

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Creative Ways to Enhance and Assess Critical Thinking in Nursing Students
Parker, Kimberly C.
About the Author Kimberly C. Parker, DNP, RN, is a clinical instructor, University of Alabama Capstone College of Nursing, Tuscaloosa, Alabama. For more information, contact her at [email protected] .
The author has declared no conflict of interest.
Nursing students should be challenged to implement critical thinking decisions regarding conclusions they implement for patient care. This article reinforces common techniques and introduces new practices to teach critical thinking. Many ways are currently recognized utilizing an assortment of techniques. The concepts from an escape room are a great way to deliver opportunities for students to practice this skill and can be provided economically and easily. Being creative in managing these concepts will offer an exciting chance to introduce critical thinking for your students.
Full Text Access for Subscribers:
Individual subscribers.

Institutional Users
Not a subscriber.
You can read the full text of this article if you:
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Escape room: innovative teaching strategy to stimulate critical..., objectives and outcomes: the fundamental difference, retention of nursing students: an integrative review, can you escape nursing school educational escape room in nursing education, a dynamic relationship between theory and research in nursing education.
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
We use cookies on our website to support technical features that enhance your user experience, and to help us improve our website. By continuing to use this website, you accept our privacy policy .
- Student Login
- Call Us: 888-549-6755
- 888-559-6763
- Search site Search our site Search Now Close
- Request Info
Skip to Content (Press Enter)
Why Critical Thinking Skills in Nursing Matter (And What You Can Do to Develop Them)
By Hannah Meinke on 07/05/2021
The nursing profession tends to attract those who have natural nurturing abilities, a desire to help others, and a knack for science or anatomy. But there is another important skill that successful nurses share, and it's often overlooked: the ability to think critically.
Identifying a problem, determining the best solution and choosing the most effective method to solve the program are all parts of the critical thinking process. After executing the plan, critical thinkers reflect on the situation to figure out if it was effective and if it could have been done better. As you can see, critical thinking is a transferable skill that can be leveraged in several facets of your life.
But why is it so important for nurses to use? We spoke with several experts to learn why critical thinking skills in nursing are so crucial to the field, the patients and the success of a nurse. Keep reading to learn why and to see how you can improve this skill.
Why are critical thinking skills in nursing important?
You learn all sorts of practical skills in nursing school, like flawlessly dressing a wound, taking vitals like a pro or starting an IV without flinching. But without the ability to think clearly and make rational decisions, those skills alone won’t get you very far—you need to think critically as well.
“Nurses are faced with decision-making situations in patient care, and each decision they make impacts patient outcomes. Nursing critical thinking skills drive the decision-making process and impact the quality of care provided,” says Georgia Vest, DNP, RN and senior dean of nursing at the Rasmussen University School of Nursing.
For example, nurses often have to make triage decisions in the emergency room. With an overflow of patients and limited staff, they must evaluate which patients should be treated first. While they rely on their training to measure vital signs and level of consciousness, they must use critical thinking to analyze the consequences of delaying treatment in each case.
No matter which department they work in, nurses use critical thinking in their everyday routines. When you’re faced with decisions that could ultimately mean life or death, the ability to analyze a situation and come to a solution separates the good nurses from the great ones.
How are critical thinking skills acquired in nursing school?
Nursing school offers a multitude of material to master and upholds high expectations for your performance. But in order to learn in a way that will actually equip you to become an excellent nurse, you have to go beyond just memorizing terms. You need to apply an analytical mindset to understanding course material.
One way for students to begin implementing critical thinking is by applying the nursing process to their line of thought, according to Vest. The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation.
“One of the fundamental principles for developing critical thinking is the nursing process,” Vest says. “It needs to be a lived experience in the learning environment.”
Nursing students often find that there are multiple correct solutions to a problem. The key to nursing is to select the “the most correct” solution—one that will be the most efficient and best fit for that particular situation. Using the nursing process, students can narrow down their options to select the best one.
When answering questions in class or on exams, challenge yourself to go beyond simply selecting an answer. Start to think about why that answer is correct and what the possible consequences might be. Simply memorizing the material won’t translate well into a real-life nursing setting.
How can you develop your critical thinking skills as a nurse?
As you know, learning doesn’t stop with graduation from nursing school. Good nurses continue to soak up knowledge and continually improve throughout their careers. Likewise, they can continue to build their critical thinking skills in the workplace with each shift.
“To improve your critical thinking, pick the brains of the experienced nurses around you to help you get the mindset,” suggests Eileen Sollars, RN ADN, AAS. Understanding how a seasoned nurse came to a conclusion will provide you with insights you may not have considered and help you develop your own approach.
The chain of command can also help nurses develop critical thinking skills in the workplace.
“Another aid in the development of critical thinking I cannot stress enough is the utilization of the chain of command,” Vest says. “In the chain of command, the nurse always reports up to the nurse manager and down to the patient care aide. Peers and fellow healthcare professionals are not in the chain of command. Clear understanding and proper utilization of the chain of command is essential in the workplace.”
How are critical thinking skills applied in nursing?
“Nurses use critical thinking in every single shift,” Sollars says. “Critical thinking in nursing is a paramount skill necessary in the care of your patients. Nowadays there is more emphasis on machines and technical aspects of nursing, but critical thinking plays an important role. You need it to understand and anticipate changes in your patient's condition.”
As a nurse, you will inevitably encounter a situation in which there are multiple solutions or treatments, and you'll be tasked with determining the solution that will provide the best possible outcome for your patient. You must be able to quickly and confidently assess situations and make the best care decision in each unique scenario. It is in situations like these that your critical thinking skills will direct your decision-making.
Do critical thinking skills matter more for nursing leadership and management positions?
While critical thinking skills are essential at every level of nursing, leadership and management positions require a new level of this ability.
When it comes to managing other nurses, working with hospital administration, and dealing with budgets, schedules or policies, critical thinking can make the difference between a smooth-running or struggling department. At the leadership level, nurses need to see the big picture and understand how each part works together.
A nurse manager , for example, might have to deal with being short-staffed. This could require coaching nurses on how to prioritize their workload, organize their tasks and rely on strategies to keep from burning out. A lead nurse with strong critical thinking skills knows how to fully understand the problem and all its implications.
- How will patient care be affected by having fewer staff?
- What kind of strain will be on the nurses?
Their solutions will take into account all their resources and possible roadblocks.
- What work can be delegated to nursing aids?
- Are there any nurses willing to come in on their day off?
- Are nurses from other departments available to provide coverage?
They’ll weigh the pros and cons of each solution and choose those with the greatest potential.
- Will calling in an off-duty nurse contribute to burnout?
- Was this situation a one-off occurrence or something that could require an additional hire in the long term?
Finally, they will look back on the issue and evaluate what worked and what didn’t. With critical thinking skills like this, a lead nurse can affect their entire staff, patient population and department for the better.
Beyond thinking
You’re now well aware of the importance of critical thinking skills in nursing. Even if you already use critical thinking skills every day, you can still work toward strengthening that skill. The more you practice it, the better you will become and the more naturally it will come to you.
If you’re interested in critical thinking because you’d like to move up in your current nursing job, consider how a Bachelor of Science in Nursing (BSN) could help you develop the necessary leadership skills.
EDITOR’S NOTE: This article was originally published in July 2012. It has since been updated to include information relevant to 2021.
- Share on Facebook
- Share on Twitter
- Share on Pinterest
- Share on LinkedIn
Request More Information
Talk with an admissions advisor today.
Fill out the form to receive information about:
- Program Details and Applying for Classes
- Financial Aid (for those who qualify)
- Customized Support Services
- Detailed Program Plans
There are some errors in the form. Please correct the errors and submit again.
Please enter your first name.
Please enter your last name.
There is an error in email. Make sure your answer has:
- An "@" symbol
- A suffix such as ".com", ".edu", etc.
There is an error in phone number. Make sure your answer has:
- 10 digits with no dashes or spaces
- No country code (e.g. "1" for USA)
There is an error in ZIP code. Make sure your answer has only 5 digits.
We offer tuition savings for many employers—see if yours is one of them.
Please enter Corporate Employer.
Can’t find your employer? Select "Other Employer Not In List" or "Not Employed".
Please choose a School of study.
Please choose a program.
Please choose a degree.
The program you have selected is not available in your ZIP code. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
The program you have selected requires a nursing license. Please select another program or contact an Admissions Advisor (877.530.9600) for help.
Rasmussen University is not enrolling students in your state at this time.
By selecting "Submit," I authorize Rasmussen University to contact me by email, phone or text message at the number provided. There is no obligation to enroll. This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
About the author
Hannah Meinke

Posted in General Nursing
- nursing education
Related Content

Brianna Flavin | 05.07.2024

Brianna Flavin | 03.19.2024

Robbie Gould | 11.14.2023

Noelle Hartt | 11.09.2023
This piece of ad content was created by Rasmussen University to support its educational programs. Rasmussen University may not prepare students for all positions featured within this content. Please visit www.rasmussen.edu/degrees for a list of programs offered. External links provided on rasmussen.edu are for reference only. Rasmussen University does not guarantee, approve, control, or specifically endorse the information or products available on websites linked to, and is not endorsed by website owners, authors and/or organizations referenced. Rasmussen University is accredited by the Higher Learning Commission, an institutional accreditation agency recognized by the U.S. Department of Education.

Effective clinical learning for nursing students
Approaches that meet student and nurse needs..
- Direct care nurses serve as significant teachers and role models for nursing students in the clinical setting.
- Building critical thinking skills is one of the most important outcomes in the clinical setting for nursing students.
- Collaboration with nursing faculty during the clinical rotation can ease the burden on direct care nurses and facilitate a positive learning experience for the student.
The nursing profession continues to experience several challenges—some longstanding and exacerbated by the COVID-19 pandemic. The shortage of nurses at the bedside and reports of nurses planning to leave the profession soon place stress on the workforce and the healthcare system. The situation has put even more pressure on nursing schools to recruit and retain students who enter the workforce well-prepared for practice and capable of filling these vacancies. However, concerns exist surrounding students’ critical thinking skills and their readiness for a demanding career.
The challenge
A longstanding shortage of nursing school faculty and a reliance on new graduate nurses to serve as preceptors create challenges to properly preparing nursing students for a demanding role that requires excellent critical thinking skills.
What-Why-How? Improving Clinical Judgement
New nurses and clinical judgment
Nurse faculty shortage
Lack of interest and incentives lead to difficulty recruiting nurses from the bedside or practice to education. Many 4-year schools require a terminal degree to teach full-time in their undergraduate programs, but only 1% of nurses hold a PhD. In addition, according to the National Advisory Council on Nurse Education and Practice (NACNEP), the average doctorally prepared nurse faculty member is in their 50s, which means they may soon retire. The surge in doctor of nursing practice programs has helped to bridge this gap, but attracting advanced practice nurses to academia from their more lucrative practice roles continues to prove difficult.
Concerns about the practice readiness of new graduate nurses have existed for several years. Missed clinical experiences and virtual learning during the COVID-19 pandemic heightened those concerns. The National Council of State Boards of Nursing (NCSBN) addressed the calls from nurse employers to make progress in this area by revamping the NCLEX-RN and NCLEX-PN exams to create Next Generation NCLEX (NGN), which includes more clinical judgment and critical thinking items. Nurse educators are working hard to prepare students for both practice and the new exam items by incorporating more active learning into classroom, clinical, and lab activities and emphasizing the importance of clinical judgment skills.
In most areas of the country, clinical student experiences have returned to pre-pandemic arrangements. State boards of nursing mandate maximum faculty-to-student ratios for clinical experiences. Schools can choose to have faculty supervise fewer students than the maximum, but faculty and clinical site shortages may eliminate that option. In many cases, preceptor-style experiences (such as capstone or practicum courses) have higher faculty-to-student ratios, and preceptors may have to meet specific criteria, such as a certain amount of experience.
Nursing faculty who facilitate on-site learning and supervise and teach students during their clinical experiences face several challenges. Some faculty supervise students across multiple units because unit size can’t accommodate 8 to 10 students at one time. Faculty may or may not have access to the organization’s electronic health records or other healthcare information technology, such as medication dispensing cabinets or glucometers.
In such instances, direct care nurses play an important role in the student’s experience at the clinical site. Their familiarity with the unit, the patient population, and the organization’s technology facilitates learning.
Direct care nurses
Allowing nursing students into the hospital can improve the patient care experience and potentially recruit students to work at the organization in the future. However, precepting a student or new employee creates an extra burden on an already overextended bedside nurse. NACNEP identifies several challenges for obtaining qualified preceptors, including lack of incentives and limited preparation in clinical teaching and learning strategies. Many hospitals have nursing students on the same unit several days a week to accommodate multiple area schools. This means that staff nurses are expected to teach students on most of their workdays during a typical school semester.
Unit nurse experience creates another barrier to effective precepting of nursing students. A study by Thayer and colleagues reported that the median length of experience for inpatient nurses working a 12-hour shift was less than 3 years at an organization. Without a better alternative, new graduate nurses frequently teach nursing students, although they may still be in what Benner describes as the advanced beginner stage of their career (still learning how to organize care, prioritize, and make clinical judgments). It’s difficult for someone who’s still learning and experiencing situations for the first time to teach complex concepts.
A guide to effective clinical site teaching
The following strategies promote critical thinking in students and collaboration with nurse faculty to ease direct care nurses’ teaching workload. Not every strategy is appropriate for all student clinical experiences. Consider them as multiple potential approaches to help facilitate meaningful learning opportunities.
Set the tone
Nursing students frequently feel anxious about clinical experiences, especially if they’ve been told or perceive that they’re a burden or unwanted on the unit. When meeting the student for the first time, welcome them and communicate willingness to have them on the unit.
If you feel that you can’t take on a student for the day, speak to the nurse faculty member and charge nurse to explore other arrangements. Nurse faculty recognize that work or personal concerns may require you to decline precepting a student. Faculty members want to find the best situation for everyone. If the charge nurse or supervisor determines that the student still needs to work with you, talk to the nurse faculty about how they can help ease the burden and facilitate the student’s learning experience for the day.
Begin your time with the student by asking about their experience level and any objectives for the day. Understanding what the student can or can’t do will help you make the most out of the clinical experience. You’ll want to know the content they’re learning in class and connect them with a patient who brings those concepts to life. A student may have assignments to complete, but their focus should be on patient care. Help the student identify the busiest parts of the day and the best time to review the electronic health record and complete assignments.
If a situation requires your full attention and limits training opportunities, briefly explain to the student what will happen. If you have time, provide the student with tasks or specific objectives to note during the observation. Involve the nursing faculty member to help facilitate the learning experience and make it meaningful.
Be a professional role model
Students like to hear about the benefits and rewards of being a nurse, and about each nurse’s unique path. Students also enjoy learning about the “real world” from nurses, but keep in mind that they’re impressionable. Speaking negatively about the unit, patients, organization, or profession may discourage the student. If you must deviate from standard care, such as performing a skill differently than it’s traditionally taught in school, provide the rationale or hospital policy behind the decision.
Feel free to discuss the student’s nursing school experience but don’t diminish the value of their education or assigned work. Keep in mind that school assignments, such as nursing care plans or concept maps, aren’t taught for job training but to deliberately and systematically promote critical thinking. These assignments allow a student to reflect on how a patient’s pathophysiology and nursing assessment and interventions relate to one another.
Reinforce how concepts students learn in school provide valuable knowledge in various settings. For example, if the student is on a medical-surgical unit but says that they want to work in obstetrics, engage the student by pointing out links between the two areas, such as managing diabetes and coagulation disorders. Provide encouragement and excitement about the student’s interest in joining the profession at a time of great need.
Build assessment skills
Explain to students your approach to performing assessments and organizing patient care. Most students learn comprehensive head-to-toe assessments but, in the clinical setting, need to focus on the most relevant assessments. To promote critical thinking, ask the student what data they should focus on gathering based on the patient’s condition. Many students focus on the psychomotor aspect of assessment (performing the assessment correctly); ask them about the subjective data they should gather.
Allow the student to perform an assessment and then compare findings. For example, a student may know that a patient’s lung sounds are abnormal but not remember what the sound is called or what it means. Provide them with the correct terminology to help connect the dots. Discuss with the student when reassessments are warranted. If appropriate, allow a student to reassess the patient (vital signs, output, pain, other physical findings) and then confirm their findings and discuss what any changes mean for the clinical situation. If you don’t have time for these types of discussions following a student’s patient assessment, ask nursing faculty to observe and discuss findings with the student.
Discuss care management
Take advantage of opportunities to discuss concepts such as prioritization, advocacy, delegation, collaboration, discharge planning, and other ways in which the nurse acts as a care manager. Pointing out what’s appropriate to delegate to unlicensed assistive personnel or a licensed practical nurse will prove valuable and help reinforce concepts frequently covered on the NGN exam.
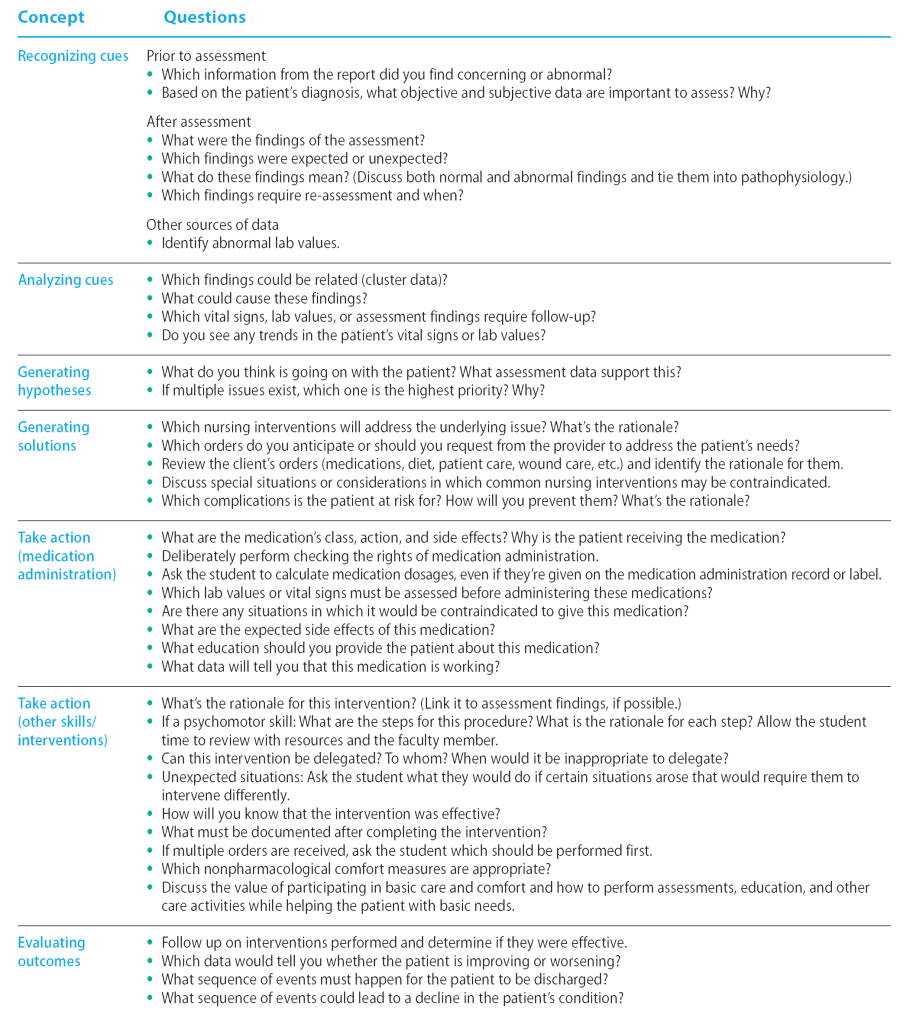
Promote critical thinking
The NCBSN has introduced the Clinical Judgment Measurement Model (CJMM) as a framework for evaluating the NGN exam, which incorporates unfolding case studies that systematically address six steps: recognize cues, analyze cues, generate hypotheses, generate solutions, take action, and evaluate outcomes. Each candidate encounters three case studies, with six questions, one for each step of the CJMM. Nursing faculty incorporate this framework and language into the nursing curriculum to help students think systematically and critically and prepare them for the exam.
Nurses with practice experience use this type of framework to gather information, make judgments, and take action. As a nurse approaches Benner’s competent stage of nursing practice, this type of thinking becomes intuitive, and nurses may not even be aware of the conclusions they draw and decisions they make based on their clinical judgment skills. To help students understand why something is happening, they should continue to work through a process like this deliberately. For example, many students view medication administration as a simple task and may say in post-conference discussion, “All I did was give meds.” You perform many assessments and make various judgments while administering medications, but you may not think to discuss them with students. Asking questions of students while they’re performing what may seem like repetitive tasks can help prompt critical thinking. (See Critical questions .)
Critical questions
Enhance self-efficacy
Many nurses believe that the student must follow them to every patient. This can be overwhelming for the direct care nurse and a barrier to agreeing to work with students. Other approaches can better facilitate learning. Most students will complete an assignment focused on one or two patients. Encourage the student to spend time alone with those patients to perform a more comprehensive history and assessment, help patients with basic care, and provide education. Select a patient who might enjoy the extra attention to ensure a mutually beneficial experience.
Also, consider asking the student to find information using available resources. Such inquiry can benefit you and the student. For example, prompt a student to answer one or more critical thinking questions using their textbooks or resources available on the hospital’s intranet. If time prevents you from explaining complex topics or helping the student problem-solve, ask the student to take the information they find to their faculty member to review. Nurse faculty won’t be familiar with the specific details of all patients on the unit, so identify the most appropriate questions for the student to consider to help the nurse faculty facilitate learning.
Allowing the student time to find answers themselves builds self-efficacy and confidence and also relieves some of the stress and anxiety associated with being asked questions on the spot. This strategy also models the professional approach of using evidence-based resources to find information as needed in the clinical setting.
To ensure a positive learning experience and reduce anxiety, provide the student with ample time to prepare for performance-based skills. For example, identify an approximate time that medications will be administered to one patient and ask the student to independently look up the medication information by that time. This is more beneficial for the student than observing every patient’s medication administration or participating only in psychomotor tasks, such as scanning and giving injections. This also can free up your time by setting the expectation that the student will have the chance to prepare for and be directly involved in one medication pass.
Similarly, if an opportunity exists for practicing a psychomotor skill, such as inserting a urinary catheter or suctioning a tracheostomy, ask the student to review the procedure with their instructor using hospital policy and resources. If time doesn’t allow for a review, have the student observe to ensure provision of the best care and efficient use of time and resources.
Opportunities in education
Nurses who enjoy working with students or new staff members may want to consider academic roles. Many advanced nursing degrees, available in various formats, focus on education. For those who want to try teaching or have an interest in teaching only in the clinical setting, opportunities exist to work as adjunct faculty or to participate in hospital-based professional development activities. Adjunct faculty (part-time instructors) teach a variety of assignments and workloads, including in clinical, lab, or classroom settings. Many clinical adjunct faculty are nurses who also work in the organization with patients and may teach one group of students one day a week. Clinical and lab assignments vary from 4- or 6-hour experiences to 12-hour shifts.
According to NACNEP, most nursing programs require that adjunct faculty and clinical preceptors have the same or higher level of educational preparation as the program; for example, a nurse with a bachelor of science in nursing (BSN) may be able to teach clinicals for associate degree in nursing or BSN programs, depending on the state’s requirements and the school’s needs. Educational requirements to work in nursing programs vary by school. In some cases, adjunct faculty who don’t have a master’s degree may be supervised by full-time faculty with advanced degrees.
Benefits for adjunct faculty can include extra income, professional development, personal reward, tuition discounts or remissions, and giving back to the profession. Locate opportunities on nursing school websites or by talking to the nursing instructors or administrators in the local area.
Everyone benefits
Applying teaching approaches that benefit students and nurses can help ensure a positive clinical learning experience for everyone. When you graciously accept and teach students you help create positive encounters that enhance student critical thinking skill development, aid program retention, and support organizational recruitment.
Jennifer Miller is an assistant professor of nursing at the University of Louisville School of Nursing in Louisville, Kentucky .
American Nurse Journal. 2024; 19(4). Doi: 10.51256/ANJ042432
American Association of Colleges of Nursing. Nursing faculty shortage fact sheet. October 2022. aacnnursing.org/news-information/fact-sheets/nursing-faculty-shortage
Benner P. From Novice to Expert: Excellence and Power in Clinical Nursing Practice . Menlo Park, CA: Addison-Wesley; 1984.
National Advisory Council on Nurse Education and Practice. Preparing nurse faculty, and addressing the shortage of nurse faculty and clinical preceptors. January 2021. hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/nacnep-17report-2021.pdf
National Council of State Boards of Nursing. Clinical Judgment Measurement Model. 2023. nclex.com/clinical-judgment-measurement-model.page
Thayer J, Zillmer J, Sandberg N, Miller AR, Nagel P, MacGibbon A. ‘The new nurse’ is the new normal. June 2, 2022. Epic Research. epicresearch.org/articles/the-new-nurse-is-the-new-normal
Key words: nursing students, nursing education, critical thinking, precepting
Let Us Know What You Think
1 comment . leave new.
All nursing programs need to put in more clinical time. Students do not get the time in clinicals so they do not have the opportunities to develop their clinical judgement and thinking skills. Clinical time is what glues concept and theory together if they don’t get the clinical time they are less likely to develop these skills which contributes to errors, burnout and nurses leaving the field.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.

Hypnosis and pain

Measuring nurses’ health

From Retirement to Preferment: Crafting Your Next Chapter

Leadership in changing times

Valuing nursing
Promoting health literacy

Mentorship: A strategy for nursing retention
Anatomy of Writing for Publication for Nurses: The writing guide you’ve been looking for

Nurse leadership: Pitfalls and solutions

It’s time embrace AI in nursing
CMS establishes minimum LTC staffing standards

Mental health matters

Connecting the dots with cannabis care

Wellness challenges

Writing retreats for nurses: Inspiration to share
Miller J. Effective clinical learning for nursing students. American Nurse Journal. 2024;19(4):32-37. doi:10.51256/anj042432 https://www.myamericannurse.com/effective-clinical-learning-for-nursing-students/

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
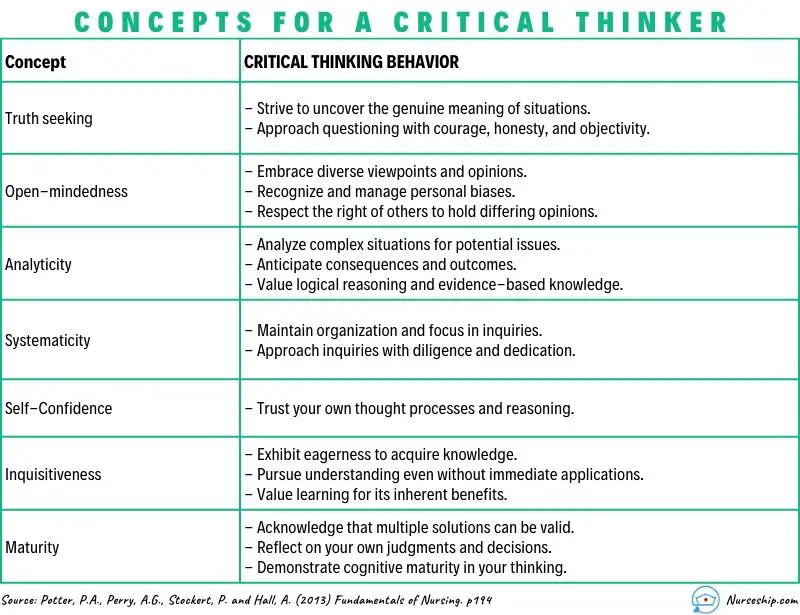
What are the Levels of Critical Thinking in Nursing?
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.

Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.
Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
| Level 1: Gathering | 1. What are the common side effects of the prescribed medication? 2. When was the patient’s last bowel movement? 3. Who is the patient’s emergency contact person? 4. Describe the patient’s current level of pain. 5. What information is in the patient’s medical record? |
| 1. What would happen if the patient’s blood pressure falls further? 2. Compare the patient’s oxygen saturation levels before and after administering oxygen. 3. What other nursing interventions could be considered for wound care? 4. Infer the potential reasons behind the patient’s increased heart rate. 5. Analyze the relationship between the patient’s diet and blood glucose levels. | |
| 1. What do you think will be the patient’s response to the new pain management strategy? 2. Could the patient’s current symptoms be indicative of an underlying complication? 3. How would you prioritize care for patients with varying acuity levels in the emergency department? 4. What evidence supports your choice of administering the medication at this time? 5. Create a care plan for a patient with complex needs requiring multiple interventions. |
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
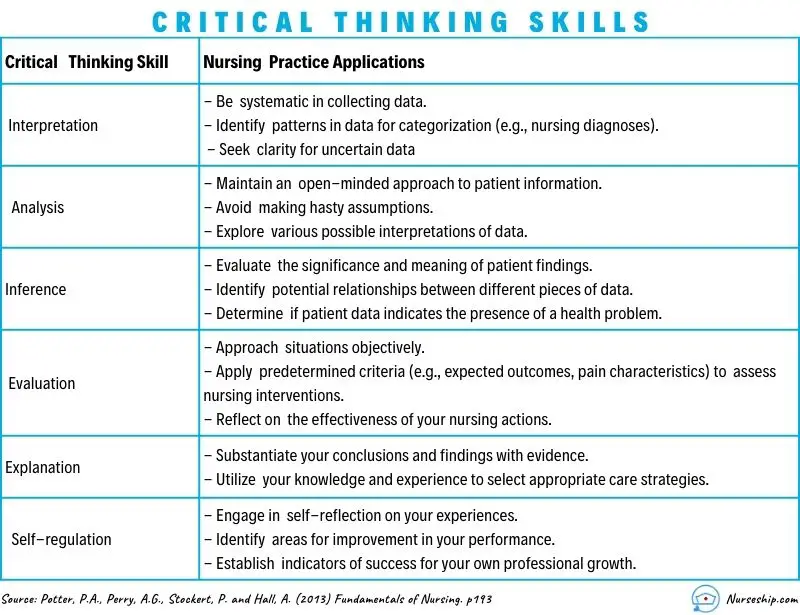
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

How to Strengthen & Develop the Critical Thinking Students Require for Practice
Keith Rischer – Ph.D., RN, CCRN, CEN
As a nurse with over 35 years of experience who remained in practice as an educator, I’ve witnessed the gap between how nursing is taught and how it is practiced, and I decided to do something about it! Read more…
The Ultimate Solution to Develop Clinical Judgment Skills
KeithRN’s Think Like a Nurse Membership
Access exclusive active learning resources for faculty and students, including KeithRN Case Studies, making it your go-to resource.
Sign up to receive a free KeithRN NextGen Case Study!
Develop clinical judgment skills with this innovative new case study on asthma to prepare your students for nextgen nclex and practice.
" * " indicates required fields
Keith Rischer
Why pathophysiology must be deeply understood to think more like a nurse, recommended for you.

Course Design Design Framework Canvas Templates Course Content Hybrid Courses Online Courses Student Assessment
Critical thinking + clinical reasoning = strong clinical judgment
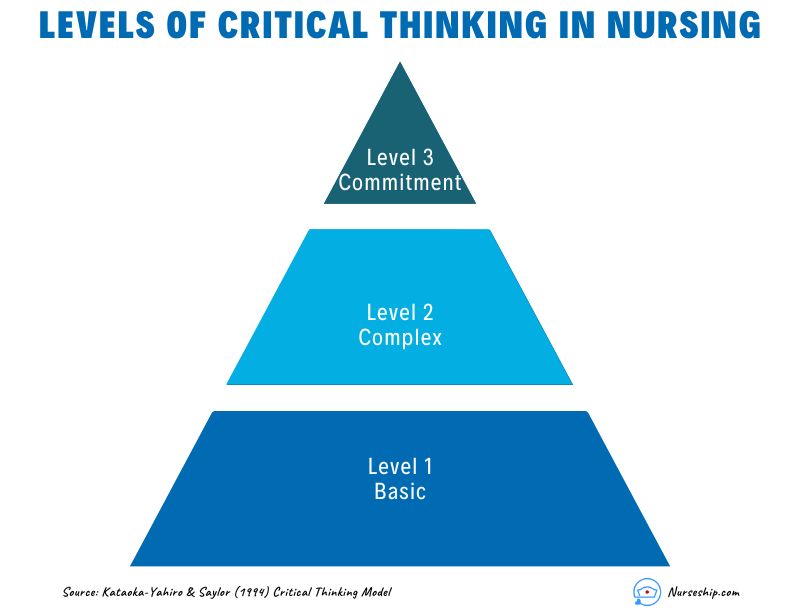
Critical thinking
To develop critical thinking skills, students must engage in activities encouraging analyzing, discriminating, information-seeking, and open-mindedness. Critical thinking requires students to think precisely and accurately and act on what they know and understand; critical thinking precedes clinical reasoning (Manetti, 2018; Potter & Perry, 2012; Alfaro-LeFevre, 2017).
Clinical reasoning
Clinical reasoning involves a student's ability to apply knowledge, think in action, and reason as a situation changes over time (Benner, et al., 2010). the analysis of data is done through four steps:
- noticing relevant clinical data
- interpreting the clinical significance of data
- responding appropriately by prioritizing responses and actions
- reflecting on the effectiveness of the response (Tanner, 2006).
Clinical judgment
Clinical judgment results in a student's conclusions after making a holistic assessment that correctly interprets clinical data to determine the best response. It is an outcome that depends on critical thinking, clinical reasoning, and intuition (Rischer, 2021).
In nursing, for example, strong clinical judgment involves choosing the best response among alternative actions in light of expected outcomes, using ongoing evaluative reflection to monitor a patient's response, and modifying interventions accordingly. Reflecting on clinical decisions afterward improves judgment when caring for future patients (Alfaro-LeFevre, 2017; Tanner, 2006; Manetti, 2019).
Clinical judgment models for nursing instruction
Nursing process (american nurses association).
- Assessment — the nurse assesses patients on an in-depth physiological, economic, social, and lifestyle basis.
- Diagnosis and analysis — the nurse considers the physical symptoms and patient behavior and forms a diagnosis or analysis of cues to determine the current nursing priority.
- Outcomes and planning — the nurse uses their expertise to set realistic goals for the patient's recovery and monitors those objectives closely.
- Implementation — the nurse implements the care plan and documents the patient's progress.
- Evaluation — the nurse analyzes the effectiveness of the care plan, studies the patient response, and alters the plan of care to achieve the best patient outcomes. (ANA Standards of Critical Nursing Practice, 1988).
Tanner's Clinical Judgment Model
- Noticing — What clinical data does the nurse recognize as important and/or significant?
- Interpreting — What is the meaning or clinical significance of relevant clinical data that was noticed?
- Responding — How will the nurse respond with a nursing priority and care plan based on the clinical data that was noticed and interpreted?
- Reflecting — After responding, what is the evaluation, reflecting on clinical data noticed by the nurse? (Tanner, 2006)
Revised Clinical Judgment Model
Based on Tanner's Clinical Judgment Model and Neilsen, Stragnell, and Jester's article Guide for Reflection using the Clinical Judgment Model, instructors from the UW-Madison School of Nursing have developed a revised model that also addresses issues of diversity, equity, social justice, and health equity into the equation. This added element of Personalizing asks the nurse to consider the emotions, reactions, beliefs, and biases they bring to the care of a patient and develop a self-care plan that manages these feelings to ensure fair and equitable patient care.

- Alfaro-LeFevre, R. (2017). Critical thinking, clinical reasoning, and clinical judgment: A practical approach. (6th ed.). St. Louise, MO: Elsevier-Saudners.
- Benner, P., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation . San Francisco, CA: Jossey-Bass.
- Manetti, W. (2019). Sound clinical judgment in nursing: A concept analysis: MANETTI. Nursing Forum, 54)1, 102-110.
- Nielsen, A., Stragnell, S., & Jester, P. (2007) Guide for reflection using the clinical judgment model. The Journal of Nursing Education , 46(11), 513-516.
- Rischer, K. (2021). Faculty guide to develop clinical judgment: Transforming nursing education through the use of clinical reasoning case studies.
- Tanner, C.A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. The Journal of Nursing Education, 45(6) , 204-211).
CTLM Instructional Resources KnowledgeBase Menu Home Course Design Course Refinement Inclusive Teaching Teaching Readiness Teaching Strategies Technology Integration CTLM Site
| Keywords | clinical judgement, judgment, analyzing, discriminating, information-seeking, open-mindedness, tanner | Doc ID | 121687 |
|---|---|---|---|
| Owner | Timmo D. | Group | Instructional Resources |
| Created | 2022-10-05 08:30:41 | Updated | 2024-08-23 15:32:27 |
| Sites | Center for Teaching, Learning & Mentoring | ||
| Feedback | 4 1 | ||
- Open access
- Published: 26 August 2024
Using a flipped teaching strategy in undergraduate nursing education: students’ perceptions and performance
- Shaherah Yousef Andargeery 1 ,
- Hibah Abdulrahim Bahri 2 ,
- Rania Ali Alhalwani 1 ,
- Shorok Hamed Alahmedi 1 &
- Waad Hasan Ali 1
BMC Medical Education volume 24 , Article number: 926 ( 2024 ) Cite this article
18 Accesses
Metrics details
Flipped teaching is an interactive learning strategy that actively engages students in the learning process. Students have an active role in flipped teaching as they independently prepare for the class. Class time is dedicated to discussion and learning activities. Thus, it is believed that flipped teaching promotes students’ critical thinking, communication, application of knowledge in real-life situations, and becoming lifelong learners. The aim of this study was to describe the students’ perception of flipped teaching as an innovative learning strategy. And to assess if there was a difference in students’ academic performance between those who participated in a traditional teaching strategy compared to those who participated in flipped teaching intervention.
A quasi-experimental design with intervention and control groups. A purposive sampling technique of undergraduate nursing students was used.
A total of 355 students participated in both groups, and 70 out of 182 students in the intervention group completed the survey. The students perceived a moderate level of effectiveness of the flipped teaching classroom as a teaching strategy. The result revealed that there is a statistically significant difference in the mean students’ scores for the intervention group (M = 83.34, SD = 9.81) and control group (M = 75.57, SD = 9.82).
Flipped teaching proves its effectiveness in improving students’ learning experience and academic performance. Also, students had a positive perception about flipped teaching as it allowed them to develop essential nursing competencies. Future studies must consider measuring the influence of flipped teaching on students’ ability to acquire nursing competencies, such as critical thinking and clinical reasoning.
Peer Review reports
The successful outcome of individualized nursing care of each patient depends on effective communication between nurses and patients. Therapeutic communication consists of an exchange of verbal and non-verbal cues. It is a process in which the professional nurse uses specific techniques to help patients better understand their conditions and promote patients’ open communication of their thoughts and feelings in an environment of mutual respect and acceptance [ 1 ]. Effective educational preparation, continuing practice, and self-reflection about one’s communication skills are all necessary for becoming proficient in therapeutic communication. Teaching therapeutic communication to nursing students explains the principles of verbal and non-verbal communication that can be emphasized through classroom presentation, discussion, case studies and role-play. It also helps them develop their ability to communicate effectively with patients, families, and other health care professionals. Nursing students should be able to critically think, conceptualizing, applying, analyzing, synthesizing, and evaluating information generated by observation, experience, reflection, reasoning, and communication. Utilizing a traditional teaching strategy can be a challenge to meet the previously stated requirements [ 2 ]. Therefore, nurse educators should adapt unique teaching methods to help students learn and participate in their own education.
The “flipped classroom” is a pedagogical approach that has gained popularity worldwide to foster active learning. Active learning is defined as instructional strategies that actively engage students in their learning. It requires them to do meaningful learning activities and reflect on their actions [ 3 ]. Flipped teaching is a teaching strategy that promotes critical thinking and the application of information learned outside of the classroom to real-world situations and solves problems within the classroom. It is used in a way that allows educators to deliver lectures by using technologies such as video, audio files, PowerPoint or other media. Thus, the students can read or study those materials on their own at home before attending the class. As a result, discussions and debates about the materials take place throughout the lecture time. Some of the main principles of flipped teaching are increasing interaction and communication between students and educators, allocating more time for content mastery and understanding, granting opportunities for closing gaps and development, creating opportunities for active engagement, and providing immediate feedback [ 4 , 5 ]. This teaching/learning methodology is supported by constructivism learning theory. A “problem-solving approach to learning” is how constructivism is frequently described. In which, it requires a shift in the nurse educator’s epistemic assumptions about the teaching-learning process. Constructivism requires nursing educators to take on the role of a learning facilitator who encourages collaboration and teamwork as well as guides the students in building their knowledge. The underlying assumptions of constructivism include the idea that learning occurs as a result of social interaction in which the student actively creates their own knowledge, while prior experiences serve as the foundation for the learning process. The “flipping classroom” reflects that approach, which integrates student-centered learning [ 6 ].
Flipped teaching approach has students learning before lectures, teaching the material to better use classroom time for cooperative learning. The discussed herein represents studies and case studies from primary through graduate schools. The literature indicated students did see value in this pedagogical approach. Most of the studies found that flipped teaching was associated with better understanding of the material learned, higher academic achievement/performance, and potentially improved psychosocial factors (self-esteem, self-efficacy) that are associated with learning. Interestingly, one article pointed out that non-didactic material used in flipped-teaching lead to an increase in performance and this did not happen with didactic material.
According to Jordan et al. [ 7 ], a flipped teaching is a methodology that was developed as a response to advancements and changes in society, pedagogical approaches, and rapid growth and advancement of technology; The flipped teaching was evolved from the peer instruction and just in time teaching approaches. Jordan and colleagues [ 7 ] state that independent learning happens outside the classroom prior to the lesson through instructional materials while classroom time is maximized to fosters an environment of collaborative learning. Qutob [ 8 ] states that flipped teaching enhances student learning and engagement and promotes greater independence for students.
Jordan et al. [ 7 ] studied the use of flipped teaching on the teaching of first- and fourth-year students’ discrete mathematics and graphs, models, and applications. Across all the classes studied (pilot, graph, model and application, practices, computer and business administration), students preferred flipped teaching compared to traditional teaching. According to Jordan et al. [ 7 ], the quality of the materials and exercises, and perceived difficulty of the course and material are important to student satisfaction with this method. Additionally, it was found that interactions with teachers and collaborative learning were positive. Likewise, Nguyen et al. [ 9 ] found students favorably perceive flipped teaching. This is especially true for those students who have an understanding that the method involves preparation and interaction and how these affect the outcomes. Vazquez and Chiang [ 10 ] discuss the lessons learned from observing two large Principles of Economics Classes at the University of Illinois; each class held 900 students. Vazquez and Chiang [ 10 ] found that the students preferred watching videos over reading the textbook. Secondly, students were better prepared after they watched pre-lecture videos compared to reading the textbook beforehand. The third finding involved the length of time pre-lecture work should take; the authors state pre-lecture work should be approximately 15 to 20 min of work ahead of each in-class session. The fourth finding is that the flipped teaching is a costly endeavor. Finally, it was found that having the students watch videos before the lectures reduced the time spent in class covering the material; the end result of this is students spend more time engaging in active learning than reviewing the material.
Qutob [ 8 ] studied the effects of flip teaching using two hematology courses. One of the courses was delivered using traditional teaching and the other course was flipped teaching. Qutob [ 8 ] found that students in the flipped course not only performed better on academic tasks, but also they had more knowledge and understanding of the material covered compared to those in the traditional format class. Additionally, Qutob [ 8 ] revealed that students in the flipped classroom found this style of learning is more beneficial than traditional teaching. Moreover, Florence and Kolski [ 11 ] found an improvement in high school students’ writing post-intervention. The authors further found that students were more engaged with the material and had a positive perception of the flipped model. Bahadur and Akhtar [ 12 ] conducted a meta-analysis of twelve research articles on flipped teaching; the studies demonstrated that students taught in the flip teaching classroom performed better academically and were more interactive and engaged in the material than students taught through traditional methods. Galindo-Dominguez [ 13 ] conducted a systematic review using 61 studies and found evidence for the effectiveness of this approach compared to other pedagogical approaches with regards to academic achievement, improved self-efficacy, motivation, engagement, and cooperativeness. Webb et al. [ 14 ] studied 127 students taking microeconomics and found the delivery of flipped material (didactic vs. non-didactic) influenced students’ improvements. They further found performance improvements for the students who attended flipped classes using non-didactic pre-class material. At the same time, Webb et al. [ 14 ] further found non-improvement associated with flipped classes that used didactic pre-class materials; these materials are akin to traditional lectures.
In the context of nursing education, flipped teaching strategy has demonstrated promising and effective results in enhancing student motivation, performance, critical thinking skills, and learning quality. The flipped teaching classrooms were associated with high ratings in teaching evaluations, increased course satisfaction, improved critical thinking skills [ 15 ], improved exam results and learning quality [ 16 ] and high levels of personal, teaching, and pedagogical readiness [ 17 ]. Another study showed that student performance motivation scores especially in extrinsic goal orientation, control beliefs, and self-efficacy for learning and performance were significantly higher in the flipped teaching classroom when compared to the traditional classroom strategy [ 16 ].
Regardless of these important findings, there have been limited studies published about the flipped teaching strategy in Saudi Arabia, particularly among nursing students. Therefore, implementing the flipped teaching strategy in a therapeutic communication course would be effective in academic performance and retention of knowledge. The flipped teaching method will fit best with the goals of a therapeutic communication course as both focus on active learning and student engagement. This approach is well-matched for a therapeutic communication course as it allows students to apply and practice the communication techniques and strategies, they have learned outside of class from the flipped teaching materials and freeing up class time for interactive and experiential activities. The filliped teaching method can provide opportunities for students to apply effective interpersonal communication skills in classes, provide more time to observe students practicing therapeutic communication techniques through role-play, group discussions, and case studies. It also allows instructors to refine and provide individualized feedback and offer real-time guidance to help students improve their interpersonal communication skills.
The current study aims to examine the students’ perception of a teaching innovation based on the use of the flipped teaching strategy in the therapeutic communication course. Further, to compare if there is a difference in students’ academic performance of students who participate in a traditional teaching strategy when compared with students who participate in flipped teaching intervention.
Students who participated in the intervention group perceived a high level of effectiveness of the flipped teaching classroom as a teaching/learning strategy.
There is a significant difference in the mean scores of students’ academic performance between students who participate in a traditional teaching strategy (control group) when compared with those students who participate in flipped teaching classroom (intervention group).
Design of the study
Quantitative method, quasi-experimental design was used in this study. This research study involves implementing a flipped teaching strategy (intervention) to examine the effectiveness of the flipped teaching among the participants in the intervention group and to examine the significant difference in the mean scores of the students’ performance between the intervention and control group.
College of Nursing at one of the educational universities located in Saudi Arabia.
A purposive sampling technique was conducted in this study. This sampling technique allows the researcher to target specific participants who have certain characteristics that are most relevant and informative for addressing the research questions. The advantages of the purposive sampling lie in gathering in-depth, detailed and contextual data from the most appropriate sources and ensure that the study captures a more comprehensive understanding of the concept of interest by considering different viewpoints [ 18 ]. Participants were eligible to participate in this study if they were (1) Enrolled in the undergraduate nursing programs (Nursing or Midwifery Programs) in the College Nursing; (2) Enrolled in Therapeutic Communication Course; (3) at least 18 years old or older. Participant’s data was excluded if 50% of the responses were incomplete. The sample size was calculated using G-Power. The required participants for recruitment to implement this study is 152 participants to reach a confidence level of 95% and a margin error of 5%.
Measurement
Demographic data including the participants’ age and GPA were collected from all the participants. Educational characteristics related to the flipped teaching were collected from the participants in the intervention group including the level of English proficiency, program enrollment, attending previous, attending previous course(s) that used flipped teaching strategy, time spent each week preparing for the lectures, time spent preparing for the course exams, and recommendation for applying flipped teaching in other classes.
The student’s perception of the effectiveness of the flipped teaching strategy was measured by a survey that focused on the effectiveness of flipped teaching. This data was collected only from the participants in the intervention group. The survey involves 14 items that used 5-point Likert-type scale (5 = strongly agree, 4 = agree, 3 = neutral, 2 = disagree and 1 = strongly disagree). The sum of the scores was calculated for the item, a high score indicates a high effectiveness of flipped teaching. The survey was developed by Neeli et al. [ 19 ] and the author was contacted to obtain permission to use the survey. The reliability of the scale was tested using Cronbach alpha, which was 0.91, indicating that the scale has an excellent reliability.
Also, student academic performance was measured for both the intervention and control groups though the average cumulative scores of the assessment methods of students who were enrolled in the Therapeutic Communication Course, given a total of 100. The students’ grades obtained in the course were calculated based grading structure of the Ministry of Education in Saudi Arabia (The Rules and Regulations of Undergraduate Study and Examination).
Ethical approval
Institutional Review Board (IRB) approval (No. 22-0860) was received before conducting the study. Participants were provided with information about the study and informed about the consent process. Informed consent to participate was obtained from all the participants in the study.
Intervention
Therapeutic communication course was taught face-to-face for students enrolled in the second year in the Bachelor of Science in Midwifery and Bachelor of Science in Nursing Programs. There were eight sections for the therapeutic communication course, two of them were under the midwifery program and the remaining (six sections) were under the nursing program. Each section was held once a week in a two-hour length for 10 weeks during the second semester of 2022. Students in all sections received the same materials, contents, and assessment methods, which is considered the traditional teaching strategy. The contents of the course included the following topics: introduction of communication, verbal and written communication, listening skills, non-verbal communication, nurse-patient relationship, professional boundaries, communication styles, effective communication skills for small groups, communication through nursing process, communication with special needs patient, health education and principles for empowering individuals, communication through technology, and trends and issues in therapeutic communication. The course materials, course objectives and learning outcomes, learning resources, and other supporting materials were uploaded to the electronic platform “Blackboard” (A Learning Management System) for all sections to facilitate students’ preparation during classes. The assessment methods include written mid-term examination, case studies, group presentation, and final written examination. The grading scores for each assessment method were also the same for all sections.
The eight course sections were randomly assigned into traditional teaching strategy (control group) or flipped teaching strategy (intervention group). Figure 1 shows random distribution of the course sections. The intervention group ( n = 182) included one section of the Bachelor of Science in Midwifery program ( n = 55 students) and three sections of Bachelor of Science in Nursing program ( n = 127 students). The control group ( n = 173) included one section of the Bachelor of Science in Midwifery program ( n = 50 students) and three sections of Bachelor of Science in Nursing program ( n = 123 students). Although randomization of the participants is not possible, we were able to create comparison groups between participants who received the flipped teaching and traditional teaching strategy. To ensure the consistency of the information given to the students and reduce the variability, the instructors were meeting periodically and reviewed the materials together. More importantly, all students received the same topics and assessment methods as stated in the course syllabus and as mentioned above. The instructors in all sections were required to answer students’ questions, provide clarification to the points raised throughout the semester, and give constructive feedback after the evaluation of each assessment method. Students were encouraged to freely express their opinions on the issues discussed and to share their thoughts when the opinions were inconsistent.

Random Distribution of the Course Sections
The intervention group were taught the course contents by using the flipped teaching strategy. The participants in the intervention group were asked to read the lectures and watch short videos from online sources before coming to classes. Similar materials and links were uploaded by the course instructors into the Blackboard system. During the classes, participants were divided into groups and were given time to appraise research articles and case scenarios related to the topics of the course. During the discussion time, each group presented their answers, and the course instructors encouraged the students to share their thoughts and provided constructive feedback. Questions corresponded to the intended objectives and learning outcomes were posted during the class time in Kahoot and Nearpod platforms as a competition to enhance students’ engagement. By the end of the semester, the flipped teaching survey was electronically distributed to students who were involved in the intervention group to examine the educational characteristics and assess the students’ perceptions about the flipped teaching.
Data collection procedure
After obtaining the IRB approval, the PI sent invitation letters to the potential participants using their official university email accounts. The invitation letter included a Microsoft Forms’ link with the description about the study, aim, research question, and sample size required to conduct the study. All students gave their permission to participate, and informed consent was obtained from them ( N = 355). The link also included questions related to age, GPA, and approval to use their scores from assessment methods for research purposes. The first part of data collection was obtained immediately after the therapeutic communication course was over. The average cumulative scores of all the assessment methods (out of 100) were calculated to measure the students’ academic performance for both the intervention and control groups.
The second part of data collection was conducted after the final exam of the therapeutic communication course ( n = 182). A Microsoft Forms link was sent to the participants in the intervention group only. It included questions related to educational characteristics and students’ perception of the effectiveness of flipped teaching. Students needed a maximum of 10 min to complete the study survey.
Data analysis
Data was analyzed using the SPSS version 27. Descriptive analysis was used to analyze the demographic and educational characteristics and perception of flipped teaching strategy. An independent t-test was implemented to compare the mean scores of the intervention and control groups to examine whether there is a statistically significance difference between both groups. A significance level of p < 0.05 was determined as statistical significance in this study.
The total number of students who enrolled in therapeutic communication course was 355 students. The intervention group included 182 students and the control group included 173 students. The mean age of all participants in the study was 19 years old (M = 19.56, SD = 1.19). The mean GPA was 3.53 (SD = 1.43). Of those enrolled in the intervention group, only 70 out of 182 students completed the survey. Table 1 represents the description of the educational characteristics of the participants in intervention group ( n = 70). Around 65% of the participants reported that their level of English proficiency is intermediate, and they were enrolled in the nursing program. Half of the students had precious courses that used flipped teaching strategy. About one-third of the students indicated that they spent less than 15 min each week preparing for lectures. Around 65% of the students stated that they spent more than 120 min preparing for the course exam. Half of the students gave their recommendation for applying flipped teaching strategy in other courses. The mean score of the students’ performance in Therapeutic Communication course who enrolled in the intervention group is 83.34 (SD = 9.81) and for those who were enrolled in the control group is 75.57 (SD = 9.82).
The students perceived a moderate level of effectiveness of the flipped teaching classroom as a teaching strategy (M = 3.49, SD = 0.69) (Table 2 ). The three highest items that improved students’ perception about the flipped teaching strategy were: flipped classroom session develops logical thinking (M = 3.77, SD = 0.99), followed by flipped classroom session provides extra information (M = 3.68, SD = 1.02), then flipped classroom session improves the application of knowledge (M = 3.64, SD = 1.04). The three lowest items perceived by the students were: Flipped classroom session should have allotted more time for each topic (M = 3.11, SD = 1.07), flipped classroom session requires a long time for preparation and conduction (M = 3.23, SD = 1.04), and flipped classroom session reduces the amount of time needed for study when compared to lectures (M = 3.26, SD = 1.07).
An independent sample T-test was implemented to compare the mean scores of the students’ academic performance between the intervention group ( n = 182) and control group ( n = 173) (Table 3 ). The results of Levene’s test for equality of variances ( p = 0.801) indicated that equal variances assumed, and the assumption of equal variances has not been violated. The significant level value (2-tailed) is p ≤ 0.001, indicating that there is a statistically significant difference in the mean scores of students’ academic performance for the intervention group (M = 83.34, SD = 9.81) and control group (M = 75.57, SD = 9.82). The magnitude of the differences in the means (Mean difference= -7.77%, CI: -10.02 to -5.52) is very small (Eta squared = 0.00035).
Flipped teaching is a learning strategy that engages students in the learning process allowing them to improve their academic performance and develop cognitive skills [ 20 ]. This study investigated the effect of implementing flipped teaching as an interactive learning strategy on nursing students’ performance. Also, the study examined students’ perceptions of integrating flipped teaching into their learning process. Flipped teaching is identified as an interactive teaching strategy that provides an engaging learning environment with immediate feedback allowing students to master the learning content [ 4 , 5 ]. Improvement in the student’s academic performance and development of learning competencies were expected outcomes. The flipped classroom approach aligns with the constructivist theory of education, which posits that students actively construct their own knowledge and understanding through engaging with the content and applying it in meaningful contexts. By providing pre-class materials (e.g., videos, readings) for students to engage with independently, the flipped classroom allows them to build a foundational understanding of the concepts before class, enabling them to actively participate in discussions, problem-solving, and collaborative activities during the class. By shifting the passive acquisition of knowledge to the pre-class phase and dedicating in-class time to active, collaborative, and problem-based learning, the flipped classroom approach creates an environment that fosters deeper understanding, the development of critical thinking and clinical reasoning skills as well as the ability to apply knowledge in clinical practice [ 21 ].
Effectiveness of the flipped teaching on students’ academic performance
The influence of flipped teaching on students’ academic performance was identified by evaluating students’ examination scores. The results of this study indicated that flipped teaching had a significant influence on students’ academic performance ( p = 0.000). This significant influence implies the positive effectiveness of flipped teaching on students’ academic performance (M = 83.34, SD = 9.81) compared to traditional classroom (M = 75.57, SD = 9.82). These results are in line with other researchers regarding improving students’ academic performance [ 7 , 8 , 9 , 10 ]. Qutob’s [ 8 ] study shows that flipped teaching positively influences students’ performance. Preparation for class positively influenced students’ academic performance. The flipped classroom approach is underpinned by the principles of constructivism. These principles emphasize the active role of students in constructing their own understanding of concepts and ideas, rather than passively receiving information [ 21 ].
In a traditional classroom, the teacher typically delivers content through lectures, and students are tasked with applying that knowledge through homework or in-class activities. However, this model often fails to engage students actively in the learning process. In contract,
Flipped classroom requires students to prepare for the class which allows them to be exposed to the learning material before the class. During class time, students are giving opportunities to interact with their classmates and instructors to discuss the learning topic which can positively influencing their academic performance later [ 7 , 9 ]. Furthermore, the flipped classroom approach aligns perfectly with the core tenets of constructivism. Its adherence to the constructivist 5E Instructional Model further demonstrates its grounding in this learning theory. The 5E model, which includes the phases of engagement, exploration, explanation, elaboration, and evaluation, provides a framework for facilitating the active construction of knowledge [ 22 ].
It first sparks student interest and curiosity about the concepts (engagement), then enables students to investigate and experiment with the ideas through hands-on activities and investigations (exploration). This is followed by opportunities for students to make sense of their explorations and construct their own explanations (explanation). The flipped classroom then allows students to apply their knowledge in new contexts, deepening their understanding (elaboration). Finally, the evaluation phase assesses student learning and provides feedback, completing the cycle of constructivist learning [ 22 ]. This alignment with the 5E model, along with the flipped classroom’s emphasis on active learning and create environment that nurtures deeper understanding, the development of higher-order thinking skills, and the ability to transfer learning to real-world contexts.
In this study, one third of the students indicated that the preparation time was less than fifteen minutes a week. According to Vazquez and Chiang [ 10 ], preparation time for classroom should be about 15 to 20 min for each topic. Preparation for class did not take much time but positively influenced students’ academic performance. Furthermore, preparation for class allows students to develop the skills to be independent learners [ 8 ]. Independence in learning develops continuous learning skills, such as long-life learning which is a required competency for nursing. Garcia et al. [ 22 ] found out that focusing on shifting teachers’ practices towards active learning approaches, such as the 5E Instructional Model, can have lasting, positive impacts on students’ conceptual understanding and learning.
Students’ perception of flipped teaching as a teaching strategy
Students’ perception of flipped teaching as a learning strategy was examined using a survey developed by Neeli et al. [ 19 ]. Students recognize flipped teaching as an effective teaching strategy (M = 3.49, SD = 0.69) that had a positive influence on their learning processes and outcomes. Several studies identified the positive influence of flipped teaching on students’ learning process and learning outcomes [ 8 , 19 ]. Flipped teaching provides a problem-based learning environment allowing students to develop clinical reasoning, critical thinking, and a deeper understanding of the subject [ 5 , 8 , 19 , 23 ]. The flipped teaching approach introduces students to the learning materials before class. Class time is then utilized for discussion, hands-on, and problem-solving activities to foster a deeper understanding of the studied subject [ 5 ]. Consequently, flipped teaching provides a problem-based learning environment as it encourages students to be actively engaged in the learning process, work collaboratively with their classmates, and apply previously learned knowledge and skills to solve a problem. The result of this study is consistent with the results from a systematic review conducted by Youhasan et al. [ 5 ]. Implementing flipped teaching in undergraduate nursing education provides positive outcomes on students’ learning experiences and outcomes and prepares them to deal with future challenges in their academic and professional activities [ 5 ].
Implications
The results from this study identified that flipped teaching has a significant influence on students’ academic performance. The results also indicated that students have positive perception of flipped teaching as an interactive learning strategy. Flipped teaching pedagogy could be integrated in nursing curriculum to improve the quality of education process and outcomes which will result in improving the students’ performance. Flipped teaching provides an interactive learning environment that enhances the development of essential nursing competencies, such as communication, teamwork, collaboration, life-long learning, clinical reasoning, and critical thinking. For example, flipped teaching allows students to develop communication skills throughout discussion in the classroom, and collaboration skills by working with their classmate and instructor. In this study, flipped teaching was implemented in a theoretical course (therapeutic communication course). This interactive learning strategy could also be applied in clinical and practice setting for effective and meaningful learning process and outcomes.
Strengths and limitations
This research study reveals the effectiveness of flipped teaching on students’ academic performance. This study used a quasi-experimental design with control and intervention groups to investigate the influence of flipped teaching on nursing education. Nevertheless, this study has limitations. One of the study’s limitations is the lack of randomization, thus causal association between the variables cannot be investigated. In addition, this study used a self-administered survey which may include respondents’ bias; thus, it may affect the results. Also, this study investigated students’ perceptions of flipped teaching as a learning strategy. The results from examining students’ perceptions indicated that students had a positive perception of flipped teaching as it allowed them to develop essential nursing competencies. This study did not focus on identifying and measuring competencies. Therefore, future studies must consider measuring the influence of flipped teaching on students’ ability to acquire nursing competencies, such as critical thinking and clinical reasoning.
Flipped teaching is an interactive learning strategy that depends on students’ preparation of the topic to be interactive learners in the learning environment. Interactive learning environment improves learning process and outcomes. This study indicated that flipped teaching has significant influence on students’ academic performance. Students perceived flipped teaching as a learning strategy that allowed them to acquire learning skills, such as logical thinking and application of knowledge. These skills allow students to have meaningful learning experience. Also, students could apply these skills in other learning content and/or environments, for example, in clinical. Thus, we believe that flipped teaching is an effective learning approach to be integrated in the nursing curriculum to enhance students’ learning experience.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to data privacy but are available from the corresponding author on reasonable request.
Abbreviations
Institutional Review Board
Standard deviation
The level of marginal significance within a statistical test
Confidence Interval of the Difference
Figueiredo AR, Potra TS. Effective communication transitions in nursing care: a scoping review. Ann Med. 2019;51(sup1):201–201. https://doi.org/10.1080/07853890.2018.1560159 .
Article Google Scholar
O’Rae A, Ferreira C, Hnatyshyn T, Krut B. Family nursing telesimulation: teaching therapeutic communication in an authentic way. Teach Learn Nurs. 2021;16(4):404–9. https://doi.org/10.1016/j.teln.2021.06.013 .
Thai NTT, De Wever B, Valcke M. The impact of a flipped classroom design on learning performance in higher education: looking for the best blend of lectures and guiding questions with feedback. Computers Educ. 2017;107:113–26. https://doi.org/10.1016/j.compedu.2017.01.003 .
Özbay Ö, Çınar S. Effectiveness of flipped classroom teaching models in nursing education: a systematic review. Nurse Educ Today. 2021;104922–104922. https://doi.org/10.1016/j.nedt.2021.104922 . 102 (n. Issue).
Youhasan P, Chen Y, Lyndon M, Henning MA. Exploring the pedagogical design features of the flipped classroom in undergraduate nursing education: a systematic review. BMC Nurs. 2021;20(1):50–50. https://doi.org/10.1186/s12912-021-00555-w .
Barbour C, Schuessler JB. A preliminary framework to guide implementation of the flipped classroom method in nursing education. Nurse Educ Pract. 2019;34:36–42. https://doi.org/10.1016/j.nepr.2018.11.001 .
Jordan C, Magrenan A, Orcos L. Considerations about flip education in the teaching of advanced mathematics. Educational Sci. 2019;9(3):227.
Qutob H. Effect of flipped classroom approach in the teaching of a hematology course. PLoS ONE. 2022;17(4):1–8.
Nguyen B, Yu X, Japutra A, Chen C. Reverse teaching: exploring student perceptions of flip teaching. Act Learn High Educ. 2016;17(1):51–61.
Vazquez J, Chiang E. Flipping out! A case study on how to flip the principles of economics classroom. Int Adv Econ Res. 2015;21(4):379–90.
Florence E, Kolski T. Investigating the flipped classroom model in a high school writing course: action research to impact student writing achievement and engagement. TechTrends: Link Res Pract Improve Learn. 2021;65(6):1042–52.
Bahadur G, Akhtar Z. Effect of teaching with flipped classroom model: a meta-analysis. Adv Social Sci Educ Humanit Res. 2021;15(3):191–7.
Google Scholar
Galindo-Dominguez H. Flipped classroom in the educational system: Trend or effective pedagogical model compared to other methodologies? J Educational Technol Soc. 2021;24(3):44–60.
Webb R, Watson D, Shepherd C, Cook S. Flipping the classroom: is it the type of flipping that adds value? Stud High Educ. 2021;46(8):1649–63.
Barranquero-Herbosa M, Abajas-Bustillo R, Ortego-Maté C. Effectiveness of flipped classroom in nursing education: a systematic review of systematic and integrative reviews. Int J Nurs Stud. 2022;135:104327. https://doi.org/10.1016/j.ijnurstu.2022.104327 .
Lelean H, Edwards F. The impact of flipped classrooms in nurse education. Waikato J Educ. 2020;25:145–57.
Youhasan P, Chen Y, Lyndon M, Henning MA. Assess the feasibility of flipped classroom pedagogy in undergraduate nursing education in Sri Lanka: a mixed-methods study. PLoS ONE. 2021;16(11):e0259003. https://doi.org/10.1371/journal.pone.0259003 .
Harris AD, McGregor JC, Perencevich EN, Furuno JP, Zhu J, Peterson DE, Finkelstein J. The use and interpretation of quasi-experimental studies in medical informatics. J Am Med Inf Association: JAMIA. 2006;13(1):16–23. https://doi.org/10.1197/jamia.M1749 .
Neeli D, Prasad U, Atla B, Kukkala SSS, Konuku VBS, Mohammad A. (2019). Integrated teaching in medical education: undergraduate student’s perception.
Baloch MH, Shahid S, Saeed S, Nasir A, Mansoor S. Does the implementation of flipped Classroom Model improve the Learning Outcomes of Medical College Students? A single centre analysis. J Coll Physicians Surgeons–pakistan: JCPSP. 2022;32(12):1544–7.
Robertson WH. The Constructivist flipped Classroom. J Coll Sci Teach. 2022;52(2):17–22.
Garcia I, Grau F, Valls C, Piqué N, Ruiz-Martín H. The long-term effects of introducing the 5E model of instruction on students’ conceptual learning. Int J Sci Educ. 2021;43(9):1441–58.
Chu TL, Wang J, Monrouxe L, Sung YC, Kuo CL, Ho LH, Lin YE. The effects of the flipped classroom in teaching evidence based nursing: a quasi-experimental study. PLoS ONE. 2019;14(1):e0210606.
Download references
Acknowledgements
The authors are grateful for the facilities and other support given by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R447), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia.
This research was funded by Princess Nourah bint Abdulrahman University Researchers Supporting Project number (PNURSP2024R447), Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Author information
Authors and affiliations.
Nursing Management and Education Department, College of Nursing, Princess Nourah bint Abdulrahman University, P.O. Box 84428, Riyadh, 11671, Saudi Arabia
Shaherah Yousef Andargeery, Rania Ali Alhalwani, Shorok Hamed Alahmedi & Waad Hasan Ali
Medical-Surgical Nursing Department, College of Nursing, Princess Nourah bint Abdulrahman University, P.O. Box 84428, Riyadh, 11671, Saudi Arabia
Hibah Abdulrahim Bahri
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, H.B, S.Y.A, W.A.; methodology, S.Y.A., S.H.A.; validation, S.Y.A.; formal analysis, S.Y.A.; resources, H.B, S.Y.A, W.A, R. A.; data curation, S.Y.A, S.H.A.; writing—original draft preparation, R.A, H.B, S.Y.A., S.H.A, W.A; writing—review and editing, R.A, H.B, S.Y.A, S.H.A, W.A; supervision, R.A, H.B, S.Y.A, S.H.A.; project administration, R.A, S.Y.A, S.H.A.; funding acquisition, S.Y.A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Hibah Abdulrahim Bahri .
Ethics declarations
Institutional review board.
Institutional Review Board (IRB) in Princess Nourah bint Abdulrahman University, approval No. (22-0860).
Informed consent
Informed consents were obtained from all study participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Andargeery, S.Y., Bahri, H.A., Alhalwani, R.A. et al. Using a flipped teaching strategy in undergraduate nursing education: students’ perceptions and performance. BMC Med Educ 24 , 926 (2024). https://doi.org/10.1186/s12909-024-05749-9
Download citation
Received : 26 February 2024
Accepted : 05 July 2024
Published : 26 August 2024
DOI : https://doi.org/10.1186/s12909-024-05749-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Flipped teaching
- Active learning
- Teaching strategy
- Nursing education
- Undergraduate nursing education
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Using unfolding case studies to develop critical thinking skills in baccalaureate nursing students: A pilot study
Affiliation.
- 1 University of Wisconsin Oshkosh, College of Nursing, 800 Algoma Blvd, Oshkosh, WI, United States of America. Electronic address: [email protected].
- PMID: 32717696
- DOI: 10.1016/j.nedt.2020.104542
Background: Research has consistently demonstrated that new graduate nurses do not possess sufficient critical thinking skills when they transition to clinical practice. Unfolding case studies encourage students to participate in a number of critical thinking skills including information-seeking, logical reasoning, and analyzing of clinical data.
Objective: The aim of this study was to determine how the use of unfolding case studies as a learning modality affected baccalaureate students' critical thinking skills in their Adult Health Theory course. The researcher compared course examination scores earned by nursing students who were taught using traditional case studies to scores obtained by nursing students who completed unfolding case studies.
Setting: The pilot study took place at a moderate-sized comprehensive university in Wisconsin.
Design: A non-experimental correlational design using course examination scores data was employed to examine how the use of unfolding case studies as a learning modality affected baccalaureate students' critical thinking skills in their Adult Health Theory course.
Participants: A total of 160 students comprised the intervention group while an additional 142 students represented the control group in the study.
Methods: An independent-samples t-test was performed to explore differences in mean scores between the intervention and control groups.
Results: Results of the t-test indicate that mean examination scores were significantly higher for the intervention group (M = 234.9, SD = 13.1) than for the control group (M = 228.2, SD = 13.3); t(299) =, p < .001.
Conclusions: Results of this study suggest that unfolding case studies more effectively develop students' critical thinking skills than do a more traditional, static case study.
Keywords: Baccalaureate education; Critical thinking; Nursing students; Unfolding case study.
Copyright © 2020 Elsevier Ltd. All rights reserved.
PubMed Disclaimer
Conflict of interest statement
Declaration of competing interest The author declares no conflicts of interest.
Similar articles
- Effects of unfolding case-based learning on academic achievement, critical thinking, and self-confidence in undergraduate nursing students learning health assessment skills. Ma C, Zhou W. Ma C, et al. Nurse Educ Pract. 2022 Mar;60:103321. doi: 10.1016/j.nepr.2022.103321. Epub 2022 Mar 8. Nurse Educ Pract. 2022. PMID: 35287002
- The impact of applying unfolding case-study learning on critical care nursing students' knowledge, critical thinking, and self-efficacy; a quasi-experimental study. Kassabry M, Al-Kalaldeh M, Ayed A, Abu-Shosha G. Kassabry M, et al. Nurse Educ Pract. 2024 Jul;78:104015. doi: 10.1016/j.nepr.2024.104015. Epub 2024 Jun 3. Nurse Educ Pract. 2024. PMID: 38852273
- Effects of using videotaped vignettes on enhancing students' critical thinking ability in a baccalaureate nursing programme. Chau JP, Chang AM, Lee IF, Ip WY, Lee DT, Wootton Y. Chau JP, et al. J Adv Nurs. 2001 Oct;36(1):112-9. doi: 10.1046/j.1365-2648.2001.01948.x. J Adv Nurs. 2001. PMID: 11555055
- The Effect of Concept Maps on Undergraduate Nursing Students' Critical Thinking. Garwood JK, Ahmed AH, McComb SA. Garwood JK, et al. Nurs Educ Perspect. 2018 Jul/Aug;39(4):208-214. doi: 10.1097/01.NEP.0000000000000307. Nurs Educ Perspect. 2018. PMID: 29629932 Review.
- Learning styles and critical thinking relationship in baccalaureate nursing education: a systematic review. Andreou C, Papastavrou E, Merkouris A. Andreou C, et al. Nurse Educ Today. 2014 Mar;34(3):362-71. doi: 10.1016/j.nedt.2013.06.004. Epub 2013 Jul 3. Nurse Educ Today. 2014. PMID: 23830067 Review.
- Perspectives of Nursing Students on Hybrid Simulation-Based Learning Clinical Experience: A Text-Mining Analysis. Saitoh A, Yokono T, Sakagami M, Kashiwa M, Abeywickrama HM, Uchiyama M. Saitoh A, et al. Nurs Rep. 2024 Apr 18;14(2):988-999. doi: 10.3390/nursrep14020074. Nurs Rep. 2024. PMID: 38651486 Free PMC article.
- A mixed methods study using case studies prepared by nursing students as a clinical practice evaluation tool. Palmar-Santos AM, Oter-Quintana C, Olmos R, Pedraz-Marcos A, Robledo-Martin J. Palmar-Santos AM, et al. Nurs Open. 2023 Sep;10(9):6592-6601. doi: 10.1002/nop2.1919. Epub 2023 Jun 20. Nurs Open. 2023. PMID: 37340631 Free PMC article.
- Scaffolding as active learning in nursing education. Coffman S, Iommi M, Morrow K. Coffman S, et al. Teach Learn Nurs. 2023 Jan;18(1):232-237. doi: 10.1016/j.teln.2022.09.012. Epub 2022 Nov 2. Teach Learn Nurs. 2023. PMID: 36339966 Free PMC article.
- Effectiveness of case scenario-based teaching to transition international Master of Public Health students specialising in health promotion from memorization to critical thinking. Hosseinzadeh H, Ratan ZA, Shnaigat M, Edwards J, Verma I, Niknami M, Dadich A. Hosseinzadeh H, et al. Health Promot J Austr. 2022 Oct;33 Suppl 1(Suppl 1):39-49. doi: 10.1002/hpja.631. Epub 2022 Jun 28. Health Promot J Austr. 2022. PMID: 35714044 Free PMC article.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Elsevier Science
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- DOI: 10.52902/kjsc.2024.28.121
- Corpus ID: 269039411
Correlation between Communication Competence, Problem-Solving Skills, Clinical Competence, and Critical Thinking Competence on Person-Centered Care Competence of Nursing Students in who Experienced Clinical Practice
- Mi Young Moon
- Published in Forum of Public Safety and… 30 March 2024
- Education, Medicine
Related Papers
Showing 1 through 3 of 0 Related Papers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- JMIR Res Protoc
- v.11(4); 2022 Apr

Simulation-Based Learning Supported by Technology to Enhance Critical Thinking in Nursing Students: Protocol for a Scoping Review
Hege vistven stenseth.
1 Lovisenberg Diaconal University College, Oslo, Norway
Simen Alexander Steindal
2 Faculty of Health Studies, VID Specialized University, Oslo, Norway
Marianne Trygg Solberg
Mia alexandra Ølnes, andrea mohallem.
3 Faculdade Israelita de Ciências da Saúde Albert Einstein, São Paulo, Brazil
Anne Lene Sørensen
Camilla strandell-laine.
4 Faculty of Health and Welfare, Novia University of Applied Sciences, Turku, Finland
Camilla Olaussen
Caroline farsjø aure, fernando riegel.
5 Federal University of Rio Grande do Sul, Porto Alegre, Rio Grande do Sul, Brazil
Ingunn Pedersen
6 Nord University, Namsos, Norway
Jaroslav Zlamal
Jussara gue martini.
7 Federal University of Santa Catarina, Florianópolis, Santa Catarina, Brazil
Paula Bresolin
Silje christin wang linnerud, andréa aparecida gonçalves nes, associated data.
Search strategy in Ovid MEDLINE.
Critical thinking is a crucial skill in the nursing profession, so teaching strategies and methodology must be carefully considered when training and preparing nursing students to think critically. Studies on simulation-based learning supported by technology are increasing in nursing education, but no scoping reviews have mapped the literature on simulation-based learning supported by technology to enhance critical thinking in nursing students.
The proposed scoping review aims to systematically map research on the use of simulation-based learning supported by technology to enhance critical thinking in nursing students.
The proposed scoping review will use the framework established by Arksey and O’Malley and will be reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews. A systematic, comprehensive literature search was performed in the LILACS, ERIC, MEDLINE, EMBASE, PsycINFO, and Web of Science databases. Pairs of authors independently selected the articles by screening titles, abstracts, full-text papers, and extract data. The data will be analyzed and thematically categorized.
The development of a comprehensive and systematic search strategy was completed in June 2021. The database searches were performed in July 2021, and the screening of titles and abstracts was completed in September 2021. Charting the data began in February 2022. Analysis and synthesis will be performed sequentially, and the scoping review is expected to be complete by May 2023.
Conclusions
The results of this proposed scoping review may identify gaps in the literature and provide an overview of research on the topic of simulation-based learning supported by technology to enhance critical thinking in nursing students. The research may identify nursing students’ reported barriers and enablers for learning critical thinking skills through simulation-based learning supported by technology, and the results may help educators enhance their educational approach through knowledge of students’ firsthand experiences and further development of successful teaching strategies in nursing education.
International Registered Report Identifier (IRRID)
DERR1-10.2196/36725
Introduction
Educational approaches for active learning in nursing education.
Active teaching methods are recognized as educational approaches by which teachers support students in the development of critical thinking (CT) [ 1 , 2 ]. One strategy for developing CT is to allow nursing students to actively participate in the learning process with the support of technology. Simulation-based learning (SBL) is a teaching strategy that may enhance the integration of theoretical and practical knowledge and the ability to reflect and to give and receive feedback [ 3 , 4 ]. Scientific evidence reveals that active learning strategies are more effective for developing CT skills for students in higher education than passive learning under traditional methods, such as lectures [ 2 , 5 ]. With the advent of the COVID-19 pandemic and its resultant social distancing requirements, the interest in, demand for, and use of technological solutions have increased in nursing education [ 6 ].
Critical Thinking in Nursing Education
CT is a crucial skill and a fundamental component of nurses’ daily professional responsibilities. Nurses require CT skills to analyze, summarize, and evaluate information and initiate action. CT skills enable nurses to manage uncertainties in nursing practice and contribute to safe and effective care across diverse clinical settings [ 7 - 9 ]. Several definitions and terms for CT are used interchangeably in nursing studies, research, and nursing curricula [ 10 , 11 ]. The core components of CT are to be able to analyze, evaluate, and investigate [ 12 ]. Because there is no consensus on the definition of CT in nursing education research, research often looks to other disciplines like philosophy, psychology, and education for clear definitions [ 10 ]. A frequently cited definition in nursing studies is the one by a consensus statement of the American Philosophical Association, which defines CT as “a judgment which is purposeful and self-regulatory and results in a process of interpretation, analysis, evaluation, and inference, as well as explanation of the evidential, conceptual, methodological, criteriological, or contextual considerations upon which that judgment is based” [ 13 ]. According to Riegel and Crossetti [ 14 ], CT is driven by internal motivation, which is reflective in nature and involves self-monitoring and self-correction. This process develops a reflective judgment on what to do, believe, or make sense of in any context.
Several distinct terms are currently used in studies exploring the outcome of CT in SBL, such as clinical problem-solving , clinical decision-making , clinical reasoning, and handling clinical deterioration [ 4 , 11 , 15 ].
In this proposed scoping review, the terms clinical decision-making , analytical thinking , creative thinking , problem-solving , reflective thinking , diagnostic reasoning, and clinical judgment are all potential synonyms of CT. Teaching CT is the responsibility of nurse educators [ 16 ], and teaching strategies and methodology must be carefully considered to meet the purpose of preparing pre- and postgraduate nursing students to think critically and manage the uncertainty of the nursing profession [ 10 , 12 , 17 ].
Simulation-Based Learning
Reflection and CT skills may be developed through learning activities with high-quality teaching strategies, such as SBL [ 7 , 10 ]. SBL facilitates learning in a safe environment with the opportunity to gain experience and practice without the risk of doing harm to the patient [ 3 ]. Bland et al [ 18 ] define SBL as “a dynamic process involving the creation of a hypothetical opportunity that incorporates an authentic representation of reality, facilitates active student engagement, and integrates the complexities of practical and theoretical learning with opportunity for repetition, feedback, evaluation, and reflection.” SBL is commonly founded on social constructivism and learning theory, which view knowledge as being constructed in a social context [ 19 ]. Within this framework, the traditional teacher-student relationship, in which knowledge is transferred from teacher to student, shifts to a learner-centered, teacher-guided approach [ 9 , 20 ]. SBL can potentially replicate clinical practice, in which the learner must employ clinical reasoning with cognitive, psychomotor, and affective skills [ 15 ]. According to the International Nursing Association for Clinical Simulation and Learning (INACSL) Standards Committee [ 21 ] self-monitoring, conscious reflection, and insightfulness occur in SBL through debriefing, feedback, and guided reflection. This process may help learners understand their own actual practice; identify knowledge gaps; increase competence; and support the transfer of knowledge, skills, and attitudes. Learners’ insights may be developed through conscious reflection that connects actions, thoughts, and beliefs.
In traditional SBL, high-tech modalities, including advanced simulators (eg, life-size patient manikins), replicate real patients and settings in health care [ 22 ]. In simulation research, the term fidelity traditionally describes the degree to which the advanced simulator looks, acts, and feels like a human being, with an emphasis on technological features and advances that enhance the physical resemblance [ 23 ].
Other simulation research focuses on different aspects of realism with a physical, semantic, and phenomenal dimension, but what constitutes realism depends on what makes sense for the individual in a given context or situation [ 24 , 25 ].
To enhance learning, scholars recommend focusing on learner engagement and correspondence between the simulation technology and the surroundings (the applied context) [ 23 ].
Simulation-Based Learning Supported by Technology
Technological solutions to support SBL in nursing education are continually expanding [ 4 ], ranging from advanced physical simulators with human features and responses to computer and online games, simulation games, and virtual reality (VR). Simulation gaming for nursing education has emerged in many forms and reportedly offers potential as a teaching strategy for stimulating CT [ 26 , 27 ]. Producers offer specific software that enables virtual computer simulations, and there are online solutions including computer games, virtual simulations, and VR intended for nursing education. Immersive VR uses special headsets that immerse the student in a virtual world [ 28 - 30 ] and has the advantage of replicating the clinical environment and patient-nurse interactions in situations designed to promote specific learning outcomes [ 26 ]. Cant and Cooper [ 29 ] conclude that internet simulation measures up to other simulation approaches and will likely be a large part of the nursing curriculum in the near future.
SBL supported by technology can ensure equitable learning opportunities by providing the same content and learning environment to all students. The potential for individual training and multiple iterations through technology makes SBL resource-efficient due to its low staff costs [ 27 , 31 , 32 ]. Due to technological advances, SBL no longer requires a physical meeting space. In virtual meetings, students and teachers can discuss and reflect on dilemmas and situations experienced in simulated or clinical practice. According to the principles of metacognition, this can encourage CT. Technology-supported learning methods can stimulate dialogue between students and teachers, adjusting students’ learning focus and ensuring an accurate assessment of learning outcomes [ 33 ]. Importantly, in the context of current and future pandemics, technology provides an environment for teaching vital CT skills that is contactless and thus at low risk of spreading infectious disease [ 32 ].
Background for the Scoping Review
A literature review by Adib-Hajbaghery and Sharifi [ 34 ] found uncertainties about the effect of SBL on the CT of nursing students and nurses. Their findings are supported by a recent systematic review that examined extant evidence of simulation’s effectiveness in promoting clinical reasoning skills in nursing education [ 15 ]. The authors of this systematic review conclude that insufficient evidence exists to form conclusions. They found a lack of substantial evidence for the cause-effect relationship of simulation training and CT due to the great heterogeneity of the studies, including diverse methods, scenarios, and measurement instruments [ 15 , 34 ]. The heterogeneity of studies makes it challenging to compare results and reach a consensus regarding SBL’s effect on CT. Systematic reviews have also noted a lack of comparative studies that could report a quantitative, overall effect of SBL [ 30 , 34 ]. A systematic review of randomized controlled trials (RCTs) found that SBL may improve the acquisition of CT knowledge as well as students’ reported satisfaction with teaching, but the authors note a lack of unambiguous evidence of SBL’s effectiveness [ 35 ].
Reviews have also examined the use of technology in nursing education and SBL with diverse outcomes. A scoping review by Duff et al [ 28 ] examined the use of online virtual simulation to enhance clinical reasoning in the education of health care professionals and found online virtual simulation to be comparable or superior to traditional simulation. However, only 3 of the 12 included studies related to nursing education.
A systematic mapping review by Plotzky et al [ 32 ] examined the use of VR in nursing education, but the review was limited to the use of VR technology from didactic and technical perspectives and did not report on the outcome of CT. According to a recent systematic review, VR provides educational outcomes similar or superior to traditional SBL practices, but the evidence is limited [ 36 ]. Another literature review concluded that most evidence indicates that virtual simulation can effectively improve skills, learning, and CT in nursing education [ 4 ], but CT was the least explored outcome, and the search used only two databases, PubMed and CINAHL. Moreover, only articles in English were included, which is an important limitation of the results.
The identified reviews did not thoroughly examine the range and use of technology in SBL to enhance nursing students’ CT skills. Furthermore, the identified reviews mainly included research presented in the English language, except two reviews that included studies in Farsi and German. A broad, comprehensive literature review, such as a scoping review that includes papers in several languages (English, Portuguese, Spanish, and the Scandinavian languages) and employs diverse research methods will enable us to examine the nature and range of the currently available research and to identify potential gaps in the research literature [ 37 ]. To our knowledge, no scoping review has examined the range of technology used in SBL and how it is used to enhance nursing students’ CT skills.
Consequently, this scoping review aims to systematically map research on the use of SBL supported by technology to enhance CT in nursing students. The results may identify potential gaps in research and inform further research on this topic.
Identifying the Research Questions
The scoping review will answer the following research questions:
- What is the range of technology used in SBL to enhance CT skills in nursing education?
- How is technology used in SBL to enhance CT skills in nursing education?
- What do nursing students report as perceived barriers and enablers to enhance CT skills in SBL supported by technology?
Overview Of Method for Conducting the Scoping Review
The proposed scoping review will follow Arksey and O´Malley´s [ 37 ] framework, which includes the following steps: (1) identifying the research questions; (2) identifying relevant studies; (3) selecting studies; (4) charting the data; and (5) collating, summarizing, and reporting the results. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews will guide the reporting of the proposed review [ 38 ]. The reporting of this protocol is guided by the PRISMA Protocol (PRISMA-P) [ 39 ].
Identifying Relevant Studies
The Sample, Phenomenon of Interest, Design, Evaluation, and Research (SPIDER) framework determined the inclusion and exclusion criteria as outlined in Table 1 [ 40 ].
Eligibility criteria according to the Sample, Phenomenon of Interest, Design, Evaluation, and Research (SPIDER) framework.
| Criterion | Inclusion | Exclusion |
| Sample (S) | ||
| Phenomenon of interest (PI) | supported by technology to stimulate CT , clinical decision-making, analytical thinking, creative thinking, problem solving, reflective thinking, diagnostic reasoning, or clinical judgement in educational/institutional contexts. | |
| Design (D) | | N/A |
| Evaluation (E) | | |
| Research type (R) |
a SBL: simulation-based learning.
b CT: critical thinking.
c N/A: not applicable.
Selecting Studies
A systematic search was conducted in the LILACS, ERIC, CINAHL, MEDLINE, EMBASE, PsycINFO, and Web of Science databases on June 28, 2021. Each database was searched from its inception. The database search will be updated approximately 3 months prior to publication.
The search strategy in Ovid MEDLINE, using Medical Subject Headings and text words, was designed by the first research librarian (author MAØ) in collaboration with the rest of the research team and embraced three elements: (1) SBL, (2) technology, and (3) nursing students and nursing education. A second research librarian (KLM) reviewed the search strategy using the Peer Review of Electronic Search Strategies (PRESS) checklist [ 41 ]. The search strategy in Ovid MEDLINE is provided in Multimedia Appendix 1 . We also performed manual searches in the reference lists of the included papers. We did not perform forward tracking (citation searches). We will conduct the entire search a second time around 3 months prior to submission; most of these studies will probably be identified without using forward tracking.
MAØ exported the identified citations into EndNote to remove duplicates using the method described in Bramer et al [ 42 ], and the citations were then exported to the web application Rayyan for storage, organization, and blinding of the study selection process. A pilot test of 10% of the citations to screen titles and abstracts was performed independently by authors HVS and AAGN, who concluded that the eligibility criteria did not require modification. Pairs of authors (HVS-CFA, SCWL-SAS, MTS-JZ, AGCM-FR, PB-JGM, ALS-CSL, CO-HVS, and IP-AAGN) independently screened paper titles and abstracts to assess whether they met the inclusion criteria. When there was any doubt regarding inclusion, a third author independently assessed the full-text paper, and the decision was based on a negotiated consensus. Further, the same pairs of authors will independently assess whether the full-text papers meet the inclusion criteria. When there is any doubt regarding inclusion, a third author will independently assess the full-text paper, and the decision will be based on a negotiated consensus. The reasons for excluding full-text papers will be recorded, and the study selection process will be recorded using the PRISMA 2020 flow diagram.
Charting the Data
A standardized data collection form will be developed in Microsoft Word for data extraction from the included papers, including authors, year, country, aim, sample, design, technology, simulation procedures, scenario design, and results related to the research question. The data collection form will be piloted by HVS and AAGN on up to five of the included papers. Their experiences will be discussed with the entire research team, and the data collection form may be revised.
Pairs of authors will extract the data, with one author extracting the data and the other checking its accuracy. Disagreement among pairs of authors will be resolved by an assessment by a third author, and agreement will be based on negotiated consensus.
Collating, Summarizing, and Reporting the Results
HVS, SAS, MTS, and AAGN will analyze the results from the included papers and will use an inductive approach to organize the results thematically, a method previously used in scoping reviews [ 43 , 44 ]. The results extracted from the included papers will be read several times to identify patterns of similarities and differences related to the research questions, and these patterns will be organized in thematic groupings. The preliminary thematic groupings will be discussed with the rest of the research team, and a frequency table showing which papers appear in which thematic groupings will be created. Any new findings from the replicated search will be analyzed to see if they fit according to the thematic groups or if new thematic groupings arise.
Ethics Approval
No ethical board approval is necessary to conduct this scoping review.
The development of a comprehensive, systematic search strategy was completed in June 2021. The database searches were performed in July 2021, and the screening of titles and abstracts was completed in September 2021. Assessment of full-text papers, charting of the data, and summarizing the results began in February 2022. We anticipate that the scoping review will be completed by May 2023.
The results of the proposed scoping review will identify and provide an overview of the research on using SBL supported by technology to enhance CT in nursing students. This scoping review may also identify the variety of technological solutions available for nursing education and describe how they are used to enhance the development of nursing students’ CT skills. Scoping searches have found reviews on the topic of simulation and CT in nursing education [ 15 , 30 , 34 , 35 ], but those reviews do not specifically report on the use of technology to support SBL to enhance CT. Reviews on SBL technologies have also been identified, which often investigate one type of technology or compare the use of technology to traditional SBL [ 27 , 29 , 31 ].
The outcome of CT is present, but not as the primary outcome for nursing students [ 28 ]. The identified reviews do not sufficiently report on the range of technology used and how technology is used in SBL to enhance CT skills in nursing students. Furthermore, the reviews do not adequately reference the outcome of enhancement of CT in nursing students. Strengths and limitations will be thoroughly examined and reported in the proposed scoping review. Limitations may be related to the inclusion criteria, by only including research studies and thus excluding grey literature. Mapping research in multiple languages may add strength to this proposed scoping review, as the exclusion of studies published in other language than English was reported as a limitation in previous scoping reviews [ 45 ].
Identifying the status of and gaps in the research in this field may contribute to future research and further the development of successful teaching strategies in nursing education. The findings may inform educators’ decisions when choosing technology to support the application of SBL, and identifying nursing students’ barriers or enablers to learning CT skills through technology-supported SBL may help educators devise their educational approaches. The results of this scoping review may also interest technology developers and guide the further development of technology-based solutions for SBL aimed at enhancing nursing students’ CT in nursing education. The results of this proposed scoping review will be disseminated through publication in relevant peer-reviewed journals in educational or nursing-specific contexts.
Acknowledgments
We acknowledge Kari Larsen Mariussen for peer reviewing the search strategy.
This research was funded by the research group Educational Research Focusing on Competence Development and Quality in Nursing Education at Lovisenberg Diaconal University College, Oslo, Norway. The authors did not receive any grants from any commercial, public, or nonprofit funding agency.
Abbreviations
| CT | critical thinking |
| INACSL | International Nursing Association for Clinical Simulation and Learning |
| PRESS | Peer Review of Electronic Search Strategies |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PRISMA-P | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols |
| SBL | simulation-based learning |
| SPIDER | Sample, Phenomenon of Interest, Design, Evaluation, and Research |
| VR | virtual reality |
Multimedia Appendix 1
Authors' Contributions: HVS, SAS, MTS, and AAGN contributed to developing the protocol. HVS drafted the manuscript’s Introduction, Background, Results, and Discussion sections, and SAS drafted the Methods. All the aforementioned authors contributed to reading and editing the manuscript, and the extended group of authors was invited to read and review the draft. All authors read and approved the final version of the manuscript.
Conflicts of Interest: None declared.
- Skip to main content
Update your browser for the best possible experience
As of January 1st, 2020, Internet Explorer (versions 11 and below) is no longer supported by Evolve. To get the best possible experience using Evolve, we recommend that you use another web browser. See the browsers we support. .

IMAGES
COMMENTS
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
The concepts from an escape room are a great way to deliver opportunities for students to practice this skill and can be provided economically and easily. Being creative in managing these concepts will offer an exciting chance to introduce critical thinking for your students. Nursing Education Perspectives42 (6):E145-E146, November/December 2021.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
To develop critical thinking skills, you have to be curious and inquisitive." ... Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient's overall well-being. Learners also ...
To help new nurses develop critical-thinking skills, the professional development resources provider Lippincott Solutions recommended nurse educators focus on the following in the classroom: Promoting interactions. Collaboration and learning in group settings help nursing students achieve a greater understanding of the content.
2. Meeting with Colleagues: Collaborative Learning for Critical Thinking. Regular interactions with colleagues foster a collaborative learning environment. Sharing experiences, discussing diverse viewpoints, and providing constructive feedback enhance critical thinking skills. Colleagues' insights can challenge assumptions and broaden ...
Abstract. Nursing students should be challenged to implement critical thinking decisions regarding conclusions they implement for patient care. This article reinforces common techniques and introduces new practices to teach critical thinking. Many ways are currently recognized utilizing an assortment of techniques.
The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation. "One of the fundamental principles for developing critical thinking is the nursing process," Vest says. "It needs to be a lived experience in the learning environment.". Nursing students often find that there are multiple correct ...
Nursing regulatory bodies worldwide such as the Nursing and Midwifery Council of Ghana and the South African Nursing Council recognize critical thinking (CT) as crucial for nurses. These bodies require that nursing curricula promote CT skills of students (Dozier et al., 2021 ; Gholami et al., 2016 ).
Building critical thinking skills is one of the most important outcomes in the clinical setting for nursing students. Collaboration with nursing faculty during the clinical rotation can ease the burden on direct care nurses and facilitate a positive learning experience for the student. The nursing profession continues to experience several ...
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment. ... For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted. 2. Complex ...
In Closing. By incorporating these questions into your clinical paperwork or as clinical questions to put in your repertoire to ask students in the clinical setting, critical thinking can be strengthened and developed. Don't make clinical education and the teaching of critical thinking so difficult. Keep it simple by drilling deep and ...
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
The importance of nurses' critical thinking skills in improving clinical decision-making is well known (Lee et al., 2017; Ludin, 2018). It has been emphasized that critical thinking and. Conclusion. This study supports the need for different learning methods for developing the nursing students' critical thinking and clinical decision-making level.
Clinical judgment. Clinical judgment results in a student's conclusions after making a holistic assessment that correctly interprets clinical data to determine the best response. It is an outcome that depends on critical thinking, clinical reasoning, and intuition (Rischer, 2021). In nursing, for example, strong clinical judgment involves ...
Clinical simulation was used to develop nursing students' clinical reasoning in evaluating wounds and their treatments , to evaluate and compare the perception of stressors, with the goal of determining whether simulations promote students' self-evaluation and critical-thinking skills , and also to evaluate the impact of multiple ...
Nursing students in order to learn and apply critical thinking should develop independence of thought, fairness, perspicacity in personal and social level, humility, spiritual courage, integrity, perseverance, self-confidence, interest for research and curiosity. Critical thinking is an essential process for the safe, efficient and skillful ...
This study supports the need for different learning methods to develop nursing students' critical thinking and clinical decision-making levels. It is seen that there is a need for revision in the delivery of education and training in nursing schools, taking into account extraordinary situations (distance education, etc.) as in the COVID-19 ...
Background:The COVID-19 pandemic may have inhibited the development of critical thinking and emotional intelligence of nursing students due to the transition from traditional to online learning env...
5.1. Setting. The study was conducted in classroom settings of an undergraduate nursing programme in a public university in Ghana. As a school in a developing country, there are constraints such as logistical inadequacies and lack of adequate qualified faculty, which could inhibit meaningful learning experience towards CT skills development of students existed.
Flipped teaching is an interactive learning strategy that actively engages students in the learning process. Students have an active role in flipped teaching as they independently prepare for the class. Class time is dedicated to discussion and learning activities. Thus, it is believed that flipped teaching promotes students' critical thinking, communication, application of knowledge in real ...
Background: Research has consistently demonstrated that new graduate nurses do not possess sufficient critical thinking skills when they transition to clinical practice. Unfolding case studies encourage students to participate in a number of critical thinking skills including information-seeking, logical reasoning, and analyzing of clinical data.
It is necessary to induce nursing students to use a lot of volunteer programs in order to increase their person-centered care competence, and it is necessary to develop and actively guide convergence extracurricular activities linked to subjects. Purpose: This study is a descriptive research study conducted to identify the relationship and influencing factors between communication competence ...
Active teaching methods are recognized as educational approaches by which teachers support students in the development of critical thinking (CT) [1,2]. One strategy for developing CT is to allow nursing students to actively participate in the learning process with the support of technology.
Evolve is a one-stop online portal for healthcare educators and students to access and purchase all of their Elsevier digital teaching & learning materials