- Join our Mailing List

Working locally in primary care and collaborating globally to improve respiratory health
Clinical case study - asthma, clinical case study - asthma, resource information.
- Disease management
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 16 October 2014
A woman with asthma: a whole systems approach to supporting self-management
- Hilary Pinnock 1 ,
- Elisabeth Ehrlich 1 ,
- Gaylor Hoskins 2 &
- Ron Tomlins 3
npj Primary Care Respiratory Medicine volume 24 , Article number: 14063 ( 2014 ) Cite this article
16k Accesses
2 Citations
6 Altmetric
Metrics details
- Health care
A 35-year-old lady attends for review of her asthma following an acute exacerbation. There is an extensive evidence base for supported self-management for people living with asthma, and international and national guidelines emphasise the importance of providing a written asthma action plan. Effective implementation of this recommendation for the lady in this case study is considered from the perspective of a patient, healthcare professional, and the organisation. The patient emphasises the importance of developing a partnership based on honesty and trust, the need for adherence to monitoring and regular treatment, and involvement of family support. The professional considers the provision of asthma self-management in the context of a structured review, with a focus on a self-management discussion which elicits the patient’s goals and preferences. The organisation has a crucial role in promoting, enabling and providing resources to support professionals to provide self-management. The patient’s asthma control was assessed and management optimised in two structured reviews. Her goal was to avoid disruption to her work and her personalised action plan focused on achieving that goal.
Similar content being viewed by others

Barriers to implementing asthma self-management in Malaysian primary care: qualitative study exploring the perspectives of healthcare professionals

The self-management abilities test (SMAT): a tool to identify the self-management abilities of adults with bronchiectasis

Improving primary care management of asthma: do we know what really works?
A 35-year-old sales representative attends the practice for an asthma review. Her medical record notes that she has had asthma since childhood, and although for many months of the year her asthma is well controlled (when she often reduces or stops her inhaled steroids), she experiences one or two exacerbations a year requiring oral steroids. These are usually triggered by a viral upper respiratory infection, though last summer when the pollen count was particularly high she became tight chested and wheezy for a couple of weeks.
Her regular prescription is for fluticasone 100 mcg twice a day, and salbutamol as required. She has a young family and a busy lifestyle so does not often manage to find time to attend the asthma clinic. A few weeks previously, an asthma attack had interfered with some important work-related travel, and she has attended the clinic on this occasion to ask about how this can be managed better in the future. There is no record of her having been given an asthma action plan.
What do we know about asthma self-management? The academic perspective
Supported self-management reduces asthma morbidity.
The lady in this case study is struggling to maintain control of her asthma within the context of her busy professional and domestic life. The recent unfortunate experience which triggered this consultation offers a rare opportunity to engage with her and discuss how she can manage her asthma better. It behoves the clinician whom she is seeing (regardless of whether this is in a dedicated asthma clinic or an appointment in a routine general practice surgery) to grasp the opportunity and discuss self-management and provide her with a (written) personalised asthma action plan (PAAP).
The healthcare professional advising the lady is likely to be aware that international and national guidelines emphasise the importance of supporting self-management. 1 – 4 There is an extensive evidence base for asthma self-management: a recent synthesis identified 22 systematic reviews summarising data from 260 randomised controlled trials encompassing a broad range of demographic, clinical and healthcare contexts, which concluded that asthma self-management reduces emergency use of healthcare resources, including emergency department visits, hospital admissions and unscheduled consultations and improves markers of asthma control, including reduced symptoms and days off work, and improves quality of life. 1 , 2 , 5 – 12 Health economic analysis suggests that it is not only clinically effective, but also a cost-effective intervention. 13
Personalised asthma action plans
Key features of effective self-management approaches are:
Self-management education should be reinforced by provision of a (written) PAAP which reminds patients of their regular treatment, how to monitor and recognise that control is deteriorating and the action they should take. 14 – 16 As an adult, our patient can choose whether she wishes to monitor her control with symptoms or by recording peak flows (or a combination of both). 6 , 8 , 9 , 14 Symptom-based monitoring is generally better in children. 15 , 16
Plans should have between two and three action points including emergency doses of reliever medication; increasing low dose (or recommencing) inhaled steroids; or starting a course of oral steroids according to severity of the exacerbation. 14
Personalisation of the action plan is crucial. Focussing specifically on what actions she could take to prevent a repetition of the recent attack is likely to engage her interest. Not all patients will wish to start oral steroids without advice from a healthcare professional, though with her busy lifestyle and travel our patient is likely to be keen to have an emergency supply of prednisolone. Mobile technology has the potential to support self-management, 17 , 18 though a recent systematic review concluded that none of the currently available smart phone ‘apps’ were fit for purpose. 19
Identification and avoidance of her triggers is important. As pollen seems to be a trigger, management of allergic rhinitis needs to be discussed (and included in her action plan): she may benefit from regular use of a nasal steroid spray during the season. 20
Self-management as recommended by guidelines, 1 , 2 focuses narrowly on adherence to medication/monitoring and the early recognition/remediation of exacerbations, summarised in (written) PAAPs. Patients, however, may want to discuss how to reduce the impact of asthma on their life more generally, 21 including non-pharmacological approaches.
Supported self-management
The impact is greater if self-management education is delivered within a comprehensive programme of accessible, proactive asthma care, 22 and needs to be supported by ongoing regular review. 6 With her busy lifestyle, our patient may be reluctant to attend follow-up appointments, and once her asthma is controlled it may be possible to make convenient arrangements for professional review perhaps by telephone, 23 , 24 or e-mail. Flexible access to professional advice (e.g., utilising diverse modes of consultation) is an important component of supporting self-management. 25
The challenge of implementation
Implementation of self-management, however, remains poor in routine clinical practice. A recent Asthma UK web-survey estimated that only 24% of people with asthma in the UK currently have a PAAP, 26 with similar figures from Sweden 27 and Australia. 28 The general practitioner may feel that they do not have time to discuss self-management in a routine surgery appointment, or may not have a supply of paper-based PAAPs readily available. 29 However, as our patient rarely finds time to attend the practice, inviting her to make an appointment for a future clinic is likely to be unsuccessful and the opportunity to provide the help she needs will be missed.
The solution will need a whole systems approach
A systematic meta-review of implementing supported self-management in long-term conditions (including asthma) concluded that effective implementation was multifaceted and multidisciplinary; engaging patients, training and motivating professionals within the context of an organisation which actively supported self-management. 5 This whole systems approach considers that although patient education, professional training and organisational support are all essential components of successful support, they are rarely effective in isolation. 30 A systematic review of interventions that promote provision/use of PAAPs highlighted the importance of organisational systems (e.g., sending blank PAAPs with recall reminders). 31 A patient offers her perspective ( Box 1 ), a healthcare professional considers the clinical challenge, and the challenges are discussed from an organisational perspective.
Box 1: What self-management help should this lady expect from her general practitioner or asthma nurse? The patient’s perspective
The first priority is that the patient is reassured that her condition can be managed successfully both in the short and the long term. A good working relationship with the health professional is essential to achieve this outcome. Developing trust between patient and healthcare professional is more likely to lead to the patient following the PAAP on a long-term basis.
A review of all medication and possible alternative treatments should be discussed. The patient needs to understand why any changes are being made and when she can expect to see improvements in her condition. Be honest, as sometimes it will be necessary to adjust dosages before benefits are experienced. Be positive. ‘There are a number of things we can do to try to reduce the impact of asthma on your daily life’. ‘Preventer treatment can protect against the effect of pollen in the hay fever season’. If possible, the same healthcare professional should see the patient at all follow-up appointments as this builds trust and a feeling of working together to achieve the aim of better self-management.
Is the healthcare professional sure that the patient knows how to take her medication and that it is taken at the same time each day? The patient needs to understand the benefit of such a routine. Medication taken regularly at the same time each day is part of any self-management regime. If the patient is unused to taking medication at the same time each day then keeping a record on paper or with an electronic device could help. Possibly the patient could be encouraged to set up a system of reminders by text or smartphone.
Some people find having a peak flow meter useful. Knowing one's usual reading means that any fall can act as an early warning to put the PAAP into action. Patients need to be proactive here and take responsibility.
Ongoing support is essential for this patient to ensure that she takes her medication appropriately. Someone needs to be available to answer questions and provide encouragement. This could be a doctor or a nurse or a pharmacist. Again, this is an example of the partnership needed to achieve good asthma control.
It would also be useful at a future appointment to discuss the patient’s lifestyle and work with her to reduce her stress. Feeling better would allow her to take simple steps such as taking exercise. It would also be helpful if all members of her family understood how to help her. Even young children can do this.
From personal experience some people know how beneficial it is to feel they are in a partnership with their local practice and pharmacy. Being proactive produces dividends in asthma control.
What are the clinical challenges for the healthcare professional in providing self-management support?
Due to the variable nature of asthma, a long-standing history may mean that the frequency and severity of symptoms, as well as what triggers them, may have changed over time. 32 Exacerbations requiring oral steroids, interrupting periods of ‘stability’, indicate the need for re-assessment of the patient’s clinical as well as educational needs. The patient’s perception of stability may be at odds with the clinical definition 1 , 33 —a check on the number of short-acting bronchodilator inhalers the patient has used over a specific period of time is a good indication of control. 34 Assessment of asthma control should be carried out using objective tools such as the Asthma Control Test or the Royal College of Physicians three questions. 35 , 36 However, it is important to remember that these assessment tools are not an end in themselves but should be a springboard for further discussion on the nature and pattern of symptoms. Balancing work with family can often make it difficult to find the time to attend a review of asthma particularly when the patient feels well. The practice should consider utilising other means of communication to maintain contact with patients, encouraging them to come in when a problem is highlighted. 37 , 38 Asthma guidelines advocate a structured approach to ensure the patient is reviewed regularly and recommend a detailed assessment to enable development of an appropriate patient-centred (self)management strategy. 1 – 4
Although self-management plans have been shown to be successful for reducing the impact of asthma, 21 , 39 the complexity of managing such a fluctuating disease on a day-to-day basis is challenging. During an asthma review, there is an opportunity to work with the patient to try to identify what triggers their symptoms and any actions that may help improve or maintain control. 38 An integral part of personalised self-management education is the written PAAP, which gives the patient the knowledge to respond to the changes in symptoms and ensures they maintain control of their asthma within predetermined parameters. 9 , 40 The PAAP should include details on how to monitor asthma, recognise symptoms, how to alter medication and what to do if the symptoms do not improve. The plan should include details on the treatment to be taken when asthma is well controlled, and how to adjust it when the symptoms are mild, moderate or severe. These action plans need to be developed between the doctor, nurse or asthma educator and the patient during the review and should be frequently reviewed and updated in partnership (see Box 1). Patient preference as well as clinical features such as whether she under- or over-perceives her symptoms should be taken into account when deciding whether the action plan is peak flow or symptom-driven. Our patient has a lot to gain from having an action plan. She has poorly controlled asthma and her lifestyle means that she will probably see different doctors (depending who is available) when she needs help. Being empowered to self-manage could make a big difference to her asthma control and the impact it has on her life.
The practice should have protocols in place, underpinned by specific training to support asthma self-management. As well as ensuring that healthcare professionals have appropriate skills, this should include training for reception staff so that they know what action to take if a patient telephones to say they are having an asthma attack.
However, focusing solely on symptom management strategies (actions) to follow in the presence of deteriorating symptoms fails to incorporate the patients’ wider views of asthma, its management within the context of her/his life, and their personal asthma management strategies. 41 This may result in a failure to use plans to maximise their health potential. 21 , 42 A self-management strategy leading to improved outcomes requires a high level of patient self-efficacy, 43 a meaningful partnership between the patient and the supporting health professional, 42 , 44 and a focused self-management discussion. 14
Central to both the effectiveness and personalisation of action plans, 43 , 45 in particular the likelihood that the plan will lead to changes in patients’ day-to-day self-management behaviours, 45 is the identification of goals. Goals are more likely to be achieved when they are specific, important to patients, collaboratively set and there is a belief that these can be achieved. Success depends on motivation 44 , 46 to engage in a specific behaviour to achieve a valued outcome (goal) and the ability to translate the behavioural intention into action. 47 Action and coping planning increases the likelihood that patient behaviour will actually change. 44 , 46 , 47 Our patient has a goal: she wants to avoid having her work disrupted by her asthma. Her personalised action plan needs to explicitly focus on achieving that goal.
As providers of self-management support, health professionals must work with patients to identify goals (valued outcomes) that are important to patients, that may be achievable and with which they can engage. The identification of specific, personalised goals and associated feasible behaviours is a prerequisite for the creation of asthma self-management plans. Divergent perceptions of asthma and how to manage it, and a mismatch between what patients want/need from these plans and what is provided by professionals are barriers to success. 41 , 42
What are the challenges for the healthcare organisation in providing self-management support?
A number of studies have demonstrated the challenges for primary care physicians in providing ongoing support for people with asthma. 31 , 48 , 49 In some countries, nurses and other allied health professionals have been trained as asthma educators and monitor people with stable asthma. These resources are not always available. In addition, some primary care services are delivered in constrained systems where only a few minutes are available to the practitioner in a consultation, or where only a limited range of asthma medicines are available or affordable. 50
There is recognition that the delivery of quality care depends on the competence of the doctor (and supporting health professionals), the relationship between the care providers and care recipients, and the quality of the environment in which care is delivered. 51 This includes societal expectations, health literacy and financial drivers.
In 2001, the Australian Government adopted a programme developed by the General Practitioner Asthma Group of the National Asthma Council Australia that provided a structured approach to the implementation of asthma management guidelines in a primary care setting. 52 Patients with moderate-to-severe asthma were eligible to participate. The 3+ visit plan required confirmation of asthma diagnosis, spirometry if appropriate, assessment of trigger factors, consideration of medication and patient self-management education including provision of a written PAAP. These elements, including regular medical review, were delivered over three visits. Evaluation demonstrated that the programme was beneficial but that it was difficult to complete the third visit in the programme. 53 – 55 Accordingly, the programme, renamed the Asthma Cycle of Care, was modified to incorporate two visits. 56 Financial incentives are provided to practices for each patient who receives this service each year.
Concurrently, other programmes were implemented which support practice-based care. Since 2002, the National Asthma Council has provided best-practice asthma and respiratory management education to health professionals, 57 and this programme will be continuing to 2017. The general practitioner and allied health professional trainers travel the country to provide asthma and COPD updates to groups of doctors, nurses and community pharmacists. A number of online modules are also provided. The PACE (Physician Asthma Care Education) programme developed by Noreen Clark has also been adapted to the Australian healthcare system. 58 In addition, a pharmacy-based intervention has been trialled and implemented. 59
To support these programmes, the National Asthma Council ( www.nationalasthma.org.au ) has developed resources for use in practices. A strong emphasis has been on the availability of a range of PAAPs (including plans for using adjustable maintenance dosing with ICS/LABA combination inhalers), plans for indigenous Australians, paediatric plans and plans translated into nine languages. PAAPs embedded in practice computer systems are readily available in consultations, and there are easily accessible online paediatric PAAPs ( http://digitalmedia.sahealth.sa.gov.au/public/asthma/ ). A software package, developed in the UK, can be downloaded and used to generate a pictorial PAAP within the consultation. 60
One of the strongest drivers towards the provision of written asthma action plans in Australia has been the Asthma Friendly Schools programme. 61 , 62 Established with Australian Government funding and the co-operation of Education Departments of each state, the Asthma Friendly Schools programme engages schools to address and satisfy a set of criteria that establishes an asthma-friendly environment. As part of accreditation, the school requires that each child with asthma should have a written PAAP prepared by their doctor to assist (trained) staff in managing a child with asthma at school.
The case study continues...
The initial presentation some weeks ago was during an exacerbation of asthma, which may not be the best time to educate a patient. It is, however, a splendid time to build on their motivation to feel better. She agreed to return after her asthma had settled to look more closely at her asthma control, and an appointment was made for a routine review.
At this follow-up consultation, the patient’s diagnosis was reviewed and confirmed and her trigger factors discussed. For this lady, respiratory tract infections are the usual trigger but allergic factors during times of high pollen count may also be relevant. Assessment of her nasal airway suggested that she would benefit from better control of allergic rhinitis. Other factors were discussed, as many patients are unaware that changes in air temperature, exercise and pets can also trigger asthma exacerbations. In addition, use of the Asthma Control Test was useful as an objective assessment of control as well as helping her realise what her life could be like! Many people with long-term asthma live their life within the constraints of their illness, accepting that is all that they can do.
After assessing the level of asthma control, a discussion about management options—trigger avoidance, exercise and medicines—led to the development of a written PAAP. Asthma can affect the whole family, and ways were explored that could help her family understand why it is important that she finds time in the busy domestic schedules to take her regular medication. Family and friends can also help by understanding what triggers her asthma so that they can avoid exposing her to perfumes, pollens or pets that risk triggering her symptoms. Information from the national patient organisation was provided to reinforce the messages.
The patient agreed to return in a couple of weeks, and a recall reminder was set up. At the second consultation, the level of control since the last visit will be explored including repeat spirometry, if appropriate. Further education about the pathophysiology of asthma and how to recognise early warning signs of loss of control can be given. Device use will be reassessed and the PAAP reviewed. Our patient’s goal is to avoid disruption to her work and her PAAP will focus on achieving that goal. Finally, agreement will be reached with the patient about future routine reviews, which, now that she has a written PAAP, could be scheduled by telephone if all is well, or face-to-face if a change in her clinical condition necessitates a more comprehensive review.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2012. Available from: http://www.ginasthma.org (accessed July 2013).
British Thoracic Society/Scottish Intercollegiate Guideline Network British Guideline on the Management of Asthma. Thorax 2008; 63 (Suppl 4 iv1–121, updated version available from: http://www.sign.ac.uk (accessed January 2014).
Article Google Scholar
National Asthma Council Australia. Australian Asthma Handbook. Available from: http://www.nationalasthma.org.au/handbook (accessed May 2014).
National Asthma Education and Prevention Program (NAEPP) Coordinating Committee. Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. Available from: https://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm (accessed May 2014).
Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke H . A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. (PRISMS Practical Systematic Review of Self-Management Support for long-term conditions). Health Serv Deliv Res (in press).
Gibson PG, Powell H, Wilson A, Abramson MJ, Haywood P, Bauman A et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No. CD001117.
Tapp S, Lasserson TJ, Rowe BH . Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007: (Issue 3) Art No. CD003000.
Powell H, Gibson PG . Options for self-management education for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No: CD004107.
Toelle B, Ram FSF . Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev 2004: (Issue 1) Art No. CD002171.
Lefevre F, Piper M, Weiss K, Mark D, Clark N, Aronson N . Do written action plans improve patient outcomes in asthma? An evidence-based analysis. J Fam Pract 2002; 51 : 842–848.
PubMed Google Scholar
Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M . Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009: (Issue 2) Art No.CD001290.
Bravata DM, Gienger AL, Holty JE, Sundaram V, Khazeni N, Wise PH et al. Quality improvement strategies for children with asthma: a systematic review. Arch Pediatr Adolesc Med 2009; 163 : 572–581.
Bower P, Murray E, Kennedy A, Newman S, Richardson G, Rogers A . Self-management support interventions to reduce health care utilisation without compromising outcomes: a rapid synthesis of the evidence. Available from: http://www.nets.nihr.ac.uk/projects/hsdr/11101406 (accessed April 2014).
Gibson PG, Powell H . Written action plans for asthma: an evidence-based review of the key components. Thorax 2004; 59 : 94–99.
Article CAS Google Scholar
Bhogal SK, Zemek RL, Ducharme F . Written action plans for asthma in children. Cochrane Database Syst Rev 2006: (Issue 3) Art No. CD005306.
Zemek RL, Bhogal SK, Ducharme FM . Systematic review of randomized controlled trials examining written action plans in children: what is the plan?. Arch Pediatr Adolesc Med 2008; 162 : 157–163.
Pinnock H, Slack R, Pagliari C, Price D, Sheikh A . Understanding the potential role of mobile phone based monitoring on asthma self-management: qualitative study. Clin Exp Allergy 2007; 37 : 794–802.
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R . Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012: (Issue 12) Art No. CD007459.
Huckvale K, Car M, Morrison C, Car J . Apps for asthma self-management: a systematic assessment of content and tools. BMC Med 2012; 10 : 144.
Allergic Rhinitis and its Impact on Asthma. Management of Allergic Rhinitis and its Impact on Asthma: Pocket Guide. ARIA 2008. Available from: http://www.whiar.org (accessed May 2014).
Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011; 85 : e131–e143.
Moullec G, Gour-Provencal G, Bacon SL, Campbell TS, Lavoie KL . Efficacy of interventions to improve adherence to inhaled corticosteroids in adult asthmatics: Impact of using components of the chronic care model. Respir Med 2012; 106 : 1211–1225.
Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D et al. Accessibility, acceptability and effectiveness of telephone reviews for asthma in primary care: randomised controlled trial. BMJ 2003; 326 : 477–479.
Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A . Accessibility, clinical effectiveness and practice costs of providing a telephone option for routine asthma reviews: phase IV controlled implementation study. Br J Gen Pract 2007; 57 : 714–722.
PubMed PubMed Central Google Scholar
Kielmann T, Huby G, Powell A, Sheikh A, Price D, Williams S et al. From support to boundary: a qualitative study of the border between self care and professional care. Patient Educ Couns 2010; 79 : 55–61.
Asthma UK . Compare your care report. Asthma UK, 2013. Available from: http://www.asthma.org.uk (accessed January 2014).
Stallberg B, Lisspers K, Hasselgren M, Janson C, Johansson G, Svardsudd K . Asthma control in primary care in Sweden: a comparison between 2001 and 2005. Prim Care Respir J 2009; 18 : 279–286.
Reddel H, Peters M, Everett P, Flood P, Sawyer S . Ownership of written asthma action plans in a large Australian survey. Eur Respir J 2013; 42 . Abstract 2011.
Wiener-Ogilvie S, Pinnock H, Huby G, Sheikh A, Partridge MR, Gillies J . Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J 2007; 16 : 369–377.
Kennedy A, Rogers A, Bower P . Support for self care for patients with chronic disease. BMJ 2007; 335 : 968–970.
Ring N, Malcolm C, Wyke S, Macgillivray S, Dixon D, Hoskins G et al. Promoting the Use of Personal Asthma Action Plans: A Systematic Review. Prim Care Respir J 2007; 16 : 271–283.
Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB et al. A new perspective on concepts of asthma severity and control. Eur Respir J 2008; 32 : 545–554.
Horne R . Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130 (suppl): 65S–72S.
Reddel HK, Taylor DR, Bateman ED, Boulet L-P, Boushey HA, Busse WW et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009; 180 : 59–99.
Thomas M, Kay S, Pike J, Rosenzweig JR, Hillyer EV, Price D . The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Prim Care Respir J 2009; 18 : 41–49.
Hoskins G, Williams B, Jackson C, Norman P, Donnan P . Assessing asthma control in UK primary care: use of routinely collected prospective observational consultation data to determine appropriateness of a variety of control assessment models. BMC Fam Pract 2011; 12 : 105.
Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshon J, Price D et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010; 19 : 75–83.
McKinstry B, Hammersley V, Burton C, Pinnock H, Elton RA, Dowell J et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010; 19 : 298–303.
Gordon C, Galloway T . Review of Findings on Chronic Disease Self-Management Program (CDSMP) Outcomes: Physical, Emotional & Health-Related Quality of Life, Healthcare Utilization and Costs . Centers for Disease Control and Prevention and National Council on Aging: Atlanta, GA, USA, 2008.
Beasley R, Crane J . Reducing asthma mortality with the self-management plan system of care. Am J Respir Crit Care Med 2001; 163 : 3–4.
Ring N, Jepson R, Pinnock H, Wilson C, Hoskins G, Sheikh A et al. Encouraging the promotion and use of asthma action plans: a cross study synthesis of qualitative and quantitative evidence. Trials 2012; 13 : 21.
Jones A, Pill R, Adams S . Qualitative study of views of health professionals and patients on guided self-management plans for asthma. BMJ 2000; 321 : 1507–1510.
Bandura A . Self-efficacy: toward a unifying theory of behavioural change. Psychol Rev 1977; 84 : 191–215.
Gollwitzer PM, Sheeran P . Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol 2006; 38 : 69–119.
Google Scholar
Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham NJ, Kinmonth AL . Application of the theory of planned behaviour change interventions: a systematic review. Psychol Health 2002; 17 : 123–158.
Schwarzer R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008; 57 : 1–29.
Sniehotta F . Towards a theory of intentional behaviour change: plans, planning, and self-regulation. Br J Health Psychol 2009; 14 : 261–273.
Okelo SO, Butz AM, Sharma R, Diette GB, Pitts SI, King TM et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics 2013; 132 : 517–534.
Grol R, Grimshaw RJ . From best evidence to best practice: effective implementation of change in patients care. Lancet 2003; 362 : 1225–1230.
Jusef L, Hsieh C-T, Abad L, Chaiyote W, Chin WS, Choi Y-J et al. Primary care challenges in treating paediatric asthma in the Asia-Pacific region. Prim Care Respir J 2013; 22 : 360–362.
Donabedian A . Evaluating the quality of medical care. Milbank Q 2005; 83 : 691–729.
Fardy HJ . Moving towards organized care of chronic disease. The 3+ visit plan. Aust Fam Physician 2001; 30 : 121–125.
CAS PubMed Google Scholar
Glasgow NJ, Ponsonby AL, Yates R, Beilby J, Dugdale P . Proactive asthma care in childhood: general practice based randomised controlled trial. BMJ 2003; 327 : 659.
Douglass JA, Goemann DP, Abramson MJ . Asthma 3+ visit plan: a qualitative evaluation. Intern Med J 2005; 35 : 457–462.
Beilby J, Holton C . Chronic disease management in Australia; evidence and policy mismatch, with asthma as an example. Chronic Illn 2005; 1 : 73–80.
The Department of Health. Asthma Cycle of Care. Accessed on 14 May 2014 at http://www.health.gov.au/internet/main/publishing.nsf/Content/asthma-cycle .
National Asthma Council Australia. Asthma and Respiratory Education Program. Accessed on 14 May 2014 at http://www.nationalasthma.org.au/health-professionals/education-training/asthma-respiratory-education-program .
Patel MR, Shah S, Cabana MD, Sawyer SM, Toelle B, Mellis C et al. Translation of an evidence-based asthma intervention: Physician Asthma Care Education (PACE) in the United States and Australia. Prim Care Respir J 2013; 22 : 29–34.
Armour C, Bosnic-Anticevich S, Brilliant M, Burton D, Emmerton L, Krass I et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax 2007; 62 : 496–502.
Roberts NJ, Mohamed Z, Wong PS, Johnson M, Loh LC, Partridge MR . The development and comprehensibility of a pictorial asthma action plan. Patient Educ Couns 2009; 74 : 12–18.
Henry RL, Gibson PG, Vimpani GV, Francis JL, Hazell J . Randomised controlled trial of a teacher-led asthma education program. Pediatr Pulmonol 2004; 38 : 434–442.
National Asthma Council Australia. Asthma Friendly Schools program. Accessed on 14 May 2014 at http://www.asthmaaustralia.org.au/Asthma-Friendly-Schools.aspx .
Download references
Author information
Authors and affiliations.
Asthma UK Centre for Applied Research, Centre for Population Health Sciences, The University of Edinburgh, Edinburgh, UK,
Hilary Pinnock & Elisabeth Ehrlich
NMAHP-RU, University of Stirling, Stirling, UK,
Gaylor Hoskins
Discipline of General Practice, University of Sydney, Sydney, NSW, Australia
Ron Tomlins
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hilary Pinnock .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
Reprints and permissions
About this article
Cite this article.
Pinnock, H., Ehrlich, E., Hoskins, G. et al. A woman with asthma: a whole systems approach to supporting self-management. npj Prim Care Resp Med 24 , 14063 (2014). https://doi.org/10.1038/npjpcrm.2014.63
Download citation
Received : 23 June 2014
Revised : 15 July 2014
Accepted : 15 July 2014
Published : 16 October 2014
DOI : https://doi.org/10.1038/npjpcrm.2014.63
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Case Report
- Open access
- Published: 16 December 2008
Bronchial carcinoid in a 39-year-old man treated for bronchial asthma: a case report
- Justyna Emeryk 1 ,
- Elżbieta Czekajska-Chehab 2 ,
- Elżbieta Korobowicz 1 ,
- Marta Korbel 3 ,
- Irena Węgrzyn-Szkutnik 1 &
- Janusz Milanowski 1
Cases Journal volume 2 , Article number: 7414 ( 2008 ) Cite this article
14k Accesses
3 Citations
Metrics details
A case study of 39-year old man with persistent wheezing, episodes of haemoptysis and dry cough unsuccessfully treated with inhaled beta2-agonists and steroids for about 10 months. Chest radiograph revealed a disproportion in dimensions between both lungs, with the left one being smaller than the right one. Spirometry demonstrated a restrictive pattern. During bronchoscopy, a polypoid endobronchial tumor, localized in the left main bronchus, completely occluding its lumen, was found. The tumor was diagnosed as carcinoid. In this case, due to the lack of characteristic symptoms, diagnosis of carcinoid was delayed. Patients unsuccessfully treated for bronchial asthma or chronic obstructive pulmonary disease should undergo bronchoscopic examination.
Case presentation
A 39-year-old white man, working as a house builder, was admitted to our pulmonary ward in August 2007 with an eleven-month history of persistent wheezing, heard not only during auscultation but also by patient himself. This wheezing had no correlation with physical exertion. He also reported a few episodes of haemoptysis within last 7 months and dry cough for about a month. Patient's weight was 81.5 kg, his height was 180 cm. Except from nodular goitre (in euthyreosis), the patient reported no other complaints or diseases in his medical history. His family history was not clinically significant. He had a 10 pack-years smoking history, until the age of 31 when he stopped smoking. He drank alcohol occasionally. His symptoms were unsuccessfully treated with inhaled β 2 -agonists and steroids for about 10 months. Apart from these medications, he took no other drugs. On auscultation, there were wheezes in upper fields of both lungs. The chest radiograph (figure 1 ) showed a disproportion in dimensions and vascular markings between both lungs- the left one was significantly smaller and had decreased vascular markings in comparison to the right one- these findings might be the expression of left lung hypoplasia. The heart silhouette was discretely displaced to the left side.

Chest radiograph performed at admission to the hospital .
Spirometry performed during hospitalization in our clinic showed a restrictive pattern (figure 2 ) with forced expiratory volume in one second (FEV 1 ) of 59% predicted and forced vital capacity (FVC) of 66% predicted. The FEV 1 /FVC ratio was 70% predicted.
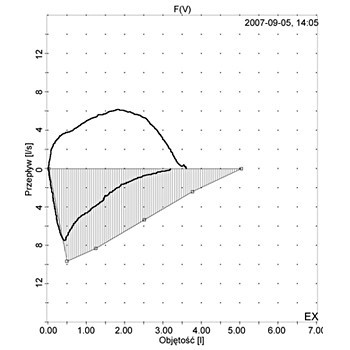
Flow-volume curve showing a restrictive pattern performed at admission to the hospital .
Bronchoscopy was performed, revealing a polypoid endobronchial tumor, localized in the left main bronchus (2 cm from tracheal bifurcation), completely occluding its lumen. The tumor was biopsied and the specimen was sent to histological examination which gave the diagnosis of bronchial carcinoid.
Thoracic computed tomography showed a polypoid mass in the left main bronchus with a diameter of about 20 mm. The tumor showed very high enhancement after contrast medium administration: from 9 HU (Hounsfield units) (figure 3a ) to 119 HU in arterial phase (figure 3b ) and 47 HU in parenchymal phase (figure 3c ), which is characteristic for carcinoid.
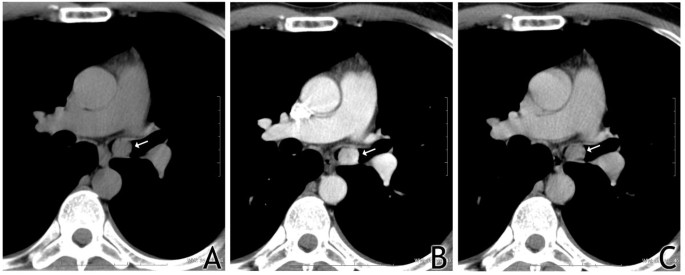
High enhancement of the tumor (arrow) after contrast medium administration: on the left- before administration of contrast medium, in the middle-after administration; arterial phase, on the right-parenchymal phase .
Hilar and mediastinal nodes were not enlarged. In virtual bronchoscopy, as well as in transparent reconstruction of the airways, a total occlusion of the left main bronchus by the tumor could be observed (Figure 4 and 5 ).
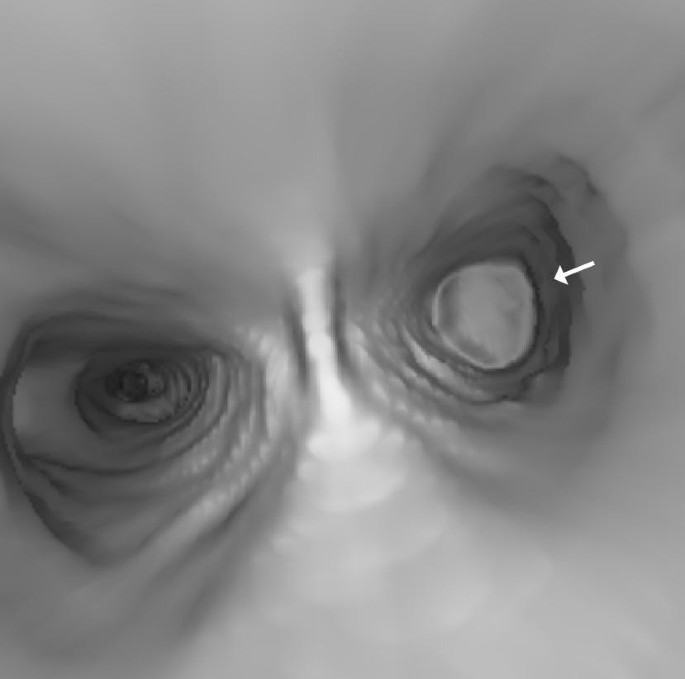
Total occlusion of the left main bronchus by the tumor (arrow) .
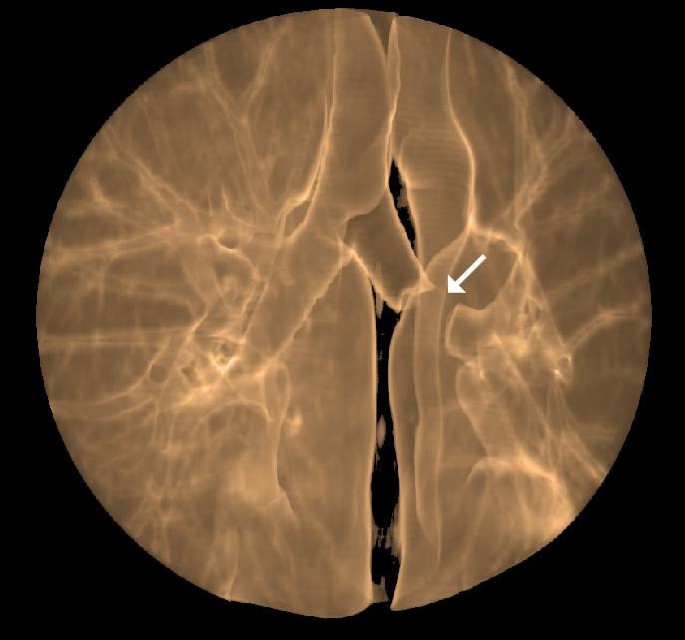
Amputation of the left main bronchus by the tumor (arrow) .
The patient was transferred to thoracic surgery ward for surgical treatment. He underwent left pulmonectomy and histopathological analysis of post-operative material confirmed the diagnosis of bronchial carcinoid. There were no complications during post-operative period and the patient was discharged from hospital 10 days after the operation. Then, the patient went abroad and was lost for follow-up until May 2008. On control visit in May, he was in very good condition, presenting no signs of pulmonary disease. On physical examination, except from diminished breath sounds and dullness to percussion over left lung (due to pulmonectomy and consequent pleural fluid accumulation) no abnormalities were found. In control computed tomography there were no signs of recurrence of the disease.
Pulmonary carcinoids comprise 1-2% of all lung tumors. They may develop in many locations in the body but most often, they are found in small intestine (26%), respiratory system (25%) and appendix (19%) [ 1 ].
Carcinoid tumors are classified as typical or atypical according to histopathological criteria. This division has a strict extrapolation to survival rates: in case of typical pulmonary carcinoids 5-year survival rate is over 90%, in atypical ones- it is within the range of 40-60% [ 2 ].
The following symptoms are observed most often in patients with carcinoid localized in respiratory system: haemoptysis, cough, recurrent pulmonary infections, fever, chest discomfort, unilateral wheezing and shortness of breath [ 3 ].
Due to the lack of characteristic symptoms, diagnosis of pulmonary carcinoid is delayed and patients are often misdiagnosed with asthma or chronic obstructive pulmonary disease. According to three studies, there is an average delay of, respectively, 19, 13 and 10 months from the first symptoms to the final diagnosis of carcinoid [ 4 – 6 ]. Although general prognosis for patients with this neoplasm is quite favorable, it is obvious that the earlier diagnosis is made, the chances for radical treatment increase.
As the majority of pulmonary carcinoids (70%) are located in the main or lobar bronchi [ 7 ], they are within the reach of a bronchoscope. According to British Thoracic Society, flexible bronchoscopy is a safe procedure and there are no controlled studies concerning the factors disqualifying a patient from it [ 8 ]. Bronchoscopy cannot replace computed tomography, these both procedures are complementary, but to be able to orientate the treatment and prognosis, we have to know the histopathological diagnosis and the specimens for examination can be easily and safely provided by bronchoscopy.
This case is a good example of misdiagnosis of the disease. Extended clinical diagnosis, including computed tomography and bronchoscopy, should be considered in all cases of bronchial asthma or chronic obstructive pulmonary disease which do not respond to standard treatment.
"Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal."
Lips CJM, Lentjes EGWM, Höppener JWM: The spectrum of carcinoid tumours and carcinoid syndromes. Ann Clin Biochem. 2003, 40: 612-27. 10.1258/000456303770367207.
Article PubMed Google Scholar
Kulke MH, Mayer RJ: Carcinoid tumours. N Engl J Med. 1999, 340: 858-68. 10.1056/NEJM199903183401107.
Article CAS PubMed Google Scholar
Zuetenhorst JM, Taal BG: Metastatic carcinoid tumours: a clinical review. Oncologist. 2005, 10: 123-31. 10.1634/theoncologist.10-2-123.
Garcia-Rio FJ, Talavera IG, Rubio BG, Prados C, Rodriguez P: Clinical study of 20 cases of bronchial carcinoid. An Med Interna. 1992, 9 (1): 9-13.
CAS PubMed Google Scholar
Blondal T, Grimelius L, Nou E, Wilander E, Aberg T: Argyrophil carcinoid tumours of the lung. Incidence, clinical study and follow-up of 46 patients. Chest. 1980, 78 (6): 840-4. 10.1378/chest.78.6.840.
Van Damme H, Layachi N, Hermans G, Dekoster G: Carcinoid tumors of the bronchi. Our experience of these during the last 10 years, with a review of the literature. Acta Chir Belg. 1989, 89 (3): 166-74.
Hage R, de la Rivière AB, Seldenrijk CA, Bosch van den JMM: Update in pulmonary carcinoid tumours: a review article. Ann Surg Oncol. 2003, 10: 697-704. 10.1245/ASO.2003.09.019.
British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001, 56 (suppl 1): 1-21.
Download references
Author information
Authors and affiliations.
Chair and Department of Pulmonology, Oncology and Allergology, Medical University of Lublin, Jaczewski Street 8, 20-950, Lublin, Poland
Justyna Emeryk, Elżbieta Korobowicz, Irena Węgrzyn-Szkutnik & Janusz Milanowski
First Department of Radiology, Medical University of Lublin, Jaczewski Street 8, 20-950, Lublin, Poland
Elżbieta Czekajska-Chehab
Chair and Department of Clinical Pathomorphology, Medical University of Lublin, Jaczewski Street 8, 20-950, Lublin, Poland
Marta Korbel
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Justyna Emeryk .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
JE performed acquisition of data, review of literature and wrote the paper. ECC performed computed tomography imagings and prepared virtual bronchoscopy reconstructions. EK performed histopathological examination of the tumour. MK was responsible for patient care, follow-up and data collection. IWS was responsible for patient care and drafting of paper. JM performed acquisition of data, revised the manuscript and provided general support as the head of department. All authors read and approved the final manuscript.
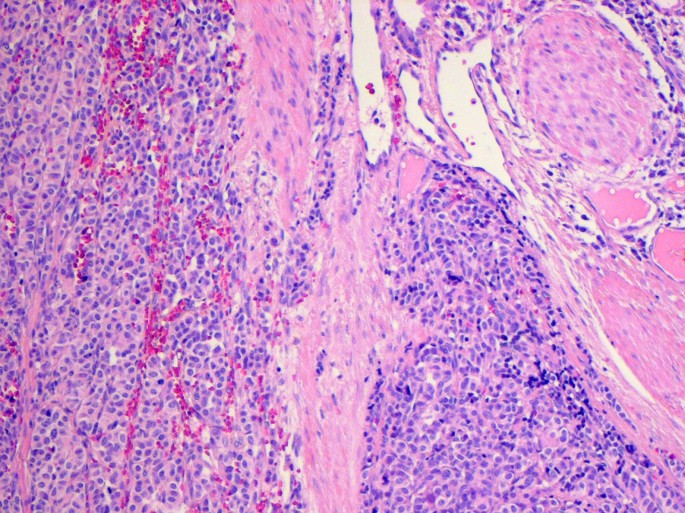
Microscopic imaging of bronchial carcinoid (hematoxylin and eosin staining) .
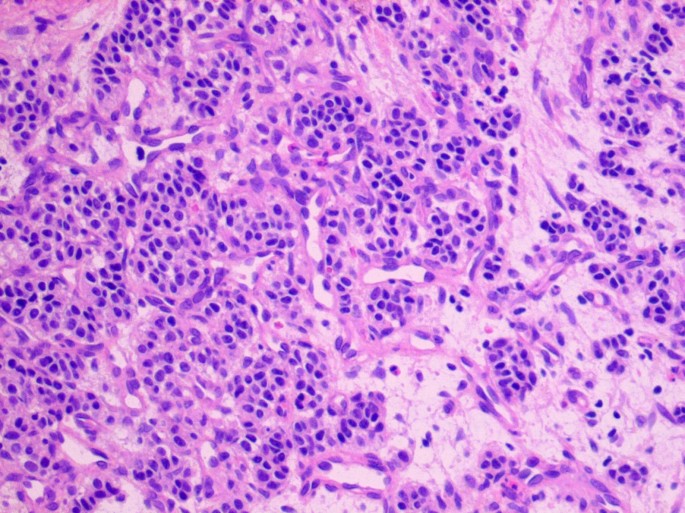
Immunohistochemical staining positive for chromogranine A .
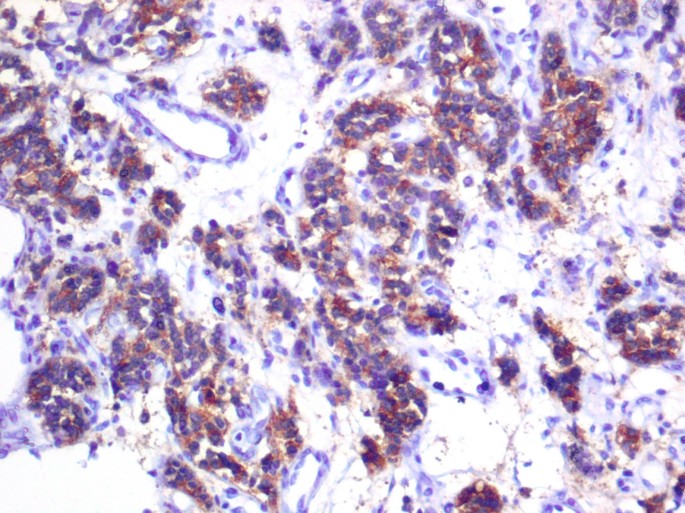
Immunohistochemical staining positive for synaptophysin .
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, authors’ original file for figure 7, authors’ original file for figure 8, authors’ original file for figure 9, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Emeryk, J., Czekajska-Chehab, E., Korobowicz, E. et al. Bronchial carcinoid in a 39-year-old man treated for bronchial asthma: a case report. Cases Journal 2 , 7414 (2008). https://doi.org/10.1186/1757-1626-2-7414
Download citation
Received : 19 November 2008
Accepted : 16 December 2008
Published : 16 December 2008
DOI : https://doi.org/10.1186/1757-1626-2-7414
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chronic Obstructive Pulmonary Disease
- Pleural Fluid
- Restrictive Pattern
- Left Main Bronchus
- British Thoracic Society
Cases Journal
ISSN: 1757-1626

Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Treatment of severe asthma: case report of fast action of mepolizumab in a patient with recent sars-cov-2 infection.

1. Introduction
1.1. covid-19 and pediatric asthma, 1.2. management and treatment of severe asthma, 2. materials and methods, 4. discussion, 5. conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Asthma Statistics|AAAAI [Internet]. Available online: https://www.aaaai.org/about/news/for-media/asthma-statistics (accessed on 25 July 2024).
- 2024 GINA Main Report—Global Initiative for Asthma—GINA [Internet]. Available online: https://ginasthma.org/2024-report/ (accessed on 25 July 2024).
- Senter, J.P.; Aisenberg, L.K.; Dudley, J.W.; Luan, X.; Huang, J.; Kenyon, C.C.; Hill, D.A. COVID-19 and Asthma Onset in Children. Pediatrics 2024 , 153 , e2023064615. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Jartti, T.; Gern, J.E. Role of viral infections in the development and exacerbation of asthma in children. J. Allergy Clin. Immunol. 2017 , 140 , 895–906. Available online: https://pubmed.ncbi.nlm.nih.gov/28987219/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Liu, L.; Pan, Y.; Zhu, Y.; Song, Y.; Su, X.; Yang, L.; Li, M. Association between rhinovirus wheezing illness and the development of childhood asthma: A meta-analysis. BMJ Open 2017 , 7 , e013034. Available online: https://pubmed.ncbi.nlm.nih.gov/28373249/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Corne, J.M.; Marshall, C.; Smith, S.; Schreiber, J.; Sanderson, G.; Holgate, S.T.; Johnston, S.L. Frequency, severity, and duration of rhinovirus infections in asthmatic and non-asthmatic individuals: A longitudinal cohort study. Lancet 2002 , 359 , 831–834. Available online: https://pubmed.ncbi.nlm.nih.gov/11897281/ (accessed on 25 July 2024). [ CrossRef ]
- Venkatesan, P. 2023 GINA report for asthma. Lancet Respir. Med. 2023 , 11 , 589. Available online: https://pubmed.ncbi.nlm.nih.gov/37302397/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Zhang, L.; Liu, H.; Ai, T.; Chen, Z.; Tang, W.; Hu, S.; Hu, J. Epidemiology of asthma exacerbation in children before and after the COVID-19 pandemic: A retrospective study in Chengdu, China. BMC Pediatr. 2023 , 23 , 588. Available online: https://pubmed.ncbi.nlm.nih.gov/37993873/ (accessed on 25 July 2024). [ CrossRef ]
- Chung, K.F.; Wenzel, S.E.; Brozek, J.L.; Bush, A.; Castro, M.; Sterk, P.J.; Adcock, I.M.; Bateman, E.D.; Bel, E.H.; Bleecker, E.R.; et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur. Respir. J. 2014 , 43 , 343–373. Available online: https://pubmed.ncbi.nlm.nih.gov/24337046/ (accessed on 25 July 2024). [ CrossRef ]
- Robbins, E.; Daoud, S.; Demissie, S.; James, P. The impact of asthma on COVID-19 disease severity in children and adolescents. J. Asthma 2023 , 60 , 1097–1103. Available online: https://pubmed.ncbi.nlm.nih.gov/36200730/ (accessed on 25 July 2024). [ CrossRef ]
- Cui, X.; Zhao, Z.; Zhang, T.; Guo, W.; Guo, W.; Zheng, J.; Zhang, J.; Dong, C.; Na, R.; Zheng, L.; et al. A systematic review and meta-analysis of children with coronavirus disease 2019 (COVID-19). J. Med. Virol. 2021 , 93 , 1057–1069. Available online: https://pubmed.ncbi.nlm.nih.gov/32761898/ (accessed on 25 July 2024). [ CrossRef ]
- Klain, A.; Indolfi, C.; Dinardo, G.; Decimo, F.; Miraglia Del Giudice, M. COVID-19 and spirometry in this age. Ital. J. Pediatr. 2022 , 48 , 11. Available online: https://ijponline.biomedcentral.com/articles/10.1186/s13052-022-01199-5 (accessed on 25 July 2024). [ CrossRef ]
- Indolfi, C.; Izzo, L.F.; Luciano, M.; Mercogliano, M.; Klain, A.; Dinardo, G.; Decimo, F.; Giudice, M.M. Impact of reduced COVID-19 restrictions on pediatric recurrent respiratory infections in Southern Italy: A cross-sectional analysis. Open Explor. 2024 , 2 , 340–349. Available online: https://www.explorationpub.com/Journals/eaa/Article/100949 (accessed on 25 July 2024). [ CrossRef ]
- Pellegrino, R.; Chiappini, E.; Licari, A.; Galli, L.; Marseglia, G.L. Prevalence and clinical presentation of long COVID in children: A systematic review. Eur. J. Pediatr. 2022 , 181 , 3995. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Esposito, S.; Principi, N.; Azzari, C.; Cardinale, F.; Di Mauro, G.; Galli, L.; Gattinara, G.C.; Fainardi, V.; Guarino, A.; Lancella, L.; et al. Italian intersociety consensus on management of long covid in children. Ital. J. Pediatr. 2022 , 48 , 42. Available online: https://pubmed.ncbi.nlm.nih.gov/35264214/ (accessed on 25 July 2024). [ CrossRef ]
- Parisi, G.F.; Diaferio, L.; Brindisi, G.; Indolfi, C.; Umano, G.R.; Klain, A.; Marchese, G.; Ghiglioni, D.G.; Zicari, A.M.; Marseglia, G.L.; et al. Cross-Sectional Survey on Long Term Sequelae of Pediatric COVID-19 among Italian Pediatricians. Children 2021 , 8 , 769. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Umano, G.R.; Rondinelli, G.; Rivetti, G.; Klain, A.; Aiello, F.; Miraglia del Giudice, M.; Decimo, F.; Papparella, A.; Miraglia del Giudice, E. Effect of COVID-19 Lockdown on Children’s Eating Behaviours: A Longitudinal Study. Children 2022 , 9 , 1078. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Rahman, N.H.A.; Mohd Zahir, M.Z.; Althabhawi, N.M. Repercussions of COVID-19 Lockdown on Implementation of Children’s Rights to Education. Children 2023 , 10 , 474. Available online: https://pubmed.ncbi.nlm.nih.gov/36980031/ (accessed on 25 July 2024). [ CrossRef ]
- Miraglia del Giudice, M.; Klain, A.; Dinardo, G.; D’Addio, E.; Bencivenga, C.L.; Fontanella, C.; Decimo, F.; Umano, G.R.; Siciliano, M.; Carotenuto, M.; et al. Behavioral and Sleep Disorders in Children and Adolescents following COVID-19 Disease: A Case-Control Study. Children 2023 , 10 , 1189. Available online: https://www.mdpi.com/2227-9067/10/7/1189/htm (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Zhang, J.; Dong, X.; Liu, G.; Gao, Y. Risk and Protective Factors for COVID-19 Morbidity, Severity, and Mortality. Clin. Rev. Allergy Immunol. 2022 , 64 , 90–107. Available online: https://link.springer.com/article/10.1007/s12016-022-08921-5 (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Brindisi, G.; Zicari, A.M.; Parisi, G.F.; Diaferio, L.; Indolfi, C.; Marchese, G.; Ghiglioni, D.G.; Umano, G.R.; Klain, A.; Marseglia, G.L.; et al. Prevalence of COVID-19 in children affected by allergic rhinoconjunctivitis and asthma: Results from the second “SIAIP rhinosinusitis and conjunctivitis committee” survey. Ital. J. Pediatr. 2022 , 48 , 1. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Graff, K.; Smith, C.; Silveira, L.; Jung, S.; Curran-Hays, S.; Jarjour, J.; Carpenter, L.; Pickard, K.; Mattiucci, M.; Fresia, J.; et al. Risk Factors for Severe COVID-19 in Children. Pediatr. Infect. Dis. J. 2021 , 40 , E137–E145. Available online: https://pubmed.ncbi.nlm.nih.gov/33538539/ (accessed on 25 July 2024). [ CrossRef ]
- Kara, A.A.; Böncüoğlu, E.; Kıymet, E.; Arıkan, K.; Şahinkaya, Ş.; Düzgöl, M.; Cem, E.; Çelebi, M.; Ağın, H.; Bayram, S.N.; et al. Evaluation of predictors of severe-moderate COVID-19 infections at children: A review of 292 children. J. Med. Virol. 2021 , 93 , 6634. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Mendes, N.F.; Jara, C.P.; Mansour, E.; Araújo, E.P.; Velloso, L.A. Asthma and COVID-19: A systematic review. Allergy Asthma Clin. Immunol. 2021 , 17 , 5. Available online: https://pubmed.ncbi.nlm.nih.gov/33407838/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Nazif, J.; Silver, E.; Okada, C.; Gross, E. Comparison of Children Hospitalized for Asthma Before and During the COVID-19 Pandemic. Pediatr. Allergy Immunol. Pulmonol. 2022 , 35 , 174–178. Available online: https://pubmed.ncbi.nlm.nih.gov/36537703/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Indolfi, C.; Klain, A.; Dinardo, G.; D’Addio, E.; Ferrara, S.; Decimo, F.; Ciprandi, G.; Tosca, M.A.; Miraglia del Giudice, M. COVID-19 Pediatric Follow-Up: Respiratory Long COVID-Associated Comorbidities and Lung Ultrasound Alterations in a Cohort of Italian Children. Children 2024 , 11 , 166. Available online: https://www.mdpi.com/2227-9067/11/2/166/htm (accessed on 25 July 2024). [ CrossRef ]
- Ahmed, H.; Turner, S. Severe asthma in children-a review of definitions, epidemiology, and treatment options in 2019. Pediatr Pulmonol 2019 , 54 , 778–787. Available online: https://pubmed.ncbi.nlm.nih.gov/30884194/ (accessed on 25 July 2024). [ CrossRef ]
- Ciprandi, G.; Cioffi, L.; Schiavetti, I.; del Giudice, M.M.; Tosca, M.A. Factors associated with wheezing recurrence in clinical practice. J. Asthma 2022 , 60 , 843–844. Available online: https://pubmed.ncbi.nlm.nih.gov/35666209/ (accessed on 25 July 2024). [ CrossRef ]
- Marseglia, G.L.; Manti, S.; Chiappini, E.; Brambilla, I.; Caffarelli, C.; Calvani, M.; Cardinale, F.; Cravidi, C.; Duse, M.; Martelli, A.; et al. Chronic cough in childhood: A systematic review for practical guidance by the Italian Society of Pediatric Allergy and Immunology. Allergol. Immunopathol. 2021 , 49 , 133–154. Available online: https://pubmed.ncbi.nlm.nih.gov/33641305/ (accessed on 25 July 2024). [ CrossRef ]
- Tozzi, A.E.; Armenio, L.; Bernardini, R.; Boner, A.; Calvani, M.; Cardinale, F.; Cavagni, G.; Dondi, A.; Duse, M.; Fiocchi, A.; et al. Pediatric allergy and immunology in Italy. Pediatr. Allergy Immunol. 2011 , 22 , 267–276. Available online: https://pubmed.ncbi.nlm.nih.gov/21457333/ (accessed on 25 July 2024). [ CrossRef ]
- Johnston, N.W.; Johnston, S.L.; Norman, G.R.; Dai, J.; Sears, M.R. The September epidemic of asthma hospitalization: School children as disease vectors. J. Allergy Clin. Immunol. 2006 , 117 , 557–562. [ Google Scholar ] [ CrossRef ]
- Garcia, G.; Taillé, C.; Laveneziana, P.; Bourdin, A.; Chanez, P.; Humbert, M. Anti-interleukin-5 therapy in severe asthma. Eur. Respir. Rev. 2013 , 22 , 251–257. Available online: https://pubmed.ncbi.nlm.nih.gov/23997052/ (accessed on 25 July 2024). [ CrossRef ]
- Ortega, H.G.; Liu, M.C.; Pavord, I.D.; Brusselle, G.G.; FitzGerald, J.M.; Chetta, A.; Humbert, M.; Katz, L.E.; Keene, O.N.; Yancey, S.W.; et al. Mepolizumab Treatment in Patients with Severe Eosinophilic Asthma. N. Engl. J. Med. 2014 , 371 , 1198–1207. Available online: https://www.nejm.org/doi/full/10.1056/nejmoa1403290 (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Chupp, G.L.; Bradford, E.S.; Albers, F.C.; Bratton, D.J.; Wang-Jairaj, J.; Nelsen, L.M.; Trevor, J.L.; Magnan, A.; Ten Brinke, A. Efficacy of mepolizumab add-on therapy on health-related quality of life and markers of asthma control in severe eosinophilic asthma (MUSCA): A randomised, double-blind, placebo-controlled, parallel-group, multicentre, phase 3b trial. Lancet Respir. Med. 2017 , 5 , 390–400. Available online: https://pubmed.ncbi.nlm.nih.gov/28395936/ (accessed on 25 July 2024). [ CrossRef ]
- Walsh, G.M. Anti-IL-5 monoclonal antibodies for the treatment of asthma: An update. Expert. Opin. Biol. Ther. 2020 , 20 , 1237–1244. Available online: https://pubmed.ncbi.nlm.nih.gov/32529893/ (accessed on 25 July 2024). [ CrossRef ]
- Ullmann, N.; Peri, F.; Florio, O.; Porcaro, F.; Profeti, E.; Onofri, A.; Cutrera, R. Severe Pediatric Asthma Therapy: Mepolizumab. Front. Pediatr. 2022 , 10 , 920066. Available online: https://pubmed.ncbi.nlm.nih.gov/35844748/ (accessed on 25 July 2024). [ CrossRef ]
- Bousquet, J.; Heinzerling, L.; Bachert, C.; Papadopoulos, N.G.; Bousquet, P.J.; Burney, P.G.; Canonica, G.W.; Carlsen, K.H.; Cox, L.; Haahtela, T.; et al. Practical guide to skin prick tests in allergy to aeroallergens. Allergy 2012 , 67 , 18–24. Available online: https://pubmed.ncbi.nlm.nih.gov/22050279/ (accessed on 25 July 2024). [ CrossRef ]
- Ansotegui, I.J.; Melioli, G.; Walter Canonica, G.; Caraballo, L.; Villa, E.; Ebisawa, M.; Passalacqua, G.; Savi, E.; Ebo, D.; Maximiliano Gómez, R.; et al. IgE allergy diagnostics and other relevant tests in allergy, a World Allergy Organization position paper. World Allergy Organ. J. 2020 , 13 , 100080. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Stanojevic, S.; Kaminsky, D.A.; Miller, M.R.; Thompson, B.; Aliverti, A.; Barjaktarevic, I.; Cooper, B.G.; Culver, B.; Derom, E.; Hall, G.L.; et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur. Respir. J. 2022 , 60 , 2101499. Available online: https://erj.ersjournals.com/content/60/1/2101499 (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Dinakar, C.; Chipps, B.E.; Matsui, E.C.; Abramson, S.L.; Irani, A.M.; Kim, J.S.; Mahr, T.A.; Pistiner, M.; Wang, J.; Katkin, J.P.; et al. Clinical tools to assess asthma control in children. Pediatrics 2017 , 139 , e20163438. Available online: https://pubmed.ncbi.nlm.nih.gov/28025241/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Agache, I.; Akdis, C.A.; Akdis, M.; Canonica, G.W.; Casale, T.; Chivato, T.; Corren, J.; Chu, D.K.; Del Giacco, S.; Eiwegger, T.; et al. EAACI Biologicals Guidelines—Recommendations for severe asthma. Allergy 2021 , 76 , 14–44. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/all.14425 (accessed on 25 July 2024). [ CrossRef ]
- Parisi, G.F.; Indolfi, C.; Decimo, F.; Leonardi, S.; Miraglia del Giudice, M. COVID-19 Pneumonia in Children: From Etiology to Management. Front. Pediatr. 2020 , 8 , 616622. Available online: https://pubmed.ncbi.nlm.nih.gov/33381482/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Cardinale, F.; Ciprandi, G.; Barberi, S.; Bernardini, R.; Caffarelli, C.; Calvani, M.; Cavagni, G.; Galli, E.; Minasi, D.; Del Giudice, M.M.; et al. Consensus statement of the Italian society of pediatric allergy and immunology for the pragmatic management of children and adolescents with allergic or immunological diseases during the COVID-19 pandemic. Ital. J. Pediatr. 2020 , 46 , 84. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ PubMed Central ]
- Diaferio, L.; Parisi, G.F.; Brindisi, G.; Indolfi, C.; Marchese, G.; Ghiglioni, D.G.; Zicari, A.M.; Marseglia, G.L.; Miraglia Del Giudice, M. Cross-sectional survey on impact of paediatric COVID-19 among Italian paediatricians: Report from the SIAIP rhino-sinusitis and conjunctivitis committee. Ital. J. Pediatr. 2020 , 46 , 146. Available online: https://ijponline.biomedcentral.com/articles/10.1186/s13052-020-00906-4 (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Aksu, K.; Demir, Ş.; Topel, M.; Yeşilkaya, S.; Ateş, H.; Koca Kalkan, İ.; Öncül, A.; Çuhadar Erçelebi, D.; Türkyilmaz, S. COVID-19 in patients with severe asthma using biological agents. Tuberk. Toraks 2021 , 69 , 433–436. Available online: https://pubmed.ncbi.nlm.nih.gov/34581170/ (accessed on 25 July 2024). [ CrossRef ] [ PubMed ]
- Azim, A.; Pini, L.; Khakwani, Z.; Kumar, S.; Howarth, P. Severe acute respiratory syndrome coronavirus 2 infection in those on mepolizumab therapy. Ann. Allergy Asthma Immunol. 2021 , 126 , 438–440. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Before Treatment with Mepolizumab | After 12 Weeks of Treatment with Mepolizumab | |
|---|---|---|
| C-ACT | 15 | 21 |
| ACQ-7 | 2, 28 | 1, 14 |
| FEV 1 L (%) | 1.07 (54) | 1.69 (83) |
| FEF 25% L/s (%) | 1.47 (36) | 3.02 (74) |
| FEF 50% L/s (%) | 0.85 (30) | 1.79 (62) |
| FEF 75% L/s (%) | 0.60 (41) | 0.90 (61) |
| FeNO | 19 | 3 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Indolfi, C.; Dinardo, G.; Klain, A.; Decimo, F.; Miraglia del Giudice, M. Treatment of Severe Asthma: Case Report of Fast Action of Mepolizumab in a Patient with Recent SARS-CoV-2 Infection. Life 2024 , 14 , 1063. https://doi.org/10.3390/life14091063
Indolfi C, Dinardo G, Klain A, Decimo F, Miraglia del Giudice M. Treatment of Severe Asthma: Case Report of Fast Action of Mepolizumab in a Patient with Recent SARS-CoV-2 Infection. Life . 2024; 14(9):1063. https://doi.org/10.3390/life14091063
Indolfi, Cristiana, Giulio Dinardo, Angela Klain, Fabio Decimo, and Michele Miraglia del Giudice. 2024. "Treatment of Severe Asthma: Case Report of Fast Action of Mepolizumab in a Patient with Recent SARS-CoV-2 Infection" Life 14, no. 9: 1063. https://doi.org/10.3390/life14091063
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.16(7); 2024 Jul
- PMC11329887

A Case Report of Central Bronchiectasis in a Poorly Controlled Asthmatic Adolescent With Allergic Bronchopulmonary Aspergillosis and Secondary Spontaneous Pneumothorax
Kasireddy sravanthi.
1 Pediatrics, Dr. D. Y. Patil Medical College, Hospital & Research Centre, Dr. D.Y. Patil Vidyapeeth, Pune, IND
Devika Jadhav
Sampada tambolkar, shailesh b meshram.
2 Respiratory Medicine, Dr. D. Y. Patil Medical College, Hospital & Research Centre, Dr. D.Y. Patil Vidyapeeth, Pune, IND
Manojkumar G Patil
Shailaja mane.
Allergic bronchopulmonary aspergillosis (ABPA) is a multifaceted immune hypersensitivity reaction occurring in the lungs and bronchi, triggered by exposure and colonization of Aspergillus species, commonly Aspergillus fumigatus (A. fumigatus) . It typically affects individuals who are immunocompetent but predisposed, such as those with bronchial asthma and cystic fibrosis. Diagnosis involves various methods including chest radiography, computed tomography, identification of eosinophilia, elevated serum IgE (immunoglobulin E) levels, and immunological tests for Aspergillus antigen. Left undiagnosed and untreated, ABPA can advance to bronchiectasis and/or pulmonary fibrosis, leading to significant morbidity and mortality.
Introduction
Aspergilli , a widespread type of fungi, consist of approximately 185 species, with A. fumigatus, Aspergillus niger , and Aspergillus flavus being the most prevalent ones known to cause diseases in humans. Among these, A. fumigatus predominantly contributes to cases of ABPA, a condition characterized by an inflammatory reaction to Aspergillus present in the mucus of individuals with underlying lung conditions such as persistent asthma and cystic fibrosis (CF). Various immune factors, such as atopy and specific immunogenic human leukocyte antigen (HLA) types in asthma patients, as well as genetic factors like mutations in the CF transmembrane conductance regulator (CFTR) gene in CF patients, elevate the susceptibility to ABPA in these populations [ 1 ].
ABPA manifests in around 1-2% of children with asthma and 2-15% of individuals with CF [ 2 ]. Establishing the prevalence of ABPA in asthmatics has proven problematic due to the absence of standardized diagnostic criteria. Consider ABPA in patients with chronic breathing difficulties (airway limitation) and a pre-existing lung condition like asthma or CF. A positive skin test result for Aspergillus , increased serum IgE (>417 IU/L), fungal-specific IgE and IgG antibodies, and imaging modalities are all part of the diagnostic workup for ABPA [ 1 ].
Case presentation
A 13-year-old male child presented to the outpatient department with complaints of fever, cough, and worsening asthma symptoms such as dyspnea and episodic wheezing for three years. His cough was productive, yellowish, and non-blood-stained. He was admitted with similar complaints in the past four times and was treated for pneumonia. His symptoms were relieved with treatment but didn’t improve completely. He was diagnosed with asthma at the age of eight years and progressed gradually over the past three years. He was managed with inhaled corticosteroids and short-acting beta-agonists. Spirometry showed significant bronchodilator reversibility of +23.23% and 240 ml.
On admission, the child was afebrile with a pulse of 102 beats per minute, respiration rate of 38 per minute, peripheral pulses well felt, oxygen saturation of 84% on room air and blood pressure of 100/72 mm Hg. Saturation improved to 91% on oxygen by mask. On general examination, mild cyanosis and clubbing were present. Auscultation of the chest revealed bilaterally equal air entry and bilateral crepitations with expiratory wheeze. The child was conscious and alert. Further physical examination demonstrated no other pathological findings. Family history was not significant. Routine laboratory investigations and chest X-rays were done as shown in Table Table1 1 and Figure Figure1 1 .
TLC: total leucocyte count; RBC: red blood cell; CRP: C-reactive protein
| Parameter (Reference Range) | Lab Value |
| Hemoglobin (12.8-16 g/dL) | 11 |
| TLC (4000-9100/µL) | 11,700 |
| Neutrophils (40-70%) | 60% |
| Eosinophils (1-6%) | 9% |
| Lymphocytes (20-40%) | 23% |
| Platelet count (150000-410000/µL) | 3,55,000 |
| Packed Cell Volume (37.3-47.7%) | 35.4 |
| RBC count (4.4-5.5 million/µL) | 5.08 |
| CRP (<2mg/L) | 11.1 |
| Erythrocyte sedimentation rate (Up to 15mm/hr) | 25 |
| Alanine aminotransferase (7-55 U/Lt) | 8 |
| Aspartate aminotransferase (8-60U/Lt) | 12 |
| Creatinine (0.35-0.86 mg/dl) | 0.63 |

Red arrow: gloved finger appearence
The child having experienced multiple episodes of pneumonia following asthma treatment combined with the clinical picture, tuberculosis infection was suspected. Given India's status as a developing nation with tuberculosis prevalence, a thorough tuberculosis workup was conducted, but laboratory and radiological findings ruled out the infection. A sweat chloride test was done to rule out CF which returned to be negative. Despite this, clinical and laboratory assessments pointed towards uncontrolled asthma as the likely diagnosis.
A high-resolution computed tomography was done, which revealed extensive areas of cystic, tubular and varicoid bronchiectasis with bronchial wall thickening of the subsegmental and segmental bronchi giving the finger-in-glove appearance in all the lobes of bilateral lungs with central distribution suggestive of ABPA, as shown in Figure Figure2 2 .

Red arrow: tubular bronchiectasis; yellow arrow: cystic bronchiectasis
Additionally, blood tests indicated peripheral eosinophilia with an absolute eosinophil count of 1053/ µL and significantly elevated serum total IgE 2428 IU/ml, positive blood test for Aspergillus specific IgE 49.6kUA/L and Aspergillus specific IgG 142 mgA/L, as listed in Table Table2. 2 . His blood culture was negative, but sputum culture tested positive for Pseudomonas aeruginosa.
IgE: Immunoglobulin E; IgG: immunoglobulin G
| Parameter (Reference Range) | Lab Value |
| Absolute Eosinophil count (0-500/ µL) | 1053 |
| Serum total IgE (100-200 IU/ml) | 2428 |
| specific IgE (<0.1 kUA/L) | 49.6 |
| specific IgG (>30 mgA/L) | 142 |
Despite proper management, the child did not improve. On day-3 of admission, repeat chest radiography and computed tomography (CT) were done in view of no clinical improvement, which showed left-sided moderate pneumothorax as shown in Figure Figure3, 3 , and a characteristic signet ring sign was seen as shown in Figure Figure4. 4 . Pneumothorax was managed by inserting an intercostal tube as shown in Figure Figure5. The 5 . The child's condition improved significantly, and after confirming lung re-expansion on chest X-ray, the chest tube was safely removed after seven days. After stabilizing the patient, a bronchoscopy procedure was performed revealing mucus plugs in the airways, which were cleared and sent for investigation. Bronchoalveolar lavage (BAL) for malignant cytology and CBNAAT (Cartridge-Based Nucleic Acid Amplification Test) tested negative. KOH mount of BAL showed branched septate hyphae and spores. This finding further supported the diagnosis of ABPA.

Red arrow: pneumothorax

Red arrow: signet ring sign

Red arrow: intercostal tube
The child was given Prednisolone at 0.5mg/kg/day for two weeks followed by 0.5mg/kg on alternate days for the next four weeks, slowly tapered and stopped over four months. Itraconazole 200mg/day was given for 16 weeks. After regular evaluations (every month), the exacerbations became less frequent, and the need for follow-up was reduced. He showed significant improvement in his health and consistently managed his daily routine after six months.
ABPA is characterized by a complex interplay of immune responses to A. fumigatus. Although the precise pathophysiology is yet unknown, a number of immunological responses are seen, such as abnormal T-lymphocyte responses and A. fumigatus-specific IgE-mediated type-1 and type-3 hypersensitivity. Upon inhalation, A. fumigatus spores germinate into hyphae within the bronchi, releasing diverse proteins and toxins that trigger inflammatory responses. Individuals with asthma and CF who develop ABPA often exhibit genetic susceptibility factors. For instance, the absence of HLA-DQ2 and the presence of HLA-DR2 and/or HLA-DR5 increase the risk of ABPA upon exposure to Aspergillus . Conversely, the presence of HLA-DQ2 is believed to confer a protective effect against ABPA [ 3 , 4 ].
The diagnosis of ABPA is a challenging task because of the overlap in both clinical and radiographic symptoms. A mix of clinical examination, laboratory studies, and radiographic results is used to make the diagnosis, as shown in Tables Tables3, 3 , ,4 4 .
* Inner 2/3rd of chest CT field; AF: Aspergillus fumigatus ; ABPA: allergic bronchopulmonary aspergillosis; IgE: immunoglobulin E; IgG: immunoglobulin G
| Criteria | ABPA Central Bronchiectasis | ABPA-Seropositive |
| Essential Criteria | Asthma Central bronchiectasis* Immediate skin sensitivity to species or AF | Asthma Immediate skin sensitivity to species or AF Total serum IgE conc. > 417 kU/L (1000 ng/mL) Elevated serum IgE and/or IgG-AF |
| Non-essential Criteria | Chest X-ray infiltrates Serum precipitating antibodies to AF | Chest X-ray infiltrates |
AF: Aspergillus fumigatus , Total IgE (Immunoglobulin E): 1 kU/L=2.4 ng/mL, 1 kU/L=1 IU/ml, *Transient (nodules, consolidation, tram‑track sign, fleeting opacities, finger in glove/toothpaste opacities) or fixed (ring shadows, bronchiectasis, or fibrosis); ABPA: allergic bronchopulmonary aspergillosis, CF: cystic fibrosis, CT: computerized tomography
| Rosenberg‑Patterson Criteria 1977 [ ] | Greenberger Criteria 2002 [ ] | Agarwal et al. 2013 [ ] | Agarwal et al. 2016 [ ] | |
| ABPA very likely if the first 6 of 7 primary fulfilled. ABPA certain if all primary 7 present | ABPA‑central bronchiectasis | ABPA‑seropositive | ABPA is diagnosed if all of following criteria are met | ABPA is diagnosed if all of the following criteria are met |
| Primary | Essential criteria | Essential criteria | ||
| 1. Asthma | 1. Asthma | 1. Asthma | 1. Predisposing condition‑Asthma or cystic fibrosis | 1. Predisposing condition‑Asthma or cystic fibrosis, COPD, post‑TB fibrocavitary disease |
| 2. Peripheral blood eosinophilia (>1.0×109/L) | 2. Immediate skin sensitivity to species or AF | 2. Immediate skin sensitivity to species or AF | 2. Obligatory criteria 1‑Immediate skin sensitivity to or increased IgE against AF (>0.35 kUA/L) | 2. Obligatory criteria 1‑Increased IgE against AF (>0.35 kUA/L) If this not available, Immediate skin sensitivity to AF may be considered |
| 3. Immediate cutaneous reactivity to antigen | 3. Elevated serum IgE and/or IgG against AF | 3. Elevated serum IgE and/or IgG against AF | 3. Obligatory criteria 2‑ Total serum IgE >1000 IU/ml (2400 ng/mL) | 3. Obligatory criteria 2‑ Total serum IgE>1000 IU/ml (2400 ng/mL) |
| 4. Precipitating antibodies against antigen | 4. Total serum IgE conc. ( >417 kU/L or >1000 ng/mL) | 4. Total serum IgE concentration > 417 kU/L (1000 ng/mL) | ||
| 5. Elevated total serum IgE (>1000 ng/mL) | 5. Central bronchiectasis | |||
| 6. Chest X‑ray infiltrates (transient or fixed) | ||||
| 7. Central bronchiectasis | ||||
| Secondary | Non-essential criteria | 4. Other criteria: At least 2 of three | 4. Other criteria: At least 2 of three | |
| 1. in sputum (by culture or microscopy) | 1. Chest X‑ray infiltrates | 1. Chest X‑ray infiltrates | 1. Radiographic findings consistent with ABPA* | 1. Radiographic findings consistent with ABPA* |
| 2. History of brown plugs in sputum | 2. Serum precipitating antibodies to AF | 2. Serum precipitating or IgG antibodies to AF | 2. Serum IgG >27 mgA/L against AF | |
| 3. Late (Arthus) skin reaction to antigen | 3. Increased total Eosinophils (>500) may be historical | 3. Increased total Eosinophils (>500) may be historical | ||
| 4. Increased total eosinophils (>500) may be historical | ||||
ABPA should be considered in asthmatic patients exhibiting certain indicators. These include new or recent infiltrates on lung imaging, suggestive of pneumonia or tuberculosis, alongside clinical and laboratory evidence of asthma that remains uncontrolled despite appropriate treatment. Additionally, ABPA may be suspected in cases of unresolved pneumonia and bronchiectasis, regardless of asthma history. The potential differentials for ABPA encompass uncontrolled asthma, tuberculosis, pneumonia, foreign body inhalation, immotile cilia syndrome, pulmonary infiltrates with eosinophilia, cystic fibrosis without ABPA, and sarcoidosis [ 3 ].
Managing ABPA requires a dual strategy that involves both controlling the immune response to alleviate symptoms and prevent immune-related complications and reducing the organism's burden to minimize the host's exposure to the triggering stimulus [ 9 ]. The 2016 guidelines by the Infectious Diseases Society of America recommend oral corticosteroids to reduce inflammation in ABPA, with inhaled corticosteroids for asthma control in affected individuals [ 10 ]. For symptomatic patients, those with CF and low FEV1, or those with ABPA complicated by mucoid impaction, bronchiectasis, or chronic pulmonary aspergillosis, itraconazole is the first-line antifungal treatment [ 9 ].
The primary treatment approach for ABPA typically involves systemic glucocorticoids, supplemented by antifungal medications and anti-IgE therapy such as omalizumab. During exacerbations in stages 1 and 3, glucocorticoids are administered at a dose of 0.5-1mg/kg for 14 days, followed by a tapering regimen over three to six months, or longer if necessary, with alternate-day usage. Stage 2, characterized by remission, and stage 5, where fibrosis has developed, generally do not necessitate glucocorticoid therapy. Stage 4 signifies a scenario where attempts to taper glucocorticoids have failed, prompting the need for continued long-term therapy [ 11 ].
During exacerbations of ABPA, antifungal therapy using a 16-week course of itraconazole has shown efficacy in improving treatment response. This allows for a reduction in glucocorticoid dosage by 50%, along with a decrease in total serum IgE levels by 25% or more. In children, the recommended dose is 5 mg/kg/day administered in a single dose. If the calculated dose exceeds 200mg, it should be divided equally and given twice daily. However, caution is necessary, as a typical dosage regimen of 7mg/kg/day in children may lead to hepatotoxicity, necessitating close monitoring of liver function [ 11 ].
Antifungal therapy helps decrease the fungal burden, antigenic stimulus, and inflammatory response, thereby reducing the need for systemic corticosteroids [ 12 ]. Azole antifungals, like itraconazole, are usually administered at 200 mg twice daily for 16 weeks [ 13 ]. The combination of itraconazole and prednisolone has been shown to significantly lower the one-year exacerbation rate compared to the use of either drug alone [ 12 ].
Conclusions
While ABPA in bronchial asthma is relatively uncommon, it should be considered in the list of potential causes of uncontrolled or difficult-to-treat asthma. Early identification before irreversible lung damage occurs is crucial for a favorable prognosis, emphasizing the importance of prompt treatment. Monitoring radiological findings and IgE levels is essential as clinical features alone may not reliably indicate ABPA progression or remission. Therefore, a comprehensive approach that includes vigilant observation of both imaging and immunological markers is necessary for effective management of ABPA in asthma patients.
Disclosures
Human subjects: Consent was obtained or waived by all participants in this study.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Kasireddy Sravanthi
Acquisition, analysis, or interpretation of data: Kasireddy Sravanthi, Devika Jadhav, Sampada Tambolkar, Shailesh B. Meshram, Shailaja Mane, Manojkumar G. Patil
Drafting of the manuscript: Kasireddy Sravanthi
Critical review of the manuscript for important intellectual content: Kasireddy Sravanthi, Devika Jadhav, Sampada Tambolkar, Shailesh B. Meshram, Shailaja Mane, Manojkumar G. Patil
Supervision: Devika Jadhav, Sampada Tambolkar, Shailesh B. Meshram, Shailaja Mane, Manojkumar G. Patil
Asthma as a risk factor and allergic rhinitis as a protective factor for COVID-19 severity: a case-control study
- Miscellaneous
- Published: 24 August 2024
Cite this article

- Martha Débora Lira Tenório 1 , 2 ,
- Gabriel Valentim dos Santos Menezes Siqueira 3 ,
- Gustavo Costa Caldas 3 ,
- Roque Pacheco de Almeida 1 , 3 ,
- Amélia Ribeiro de Jesus 1 , 3 &
- Paulo Ricardo Martins-Filho ORCID: orcid.org/0000-0001-8779-0727 1 , 2 , 4
92 Accesses
3 Altmetric
Explore all metrics
The COVID-19 pandemic has resulted in significant global morbidity and mortality. The disease presents a broad clinical spectrum, significantly influenced by underlying comorbidities. While certain conditions are known to exacerbate COVID-19 outcomes, the role of chronic inflammatory airway diseases such as asthma and rhinitis in influencing disease severity remains controversial. This study investigates the association between asthma and allergic rhinitis and the severity of COVID-19 outcomes in a specific geographical region prior to widespread vaccine deployment.
We conducted a case-control study with unvaccinated adult patients who had laboratory-confirmed COVID-19 by polymerase chain reaction (PCR). Cases were defined as severe or critical COVID-19 patients requiring intensive care unit (ICU) admission, and controls were non-severe patients without signs of viral pneumonia or hypoxia. We utilized the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire to assess the presence of asthma and allergic rhinitis. The association between these chronic inflammatory airway diseases and the severity of COVID-19 was evaluated using multivariate logistic regression analysis.
A total of 122 patients were analyzed, with 61 in each group. The presence of asthma (9 patients) was associated with an increased likelihood of severe COVID-19 (OR = 13.0; 95% CI 1.27-133.74), while rhinitis (39 patients) was associated with a protective effect against severe outcomes (OR = 0.36; 95% CI 0.13–0.99). No significant association was found between the frequency of asthmatic episodes or the severity of rhinitis and the severity of COVID-19 outcomes.
This study underscores the divergent effects of chronic inflammatory airway diseases on COVID-19 severity, with asthma associated with a higher likelihood of severe outcomes and rhinitis potentially offering protective effects. These findings enhance our understanding of the complex interactions between respiratory allergies and COVID-19, emphasizing the importance of targeted clinical management and public health strategies.
Key message
• Asthma increases the likelihood of severe COVID-19 outcomes.
• Allergic rhinitis may provide protection against severe COVID-19.
• Comorbidities strongly influence COVID-19 severity.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others

Prognosis of COVID-19 in respiratory allergy: a systematic review and meta-analysis

How does allergic rhinitis impact the severity of COVID-19?: a case–control study

The association between COVID-19 vaccine/infection and new-onset asthma in children - based on the global TriNetX database
Data availability.
The data supporting this study’s findings are available from the corresponding author, upon reasonable request.
Yang JM, Koh HY, Moon SY et al (2020) Allergic disorders and susceptibility to and severity of COVID-19: a nationwide cohort study. J Allergy Clin Immunol 146:790–798. https://doi.org/10.1016/j.jaci.2020.08.008
Article CAS PubMed PubMed Central Google Scholar
Gao Y, Ding M, Dong X et al (2021) Risk factors for severe and critically ill COVID-19 patients: a review. Allergy 76:428–455. https://doi.org/10.1111/all.14657
Article CAS PubMed Google Scholar
Gasmi A, Peana M, Pivina L et al (2021) Interrelations between COVID-19 and other disorders. Clin Immunol 224:108651. https://doi.org/10.1016/j.clim.2020.108651
Martins-Filho PR, Araújo AAS, Góes MAO et al (2021) COVID-19 mortality and case-fatality rates in Sergipe State, Northeast Brazil, from April to June 2020. Front Public Heal 9:581618. https://doi.org/10.3389/fpubh.2021.581618
Article Google Scholar
Martins-Filho PR, Antunes de Souza Araújo A, Pereira LX et al (2021) Factors Associated with mortality among hospitalized patients with COVID-19: a retrospective cohort study. Am J Trop Med Hyg 104:103–105. https://doi.org/10.4269/ajtmh.20-1170
Zhang J, Dong X, Liu G, Gao Y (2022) Risk and protective factors for COVID-19 morbidity, severity, and Mortality. Clin Rev Allergy Immunol 64:90–107. https://doi.org/10.1007/s12016-022-08921-5
Guvey A (2021) How does allergic rhinitis impact the severity of COVID-19? A case–control study. Eur Arch Oto-Rhino-Laryngology 278:4367–4371. https://doi.org/10.1007/s00405-021-06836-z
Shi W, Gao Z, Ding Y et al (2020) Clinical characteristics of COVID-19 patients combined with allergy. Allergy 75:2405–2408. https://doi.org/10.1111/all.14434
Jiao L, Bujnowski D, Liu P et al (2024) Asthma and clinical outcomes of COVID-19 in a community setting. Public Health 226:84–90. https://doi.org/10.1016/j.puhe.2023.10.040
Zhu Z, Hasegawa K, Ma B et al (2020) Association of Asthma and its genetic predisposition with the risk of severe COVID-19. J Allergy Clin Immunol 146:327–329e4. https://doi.org/10.1016/j.jaci.2020.06.001
Wang Y, Ao G, Qi X, Xie B (2020) The association between COVID-19 and asthma: a systematic review and meta‐analysis. Clin Exp Allergy 50:1274–1277. https://doi.org/10.1111/cea.13733
Kimura H, Francisco D, Conway M et al (2020) Type 2 inflammation modulates ACE2 and TMPRSS2 in airway epithelial cells. J Allergy Clin Immunol 146:80–88e8. https://doi.org/10.1016/j.jaci.2020.05.004
Yao Y, Wang H, Liu Z (2020) Expression of ACE2 in airways: implication for COVID-19 risk and disease management in patients with chronic inflammatory respiratory diseases. Clin Exp Allergy 50:1313–1324. https://doi.org/10.1111/cea.13746
von Elm E, Altman DG, Egger M et al (2007) The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Martins-Filho PR, de Souza Araújo AA, Quintans-Júnior LJ et al (2022) Dynamics of hospitalizations and in-hospital deaths from COVID-19 in northeast Brazil: a retrospective analysis based on the circulation of SARS-CoV-2 variants and vaccination coverage. Epidemiol Health 44:e2022036. https://doi.org/10.4178/epih.e2022036
Marshall JC, Murthy S, Diaz J et al (2020) A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect Dis 20:e192–e197. https://doi.org/10.1016/S1473-3099(20)30483-7
Article CAS Google Scholar
Asher M, Keil U, Anderson H et al (1995) International Study of Asthma and allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 8:483–491. https://doi.org/10.1183/09031936.95.08030483
Solé D, Vanna AT, Yamada E et al (1998) International Study of Asthma and allergies in Childhood (ISAAC) written questionnaire: validation of the asthma component among Brazilian children. J Investig Allergol Clin Immunol 8:376–382
PubMed Google Scholar
Solé D, Wandalsen GF, Camelo-Nunes IC et al (2006) Prevalence of symptoms of asthma, rhinitis, and atopic eczema among Brazilian children and adolescents identified by the International Study of Asthma and allergies in Childhood (ISAAC) - phase 3. J Pediatr (Rio J) 82:341–346. https://doi.org/10.2223/JPED.1521
Article PubMed Google Scholar
Oliveira TB, Persigo ALK, Ferrazza CC et al (2020) Prevalence of asthma, allergic rhinitis and pollinosis in a city of Brazil: a monitoring study. Allergol Immunopathol (Madr) 48:537–544. https://doi.org/10.1016/j.aller.2020.03.010
Urrutia-Pereira M, Chong-Neto H, Mocellin LP et al (2021) Prevalence of asthma symptoms and associated factors in adolescents and adults in southern Brazil: A Global Asthma Network Phase I study. World Allergy Organ J 14:100529. https://doi.org/10.1016/j.waojou.2021.100529
Article PubMed PubMed Central Google Scholar
Barbarot S, Auziere S, Gadkari A et al (2018) Epidemiology of atopic dermatitis in adults: results from an international survey. Allergy 73:1284–1293. https://doi.org/10.1111/all.13401
Peñaranda A, Pérez-Herrera LC, Gantiva M et al (2023) Factors associated with allergic rhinitis and combined allergic rhinitis and asthma syndrome (CARAS) in adults undergoing immunotherapy in a tropical country: is ISAAC-III questionnaire useful in adult populations? Allergol Immunopathol (Madr) 51:78–86. https://doi.org/10.15586/aei.v51i4.833
Hoffmann M, Kleine-Weber H, Schroeder S et al (2020) SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181:271–280e8. https://doi.org/10.1016/j.cell.2020.02.052
Matsumoto K, Saito H (2020) Does asthma affect morbidity or severity of COVID-19? J Allergy Clin Immunol 146:55–57. https://doi.org/10.1016/j.jaci.2020.05.017
Ren J, Pang W, Luo Y et al (2022) Impact of allergic Rhinitis and Asthma on COVID-19 infection, hospitalization, and Mortality. J Allergy Clin Immunol Pract 10:124–133. https://doi.org/10.1016/j.jaip.2021.10.049
Ziegler CGK, Allon SJ, Nyquist SK et al (2020) SARS-CoV-2 receptor ACE2 is an Interferon-stimulated gene in human airway epithelial cells and is detected in specific cell subsets across tissues. Cell 181:1016–1035e19. https://doi.org/10.1016/j.cell.2020.04.035
Grifoni A, Weiskopf D, Ramirez SI et al (2020) Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell 181:1489–1501e15. https://doi.org/10.1016/j.cell.2020.05.015
Skevaki C, Karsonova A, Karaulov A et al (2020) Asthma-associated risk for COVID-19 development. J Allergy Clin Immunol 146:1295–1301. https://doi.org/10.1016/j.jaci.2020.09.017
Samitas K, Carter A, Kariyawasam HH, Xanthou G (2018) Upper and lower airway remodelling mechanisms in asthma, allergic rhinitis and chronic rhinosinusitis: the one airway concept revisited. Allergy 73:993–1002. https://doi.org/10.1111/all.13373
Chen C, Song X, Murdock DJ et al (2024) Association between allergic conditions and COVID-19 susceptibility and outcomes. Ann Allergy Asthma Immunol 132:637–645e7. https://doi.org/10.1016/j.anai.2024.01.011
Valle SOR, Kuschnir FC, Solé D et al (2012) Validity and reproducibility of the Asthma Core International Study of Asthma and allergies in Childhood (ISAAC) Written Questionnaire obtained by Telephone Survey. J Asthma 49:390–394. https://doi.org/10.3109/02770903.2012.669440
Download references
Acknowledgements
PRMF is a research productivity fellow at the National Council for Scientific and Technological Development (CNPq), Brazil.
This study did not receive financial support.
Author information
Authors and affiliations.
Graduate Program in Health Sciences, Federal University of Sergipe, Aracaju, SE, Brazil
Martha Débora Lira Tenório, Roque Pacheco de Almeida, Amélia Ribeiro de Jesus & Paulo Ricardo Martins-Filho
Investigative Pathology Laboratory, Federal University of Sergipe, Aracaju, SE, Brazil
Martha Débora Lira Tenório & Paulo Ricardo Martins-Filho
Department of Medicine, Federal University of Sergipe, Aracaju, SE, Brazil
Gabriel Valentim dos Santos Menezes Siqueira, Gustavo Costa Caldas, Roque Pacheco de Almeida & Amélia Ribeiro de Jesus
Hospital Universitário, Laboratório de Patologia Investigativa, Universidade Federal de Sergipe, Rua Cláudio Batista, s/n. Sanatório, Aracaju, CEP: 49060-100, Sergipe, Brasil
Paulo Ricardo Martins-Filho
You can also search for this author in PubMed Google Scholar
Contributions
MDLT contributed to the conception, study design, data collection, data analysis, interpretation, writing of the manuscript, and manuscript revisions. GVSMS and GCC contributed to the data collection, interpretation, and manuscript revisions. RPA and ARJ contributed to the conception, study design, interpretation, and manuscript revisions. PRMF contributed to the study design, data collection, data analysis, interpretation, writing of the manuscript, and manuscript revisions. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Paulo Ricardo Martins-Filho .
Ethics declarations
Conflict of interest.
The authors have no conflict of interest to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Lira Tenório, M., dos Santos Menezes Siqueira, G., Costa Caldas, G. et al. Asthma as a risk factor and allergic rhinitis as a protective factor for COVID-19 severity: a case-control study. Eur Arch Otorhinolaryngol (2024). https://doi.org/10.1007/s00405-024-08893-6
Download citation
Received : 27 May 2024
Accepted : 03 August 2024
Published : 24 August 2024
DOI : https://doi.org/10.1007/s00405-024-08893-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
On examination, the temperature was 37.9°C, the blood pressure 157/95 mm Hg, the pulse 112 beats per minute, the respiratory rate 30 breaths per minute, and the oxygen saturation 91% while the ...
CASE PRESENTATION: A 58 years old Caucasian male, non smoker, with late onset allergic asthma was referred to our pulmonary rehabilitation clinic because of deconditioning, wheezing and recurrent asthma exacerbations despite treatment with budesonide-formoterol 200/6 mcg b.i.d., montelukast 10 mg q.i.d. He had daily complaints of dyspnea both at rest and on exertion using almost 200 ...
Clinical presentation (recurrent, episodic attacks of wheezing, cough, dyspnea, itchy red eyes, nasal discharge, stuffiness, and chest tightness), and PFT findings (FEV1/FVC of 0.65, FEV1 is 60% of predictive and post-bronchodilator therapy the FEV1 increases to 74% of predictive) are consistent with the diagnosis of asthma.
A 48-year-old female patient with uncontrolled severe asthma was referred to our hospital for anti-IgE therapy. She was suffering with persistent wheezing and dyspnea after a severe asthma attack that had taken place 5 months previously. Her asthma had not been controlled with adequate asthma treatment, including budesonide at 320 μg ...
To The Editor, The Global Initiative for Asthma (GINA) 2021 update was published on the 28th of April, 2021. [1]. There are significant changes, including treatment of mild asthma, the role of ...
MANAGEMENT OF A CASE OF UNCONTROLLED BRONCHIAL ASTHMA. INTRODUCTION: poor asthma control.1 Our case reports an undiagnosed comorbid depression as cause of persistent uncontrolled asthma. A 58 years old Caucasian male, non smoker, with late onset allergic asthma was referred to our CASE PRESENTATION: pulmonary rehabilitation clinic because of ...
Results/Discussion. Bronchial asthma is a chronic inflammatory disease of the airways characterized by bronchial hyperreactivity and a variable degree of airway obstruction. It is diagnosed on the basis of the clinical history, physical examination, and pulmonary function tests, including reversibility testing and measurement of bronchial ...
Dr. Wechsler: This case highlights the problem of asthma-associated morbidity and mortality, with more than 4000 deaths from asthma occurring annually in the United States. 1 This patient's ...
The prevalence of asthma in adults in the United States is approximately 7.7%. 1 It is one of the most common chronic, noncommunicable diseases in the country and worldwide. 1,2 Among U.S. adults ...
A Case of Severe Acute Exacerbation of Bronchial Asthma Treated with Low Minute Ventilation - A Case Report -.pdf Available via license: CC BY-NC 3.0 Content may be subject to copyright.
Clinical case study - asthma . 2019 . Clinical Case Study - Asthma. pdf. Clinical Case Study - Asthma. 6.34 MB. Resource information. Respiratory conditions. Asthma; Respiratory topics. Disease management; Diagnosis; Type of resource. Presentation . Author(s) Jaime Correia de Sousa Ioanna Tsiligianni Miguel Román Rodriguez
Supported self-management reduces asthma morbidity. The lady in this case study is struggling to maintain control of her asthma within the context of her busy professional and domestic life.
The Hupa case study (Hupa, 2015) reported on the evolution of a patient with BA for 22 years since he was diagnosed at 11 years of age. The long-term study based the evaluation of results on ...
Jane Doe #1. 49 year old female. History of heavy tobacco use and asthma. Patient has been feeling somewhat poorly over the last few weeks and her roommate reports that she has been using her nebulizers quite heavily -despite this, she also has continued to smoke quite heavily. The patient's roommate said that the patient was in her room and ...
27423409-Case-Study-of-bronchial-asthma-in-acute-exacerbation - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. Plan: Goal: 4. Encourage rest periods. 4. To allow rest and activities without Mother - Encourage - Maintain or 5. Provide comfort recovery. difficulty or fatigue. ...
Case Study of Bronchial Asthma in Acute Exacerbation - Free download as PDF File (.pdf), Text File (.txt) or read online for free. asthma
Bronchial asthma is a disorder of the airways causing swelling and narrowing; which leads to wheezing, shortness of breath, chest tightness, and coughing. The impact of asthma in children depends on complex interaction between disease severity, reaction of children towards disease, treatment eficiency, social roles, and social environment.
Tamaka shwas and bronchial asthma are associated in current times. The subject in this case study had a condition related to severe asthma. Vamana, because of its Veerya (potency), Dravyas circulate fast in both the body's large and small capillaries, giving them the qualities of Vyavayi and Vikasi. It permeates every part of the body.
A case study of 39-year old man with persistent wheezing, episodes of haemoptysis and dry cough unsuccessfully treated with inhaled beta2-agonists and steroids for about 10 months. Chest radiograph revealed a disproportion in dimensions between both lungs, with the left one being smaller than the right one. Spirometry demonstrated a restrictive pattern. During bronchoscopy, a polypoid ...
Case Study (Bronchial Asthma) - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. The document provides a case study of a 15-year-old male patient admitted to the hospital with bronchial asthma and an acute exacerbation. It details the patient's medical history including a family history of asthma, presents findings from a physical exam and ...
ate therapeutic choice [1-3]. In the present case, the lesion was excised by tracheal wedge resec-tion. As the origin of the lesion was from the posterior tracheal wall and had a wide base, endo-bronchial therapy, which could result either in perforation or insufficient resection, was not con-sidered. In addition, the patient's dyspnoea did
The control of severe bronchial asthma, such as corticosteroid-resistant asthma, is difficult. It is also possible that. immunosuppressi ve agents would be e ffective for bronchial asthma. Case ...
1. Introduction. Bronchial asthma is a common chronic respiratory disease in children, and the etiology is unclear. Most studies indicate that asthma is related to genetic and environmental factors, such as allergic constitution, viral infection, particulate matter, smoke, and ozone exposure [].The main clinical manifestations of asthma include breathlessness, cough, shortness of breath, and ...
Asthma is one of the most common chronic inflammatory diseases of childhood with a heterogeneous impact on health and quality of life. Mepolizumab is an antagonist of interleukin-5, indicated as an adjunct therapy for severe refractory eosinophilic asthma in adolescents and children aged >6 years old. We present the case of a 9 year-old boy with severe asthma who experienced several asthmatic ...
Bronchial Asthma in Acute Exacerbation Case Study - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Acute exacerbations of bronchial asthma (AEBA) are episodes of worsening asthma symptoms requiring urgent care. Common triggers include viral infections, allergens, irritants, and lack of medication adherence.
These extracts may be further developed as natural therapeutic agents for the treatment of asthma and improvement of bronchial health. Disclosure. The funding source had no role in the study design, collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Allergic bronchopulmonary aspergillosis (ABPA) is a multifaceted immune hypersensitivity reaction occurring in the lungs and bronchi, triggered by exposure and colonization of Aspergillus species, commonly Aspergillus fumigatus (A. fumigatus).It typically affects individuals who are immunocompetent but predisposed, such as those with bronchial asthma and cystic fibrosis.
biolincc.nhlbi.nih.gov
Bronchial Asthma (Case Study) - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. This document discusses bronchial asthma, including its objectives, causes, signs and symptoms, and treatment. The objectives are to determine a patient's nursing health history and discuss the causes, signs, and symptoms of asthma.
In the context of this case-control study, the presence of symptoms related to asthma and rhinitis was assessed using the Brazilian version of the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire [17,18,19]. Although the ISAAC is widely recognized and validated for assessing the prevalence and severity of allergic ...