ). Rationale for this included: justice, pleasure associated with receiving cash, and compensation for time spent, discomfort experienced, and effort expended. In a few studies the issue of ‘how much is too much’, in terms of cash incentives as a coercive factor, was explored with children and adolescents. In one study, some adolescents voiced concerns that disproportionately large amounts of cash could be coercive for homeless youth ( Ensign, 2006 ). In another, ethnic minority children were concerned that financial incentives could potentially undermine altruistic motivations, or even tempt youth into providing false information ( Mayeux, Underwood, & Risser, 2007 ). In another study, adolescents felt that cash was not coercive for older children who had a better understanding of the role of incentives ( Vitiello et al., 2007 ).
Although parental consent for participation remains the first step in involving children and adolescents in most research, researchers and human research ethics committees are now taking assent to participate in children aged 7–12 and consent from adolescents aged 13–18 far more seriously. This systematic review confirms that obtaining children’s and adolescents’ assent to participate in research is valid and important, as even young children have demonstrated the ability to understand the essential elements of research ( Burke et al., 2005 ; Unguru et al., 2010 ). Some of the variability in levels of understanding reported in studies with children likely reflects how assent forms were written, as opposed to developmental differences ( Burke et al., 2005 ). The challenge for researchers is to find better ways to get information across to children. This problem, while relevant for all research participants, is especially pertinent in younger children who have less life experience and are challenged with a less developed ability to understand new experiences ( Brawner et al., 2013 ; Swartling et al., 2014 ). Assent processes and instruments need to be created with the assistance of child development specialists and piloted with children before being used in a research study ( Burke et al., 2005 ). Researchers should also consider using quizzes to assess children’s understanding of assent information. In addition to setting an empirical standard for assessing understanding, assent quizzes also provide additional opportunities to interact with children about assent information ( Chu et al., 2008 ).
The decision-making model used in research consent and assent processes needs to reflect the context. With the adolescent population, in particular, there is a need to balance the desire for privacy and autonomy with inclusion of parents ( Cohn et al., 2005 ; Fisher, 2003 ). Both adolescents and parents are sympathetic to the ethical dilemmas researchers face when conducting sensitive research with adolescents ( Fisher, 2003 ). A priori consultation with representative adolescents and parents can provide guidance for the selection of consent and assent procedures within challenging contexts ( Fisher, 2003 ). While this type of consultation may seem burdensome for researchers, it demonstrates that researchers respect local norms regarding parental decision-making and do not wish to inadvertently undermine the parent–child relationship ( Fisher, 2003 ).
A key gap in the findings of this review is consideration of whether children and adolescents, beyond simply understanding their research rights, are capable of applying this knowledge and of actually exerting their research rights ( Bruzzese & Fisher, 2003 ; Unguru et al., 2010 ). For example, is a child truly capable of asserting and following through on their desire to stop participating in a research study or dissenting to participate?
Findings of this systematic review demonstrate that children and adolescents have a realistic perception of research risks, and that trust - towards both parents and researchers - is essential in establishing a safe environment for children and adolescents to participate in research. As a result, researchers must establish a mutual respect with child and adolescent participants; if their trust is eroded this could have implications for both the researcher-child and the parent-child relationship ( Woodgate & Edwards, 2010 ). In addition, when performing sensitive research with adolescents, researchers should consider obtaining a federal-wide assurance to protect all data collected for use solely in research, and in particular to prevent data from being used in legal proceedings ( Langhinrichsen-Rohling et al., 2006 ).
Researchers need to appreciate that the assessment of risk is an ongoing process throughout a research study, beyond simply explanations provided when obtaining assent, and that ethnicity and context play important roles in children’s and adolescents’ perceptions of risk. In a study of African-American children, it was found that children were more likely to trust researchers from outside their neighborhood, in particular Caucasian researchers, over and above researchers they knew from their own community ( Traube et al., 2013 ). Children in this study seemed to be fearful that a researcher from their own neighborhood might tell their parents what they shared ( Traube et al., 2013 ). This is particularly interesting as the same sample of children reported that during consent processes they believed the veracity of information provided from African-American researchers over that of Caucasian researchers ( Traube et al., 2013 ).
Impact of Research Participation
Findings from this review provide evidence that research participation can be beneficial for children and adolescents. The overwhelming majority of participants confirmed a willingness to participate in research again. Children and adolescents also identified reasons for participation in research as including altruistic motivations to help others and their own learning.
This review confirmed that most children prefer to be involved in the decision-making of whether they will participate in research. In addition, soliciting children’s and adolescents’ opinions about their involvement in illness management decision-making has been found to be related to adherence to care regimens ( Miller & Jawad, 2014 ). This decision-making involvement could also be important in intervention research where children’s participation is important to the integrity of the intervention.
All research with children and adolescents could benefit from inclusion of a short interview or survey with participants to gauge their degree of satisfaction with the study. If this were done it should be formative rather than summative. That is, the responses from participants early in the study could help shape aspects of the study to enhance the experience for future participants. Talking with children and adolescents about the process of research participation, beyond the actual study, may also be useful in enhancing engagement and future participation in research.
In this review, a common reason children and adolescents gave for participating in research was incentives. Incentives for the most part were viewed positively, although some children did share that the amount of cash incentives should be carefully considered by researchers. Based on findings from this review the age of the child and their vulnerability status needs to be considered when developing plans for incentives. Younger children do not have the same understanding of monetary incentives and could be better suited to more age appropriate incentives such as toys, books, and movie passes. Researchers could consider consulting parents or adolescents from the target population when designing a study to obtain their perceptions about the timing, type, and amount of incentives. Children and adolescents who are homeless or very financially disadvantaged require special consideration, as these participants may weigh incentives differently from those who are more advantaged. For all children and adolescents, per the findings of this integrative review, when obtaining assent/consent researchers should include non-monetary elements as a benefit of study participation including: helping other children learn things, learning something new themselves, and making others’ lives better.
Conclusions
Although there have been many studies on obtaining informed consent and assent when conducting research with ill children, historically there has been much less emphasis placed on children who are involved in research in other contexts. In addition, few studies have focused on the perspectives of children and adolescents themselves. The objective of this systematic review was to examine ethical issues in research with children and adolescents from their perspective as participants, related to assent, parental consent, risk perception, impact of research participation, and incentives. This systematic review highlights the importance of including the voice of children and adolescents in the debate regarding the ethical conduct of research. Children and adolescents are a vulnerable population in the research context, formed of diverse individuals with unique, varying needs. The wide variety of strategies used in the studies described herein exemplifies that in addition to primary research studies of children’s and adolescents’ perspectives of research participation, secondary objectives related to examining their experience as participants can feasibly be added into any pediatric research study. This analysis highlights how researchers and nurses working with children and adolescents enrolled in research can expand their voice and encourage the children to share their experiences in terms of benefits, risks and challenges. It is through linking the evidence found in these studies with their own practice that researchers can improve the experience of and benefits to child and adolescent research participants.
- Assent processes and instruments need to be created with the assistance of child development specialists and piloted with children before being used.
- A priori consultation with representative adolescents and parents can provide guidance for developing consent and assent procedures within challenging contexts.
- A key gap is consideration of whether children and adolescents, beyond simply understanding their research rights, are capable of applying this knowledge and of actually exerting their research rights.
- Researchers need to appreciate that the assessment of risk is an ongoing process throughout a research study, beyond simply explanations provided when obtaining assent and/or consent.
- All research with children and adolescents could benefit from inclusion of a short, formative, off-study interview or survey with participants to gauge their experience in the study.
- The age of the child and their vulnerability status needs to be considered when selecting incentives.
Supplementary Material
Supplemental tables.
TABLE S1. Articles Included in Sample: Summary and Characteristics
Contributor Information
Stacey Crane, Predoctoral Fellow, Indiana University School of Nursing, 1111 Middle Dr., NU345, Indianapolis, IN, 46202, 513-508-3936.
Marion E. Broome, Ruby F. Wilson Distinguished Professor and Dean, Vice-Chancellor for Nursing Affairs, Duke University School of Nursing, 307 Trent Drive, Durham, NC, 27710, 919-684-9444.
- Bagley SJ, Reynolds WW, Nelson RM. Is a “Wage-Payment” model for research participation appropriate for children? Pediatrics. 2007; 119 (1):46. doi: 10.1542/peds.2006-1813. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birnie KA, Noel M, Chambers CT, von Baeyer CL, Fernandez CV. The cold pressor task: Is it an ethically acceptable pain research method in children? Journal of Pediatric Psychology. 2011; 36 (10):1071–1081. doi: 10.1093/jpepsy/jsq092. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brawner BM, Volpe EM, Stewart JM, Gomes MM. Attitudes and beliefs toward biobehavioural research participation: Voices and concerns of urban adolescent females receiving outpatient mental health treatment. Annals of Human Biology. 2013; 40 (6):485–495. doi: 10.3109/03014460.2013.806590. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Broome ME, Kodish E, Geller G, Siminoff LA. Children in research: New perspectives and practices for informed consent. IRB: Ethics and Human Research, Suppl. 2003; 25 (5):S20–S25. [ PubMed ] [ Google Scholar ]
- Bruzzese JM, Fisher CB. Assessing and enhancing the research consent capacity of children and youth. Applied Developmental Science. 2003; 7 (1):13–26. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=aph&AN=8699738&site=ehost-live . [ Google Scholar ]
- Burke TM, Abramovitch R, Zlotkin S. Children’s understanding of the risks and benefits associated with research. J Med Ethics. 2005; 31 (12):715–720. doi: 10.1136/jme.2003.003228. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carter B. Tick box for child? The ethical positioning of children as vulnerable, researchers as Barbarians and reviewers as overly cautious. International Journal of Nursing Studies. 2009; 46 (6):858–864. doi: 10.1016/j.ijnurstu.2009.01.003. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chu AT, DePrince AP, Weinzierl KM. Children’s perception of research participation: Examining trauma exposure and distress. Journal of Empirical Research on Human Research Ethics. 2008; 3 (1):49–58. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2008-03332-005&site=ehost-live ; [email protected]. [ PubMed ] [ Google Scholar ]
- Cohn JM, Ginsburg KR, Kassam-Adams N, Fein JA. Adolescent decisional autonomy regarding participation in an emergency department youth violence interview. American Journal of Bioethics. 2005; 5 (5):70–74. doi: 10.1080/15265160500246319. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ellonen N, Pösö T. Children’s experiences of completing a computer-based violence survey: ethical implications. Children & Society. 2011; 25 (6):470–481. doi: 10.1111/j.1099-0860.2010.00292.x. [ CrossRef ] [ Google Scholar ]
- Ensign BJ. Perspectives and experiences of homeless young people. Journal of Advanced Nursing. 2006; 54 (6):647–652. doi: 10.1111/j.1365-2648.2006.03853.x. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fernandez CV, Gao J, Strahlendorf C, Moghrabi A, Pentz RD, Barfield RC, … Kodish E. Providing research results to participants: Attitudes and needs of adolescents and parents of children with cancer. Journal of Clinical Oncology. 2009; 27 (6):878–883. doi: 10.1200/JCO.2008.18.5223. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fisher CB. Adolescent and parent perspectives on ethical issues in youth drug use and suicide survey research. Ethics Behav. 2003; 13 (4):303–332. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2004184880&site=ehost-live . [ PubMed ] [ Google Scholar ]
- Giesbertz NAA, Bredenoord AL, van Delden JJM. Clarifying assent in pediatric research. European Journal of Human Genetics. 2014; 22 (2):266–269. doi: 10.1038/ejhg.2013.119. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hurst SA. Vulnerability in research and health care; Describing the elephant in the room? Bioethics. 2008; 22 (4):191–202. [ PubMed ] [ Google Scholar ]
- Institute of Medicine. The ethical conduct of clinical research involving children. Washington, DC: National Academies Press; 2004. [ PubMed ] [ Google Scholar ]
- Lambert V, Glacken M. Engaging with children in research: Theoretical and practical implications of negotiating informed consent/assent. Nurs Ethics. 2011; 18 (6):781–801. doi: 10.1177/0969733011401122. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Langhinrichsen-Rohling J, Arata C, O’Brien N, Bowers D, Klibert J. Sensitive research with adolescents: Just how upsetting are self-report surveys anyway? Violence & Victims. 2006; 21 (4):425–444. Retrieved from http://media.proquest.com/media/pq/classic/doc/1096430801/fmt/pi/rep/NONE?hl=&cit%3Aauth=Langhinrichsen-Rohling%2C+Jennifer%3BArata%2C+Catalina%3BO%27Brien%2C+Natalie%3BBowers%2C+David%3BKlibert%2C+Jeffrey&cit%3Atitle=Sensitive+Research+With+Adolescents%3A+Just+How+Upsetting+Are+Self-Report+Surveys+Anyway%3F&cit%3Apub=Violence+and+Victims&cit%3Avol=21&cit%3Aiss=4&cit%3Apg=425&cit%3Adate=Aug+2006&ic=true&cit%3Aprod=ProQuest&_a=ChgyMDE0MTAwOTIyMDI0MTM2Mjo5OTgwNjUSBjExNDA1MBoKT05FX1NFQVJDSCIOMTQwLjE4Mi42Ny4yMTcqBTQ1NjE5MgkyMDg1MzE2NTA6DURvY3VtZW50SW1hZ2VCATBSBk9ubGluZVoCRlRiA1BGVGoKMjAwNi8wOC8wMXIKMjAwNi8wOC8zMXoAggExUC0xMDA3MDI1LTczOTgtQ1VTVE9NRVItMTAwMDAwMzkvMTAwMDAxNDctMTA0NjkxMZIBBk9ubGluZcoBB0VuZE5vdGXSARJTY2hvbGFybHkgSm91cm5hbHOaAgdQcmVQYWlkqgIoT1M6RU1TLVBkZkRvY1ZpZXdCYXNlLWdldE1lZGlhVXJsRm9ySXRlbcoCD0FydGljbGV8RmVhdHVyZdICAVniAgFO6gIA8gIA&_s=ucBTFWGYfgRjWNZzoaaQAoiq3pQ%3D . [ PubMed ] [ Google Scholar ]
- Letts L, Wilkins S, Law M, Stewart D, Bosch J, Westmorland M. Guidelines for critical review form: Qualitative studies (version 2.0) 2007 Retrieved from http://www.srs-mcmaster.ca/Portals/20/pdf/ebp/qualreview_version2.0.pdf Retrieved from Retrieved from http://www.srs-mcmaster.ca/Portals/20/pdf/ebp/qualreview_version2.0.pdf .
- Levine C, Faden R, Grady C, Hammerschmidt D, Eckenwiler L, Sugarman J The Consortium to Examine Clinical Research Ethics. The limitations of “vulnerability” as a protection for human research participants. The American Journal of Bioethics. 2004; 4 (3):44–49. [ PubMed ] [ Google Scholar ]
- Long AF, Godfrey M, Randall T, Brettle A, Grant M. Developing evidence based social care policy and practice. Part 3: Feasibility of undertaking systematic reviews in social care. 2002 Retrieved from http://usir.salford.ac.uk/13071/ Retrieved from Retrieved from http://usir.salford.ac.uk/13071/
- Mayeux L, Underwood MK, Risser SD. Perspectives on the ethics of sociometric research with children. Merrill-Palmer Quarterly. 2007; 53 (1):53–78. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2007-08527-003&site=ehost-live ; [email protected]; [email protected]. [ Google Scholar ]
- Miller VA, Jawad AF. Relationship of youth involvement in diabetes-related decisions to treatment adherence. Journal of clinical psychology in medical settings. 2014; 21 (2):183–189. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of internal medicine. 2009; 151 (4):264–269. [ PubMed ] [ Google Scholar ]
- Moreno MA, Grant A, Kacvinsky L, Moreno P, Fleming M. Older adolescents’ views regarding participation in Facebook research. Journal of Adolescent Health. 2012; 51 (5):439–444. doi: 10.1016/j.jadohealth.2012.02.001. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- O’Reilly M, Karim K, Taylor H, Dogra N. Parent and child views on anonymity: ‘I’ve got nothing to hide’ International Journal of Social Research Methodology: Theory & Practice. 2012; 15 (3):211–223. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2012-12510-003&site=ehost-live ; [email protected]. [ Google Scholar ]
- Reynolds WW, Nelson RM. Risk perception and decision processes underlying informed consent to research participation. Social Science & Medicine. 2007; 65 (10):2105–2115. doi: 10.1016/j.socscimed.2007.06.021. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Solomon SR. Protecting and respecting the vulnerable: Existing regulations or further protections? Theor Med Bioeth. 2013; 34 (1):17–28. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Swartling U, Hansson MG, Ludvigsson J, Nordgren A. “My parents decide if I can. I decide if I want to.” Children’s views on participation in medical research. Journal of Empirical Research on Human Research Ethics. 2011; 6 (4):68–75. doi: 10.1525/jer.2011.6.4.68. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Swartling U, Helgesson G, Ludvigsson J, Hansson MG, Nordgren A. Children’s views on long-term screening for type 1 diabetes. Journal of Empirical Research on Human Research Ethics. 2014; 9 (4):1–9. doi: 10.1177/1556264614544456. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Traube DE, Cederbaum JA, Kerkorian D, Bhupali C, McKay MM. African American children’s perceptions of HIV-focused community-based participatory research. Journal of Empirical Research on Human Research Ethics. 2013; 8 (1):79–90. doi: 10.1525/jer.2013.8.1.79. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Unguru Y, Sill AM, Kamani N. The experiences of children enrolled in pediatric oncology research: Implications for assent. Pediatrics. 2010; 125 (4):e876–e883. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=aph&AN=49753789&site=ehost-live . [ PubMed ] [ Google Scholar ]
- Vitiello B, Kratochvil CJ, Silva S, Curry J, Reinecke M, Pathak S, … May DE. Research knowledge among the participants in the Treatment for Adolescents with Depression Study (TADS) Journal of the American Academy of Child and Adolescent Psychiatry. 2007; 46 (12):1642–1650. [ PubMed ] [ Google Scholar ]
- Wagner KD, Martinez M, Joiner T. Youths’ and their parents’ attitudes and experiences about participation in psychopharmacology treatment research. Journal of Child & Adolescent Psychopharmacology. 2006; 16 (3):298–307. [ PubMed ] [ Google Scholar ]
- Woodgate RL, Edwards M. Children in health research: A matter of trust. J Med Ethics. 2010; 36 (4):211–216. Retrieved from http://ovidsp.ovid.com/ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=ovftk&AN=00005004-201004000-00006 ; http://jme.bmj.com/content/36/4/211.full.pdf . [ PubMed ] [ Google Scholar ]
- World Medical Association. Declaration of Helsinki: Ethical principles for medical research involving human subjects. Journal of the American Medical Association. 2013; 310 (20):2191–2194. doi: 10.1001/jama.2013.281053. [ PubMed ] [ CrossRef ] [ Google Scholar ]

COMMENTS
Research ethics are a set of principles that guide your research designs and practices in both quantitative and qualitative research. In this article, you will learn about the types and examples of ethical considerations in research, such as informed consent, confidentiality, and avoiding plagiarism. You will also find out how to apply ethical principles to your own research projects with ...
In the context of academic research, a diversity of ethical issues, conditioned by the different roles of members within these institutions, arise. Previous studies on this topic addressed mainly the perceptions of researchers. However, to our knowledge, ...
The ethical principles that guide a scientific research are based on the assurance of human freedom and dignity. They are expressed in ethical codes and guidelines used by Research Ethics Committees (RECs), which are the instances that regulate research conducted with human beings.
Ethics are a guiding principle that shapes the conduct of researchers. It influences both the process of discovery and the implications and applications of scientific findings 1. Ethical considerations in research include, but are not limited to, the management of data, the responsible use of resources, respect for human rights, the treatment ...
This article explores the ethical issues that may arise in your proposed study during your doctoral research degree.
This paper will discuss different ethical issues in research, including study design and ethical approval, data analysis, authorship, conflict of interest and redundant publication and plagiarism. I have also included two case scenarios in this paper to illustrate common ethical issues in research and publication. Go to:
It is important to adhere to ethical principles in order to protect the dignity, rights and welfare of research participants. As such, all research involving human beings should be reviewed by an ethics committee to ensure that the appropriate ethical standards are being upheld. Discussion of the ethical principles of beneficence, justice and ...
Ethical considerations in research are a set of principles that guide your research designs and practices. Scientists and researchers must always adhere to a certain code of conduct when collecting data from people. The goals of human research often include understanding real-life phenomena, studying effective treatments, investigating ...
Definition. Ethics is a set of standards, a code, or value system, worked out from human reason and experience, by which free human actions are determined as ultimately right or wrong, good, or evil. If acting agrees with these standards, it is ethical, otherwise unethical. Scientific research refers to a persistent exercise towards producing ...
Based on the historical documents in the develop-ment of ethical conduct in clinical research, a framework for evaluating our own projects is presented. To ensure that we are reporting valid and ethical research that results in generalizable knowledge requires thoughtful, systematic steps in a scientific framework.
Education in research ethics is can help people get a better understanding of ethical standards, policies, and issues and improve ethical judgment and decision making.
For the researcher, however, it often comes with unforeseen or unanticipated ethical dilemmas, even when there is ethical clearance, compliance with institutional codes and consent from families. This paper presents a meta-reflective analysis of notes from four qualitative home-based research projects as recorded in reflective journals.
In this article, we'll explore the meaning and importance of research ethics in today's research landscape. You'll learn best practices to conduct ethical and impactful research.
Clinical research advances the understanding of science and promotes human health. However, it is important to remember the individuals who volunteer to participate in research. There are precautions researchers can take - in the planning, implementation and follow-up of studies - to protect these participants in research. Ethical guidelines are established for clinical research to protect ...
Ethical considerations in research have always been challenging, including ethical concerns vis-a-vis time, funding, accessibility, and proper implementation of these concerns.
Design research and practice projects present different ethical challenges to other disciplines including the extent of and expectations from participant involvement; dynamic participant roles (e.g. from users to co-designers); changing engagement methods; expected versus actual project outputs and project durations.
The goals of this chapter are to. • Introduce the idea of research ethics. • Focus on the thinking that you will need to do about ethics when developing your research design. • Explore participant confidentiality, anonymity, and consent as foundational, but at times problematic, concepts in research ethics. 27.
The role of the REBs is to ensure research is planned and conducted in a manner that protects the rights and welfare of a project's participants ( Page & Nyeboer, 2017 ). Research ethics boards make recommendations and provide direction for the ethical conduct of a research project.
Ethical Issues in Research. Both students and faculty at Lehigh University are encouraged to become involved in the research life of the University. Departmental honors and capstone courses, as well as a number of campus fellowships and programs, offer opportunities for students to learn the skills of research and present their results.
Conflict research is rife with ethical issues, and the field is increasingly reflecting on how to best address these. ... An approved project is not always an ethical project. PS: Political Science and Politics 49(2): 299-303. Crossref. Web of Science. Google Scholar. Nwabueze R (2013) Legal and Ethical Regulation of Research Involving Human ...
Arts & Sciences. Researching the promise, perils and ethical dimensions of technology's relationship with mental health. From developing peer support apps to investigating social media users' perceptions of mental health and offering ethical leadership about privacy concerns, faculty and students in the Klingler College of Arts and Sciences are finding insights at this intersection.
Sam: Researchers proposing to do work with living people have to get approval from an institutional review board or IRB before moving ahead with a project. Jyoti Madhusoodanan: And there's also another set of rules about research involving tissues or bodies of people who are deceased. But what I discovered while reporting this is that recently ...
With the rapid development of engineering construction in China, especially the emergence of large-scale engineering projects and self-built residential houses, ethical issues in engineering have become increasingly prominent. Engineering ethics encompass the moral issues within engineering practice. Currently, engineering ethics in China is in its early stages, due to a lack of practical ...
Legal and ethical issues form an important component of modern research, related to the subject and researcher. This article seeks to briefly review the various international guidelines and regulations that exist on issues related to informed consent, ...
The research involved about 13.522 projects, of which only 34% can be considered a success. The main causes for IT projects failure were related to user's com-mitment, manager support and ...
This systematic scoping review was conducted to identify the ethical issues of AI application in healthcare, to highlight gaps, and to propose steps to move towards an evidence-informed approach ...
Abstract This article aims to shed light on ethical pitfalls that may occur when researchers conduct research with young people (aged 15-24). Young age itself does not automatically indicate vulnerability. Yet, young research participants may be in need of extraordinary measures that safeguard their well-being. The presented pitfalls centre around the issues of consent, power and agency, and ...
In the context of academic research, a diversity of ethical issues, conditioned by the different roles of members within these institutions, arise. Previous studies on this topic addressed mainly the perceptions of researchers. However, to our knowledge, no studies have explored the transversal ethical issues from a wider spectrum, including other members of academic institutions as the ...
Understanding octopus research guidelines is essential for ethical healthcare progress, ensuring breakthroughs align with moral standards and prioritize animal welfare. ... Health issues, such as parasitic and bacterial infections, are common in captive octopuses, and addressing these concerns adds another layer of complexity to their care. ...
Aims The objective of this analysis was to examine ethical issues in research with children and adolescents from their perspective as participants, including: assent, parental consent, risk perception, impact of research participation, and incentives.