- LOGIN / FREE TRIAL

‘Racism absolutely must not be tolerated’
STEVE FORD, EDITOR
- You are here: COPD

Diagnosis and management of COPD: a case study
04 May, 2020
This case study explains the symptoms, causes, pathophysiology, diagnosis and management of chronic obstructive pulmonary disease
This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient’s associated pathophysiology. Diagnosis involves spirometry testing to measure the volume of air that can be exhaled; it is often performed after administering a short-acting beta-agonist. Management of chronic obstructive pulmonary disease involves lifestyle interventions – vaccinations, smoking cessation and pulmonary rehabilitation – pharmacological interventions and self-management.
Citation: Price D, Williams N (2020) Diagnosis and management of COPD: a case study. Nursing Times [online]; 116: 6, 36-38.
Authors: Debbie Price is lead practice nurse, Llandrindod Wells Medical Practice; Nikki Williams is associate professor of respiratory and sleep physiology, Swansea University.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
Introduction
The term chronic obstructive pulmonary disease (COPD) is used to describe a number of conditions, including chronic bronchitis and emphysema. Although common, preventable and treatable, COPD was projected to become the third leading cause of death globally by 2020 (Lozano et al, 2012). In the UK in 2012, approximately 30,000 people died of COPD – 5.3% of the total number of deaths. By 2016, information published by the World Health Organization indicated that Lozano et al (2012)’s projection had already come true.
People with COPD experience persistent respiratory symptoms and airflow limitation that can be due to airway or alveolar abnormalities, caused by significant exposure to noxious particles or gases, commonly from tobacco smoking. The projected level of disease burden poses a major public-health challenge and primary care nurses can be pivotal in the early identification, assessment and management of COPD (Hooper et al, 2012).
Grace Parker (the patient’s name has been changed) attends a nurse-led COPD clinic for routine reviews. A widowed, 60-year-old, retired post office clerk, her main complaint is breathlessness after moderate exertion. She scored 3 on the modified Medical Research Council (mMRC) scale (Fletcher et al, 1959), indicating she is unable to walk more than 100 yards without stopping due to breathlessness. Ms Parker also has a cough that produces yellow sputum (particularly in the mornings) and an intermittent wheeze. Her symptoms have worsened over the last six months. She feels anxious leaving the house alone because of her breathlessness and reduced exercise tolerance, and scored 26 on the COPD Assessment Test (CAT, catestonline.org), indicating a high level of impact.
Ms Parker smokes 10 cigarettes a day and has a pack-year score of 29. She has not experienced any haemoptysis (coughing up blood) or chest pain, and her weight is stable; a body mass index of 40kg/m 2 means she is classified as obese. She has had three exacerbations of COPD in the previous 12 months, each managed in the community with antibiotics, steroids and salbutamol.
Ms Parker was diagnosed with COPD five years ago. Using Epstein et al’s (2008) guidelines, a nurse took a history from her, which provided 80% of the information needed for a COPD diagnosis; it was then confirmed following spirometry testing as per National Institute for Health and Care Excellence (2018) guidance.
The nurse used the Calgary-Cambridge consultation model, as it combines the pathological description of COPD with the patient’s subjective experience of the illness (Silverman et al, 2013). Effective communication skills are essential in building a trusting therapeutic relationship, as the quality of the relationship between Ms Parker and the nurse will have a direct impact on the effectiveness of clinical outcomes (Fawcett and Rhynas, 2012).
In a national clinical audit report, Baxter et al (2016) identified inaccurate history taking and inadequately performed spirometry as important factors in the inaccurate diagnosis of COPD on general practice COPD registers; only 52.1% of patients included in the report had received quality-assured spirometry.
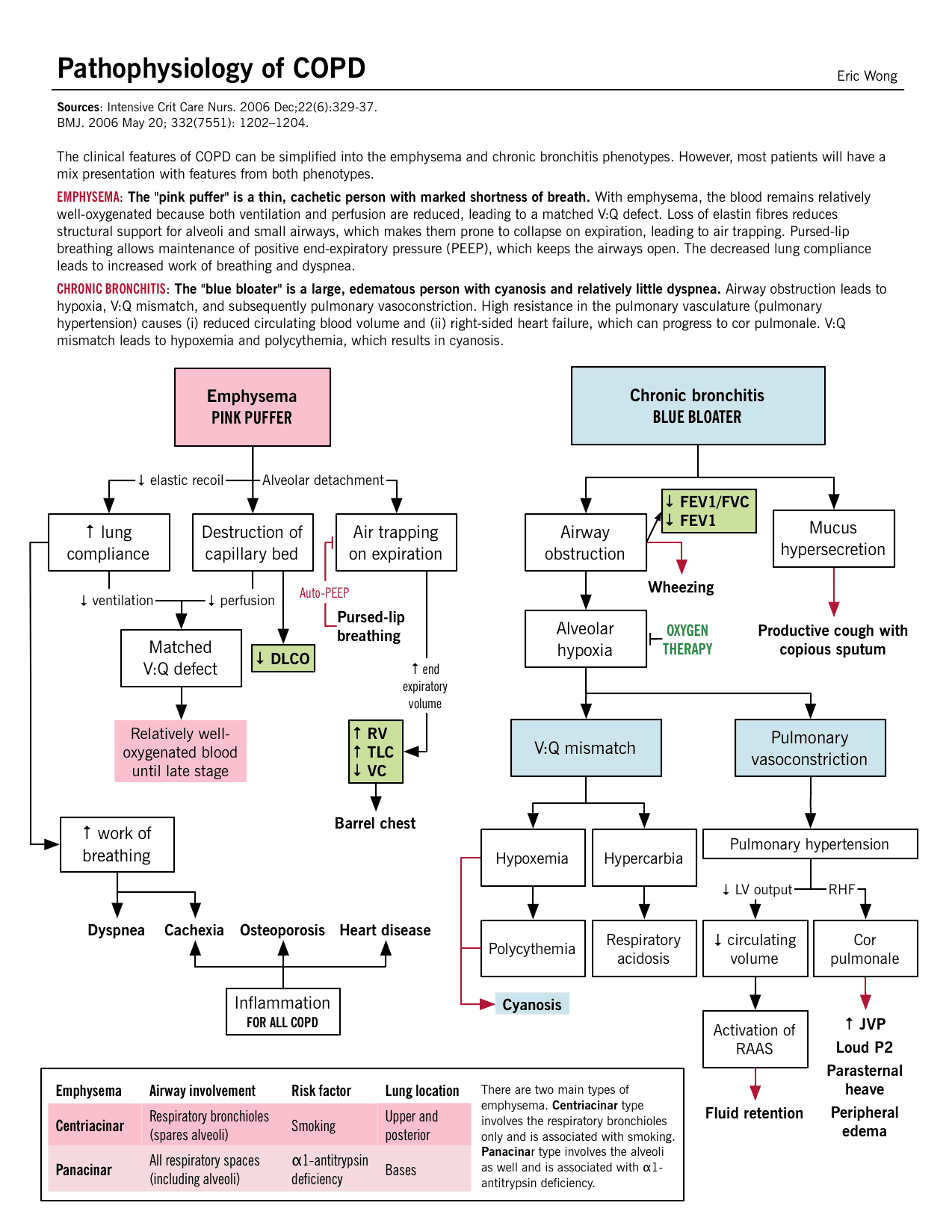
Pathophysiology of COPD
Knowing the pathophysiology of COPD allowed the nurse to recognise and understand the physical symptoms and provide effective care (Mitchell, 2015). Continued exposure to tobacco smoke is the likely cause of the damage to Ms Parker’s small airways, causing her cough and increased sputum production. She could also have chronic inflammation, resulting in airway smooth-muscle contraction, sluggish ciliary movement, hypertrophy and hyperplasia of mucus-secreting goblet cells, as well as release of inflammatory mediators (Mitchell, 2015).
Ms Parker may also have emphysema, which leads to damaged parenchyma (alveoli and structures involved in gas exchange) and loss of alveolar attachments (elastic connective fibres). This causes gas trapping, dynamic hyperinflation, decreased expiratory flow rates and airway collapse, particularly during expiration (Kaufman, 2013). Ms Parker also displayed pursed-lip breathing; this is a technique used to lengthen the expiratory time and improve gaseous exchange, and is a sign of dynamic hyperinflation (Douglas et al, 2013).
In a healthy lung, the destruction and repair of alveolar tissue depends on proteases and antiproteases, mainly released by neutrophils and macrophages. Inhaling cigarette smoke disrupts the usually delicately balanced activity of these enzymes, resulting in the parenchymal damage and small airways (with a lumen of <2mm in diameter) airways disease that is characteristic of emphysema. The severity of parenchymal damage or small airways disease varies, with no pattern related to disease progression (Global Initiative for Chronic Obstructive Lung Disease, 2018).
Ms Parker also had a wheeze, heard through a stethoscope as a continuous whistling sound, which arises from turbulent airflow through constricted airway smooth muscle, a process noted by Mitchell (2015). The wheeze, her 29 pack-year score, exertional breathlessness, cough, sputum production and tiredness, and the findings from her physical examination, were consistent with a diagnosis of COPD (GOLD, 2018; NICE, 2018).
Spirometry is a tool used to identify airflow obstruction but does not identify the cause. Commonly measured parameters are:
- Forced expiratory volume – the volume of air that can be exhaled – in one second (FEV1), starting from a maximal inspiration (in litres);
- Forced vital capacity (FVC) – the total volume of air that can be forcibly exhaled – at timed intervals, starting from a maximal inspiration (in litres).
Calculating the FEV1 as a percentage of the FVC gives the forced expiratory ratio (FEV1/FVC). This provides an index of airflow obstruction; the lower the ratio, the greater the degree of obstruction. In the absence of respiratory disease, FEV1 should be ≥70% of FVC. An FEV1/FVC of <70% is commonly used to denote airflow obstruction (Moore, 2012).
As they are time dependent, FEV1 and FEV1/FVC are reduced in diseases that cause airways to narrow and expiration to slow. FVC, however, is not time dependent: with enough expiratory time, a person can usually exhale to their full FVC. Lung function parameters vary depending on age, height, gender and ethnicity, so the degree of FEV1 and FVC impairment is calculated by comparing a person’s recorded values with predicted values. A recorded value of >80% of the predicted value has been considered ‘normal’ for spirometry parameters but the lower limit of normal – equal to the fifth percentile of a healthy, non-smoking population – based on more robust statistical models is increasingly being used (Cooper et al, 2017).
A reversibility test involves performing spirometry before and after administering a short-acting beta-agonist (SABA) such as salbutamol; the test is used to distinguish between reversible and fixed airflow obstruction. For symptomatic asthma, airflow obstruction due to airway smooth-muscle contraction is reversible: administering a SABA results in smooth-muscle relaxation and improved airflow (Lumb, 2016). However, COPD is associated with fixed airflow obstruction, resulting from neutrophil-driven inflammatory changes, excess mucus secretion and disrupted alveolar attachments, as opposed to airway smooth-muscle contraction.
Administering a SABA for COPD does not usually produce bronchodilation to the extent seen in someone with asthma: a person with asthma may demonstrate significant improvement in FEV1 (of >400ml) after having a SABA, but this may not change in someone with COPD (NICE, 2018). However, a negative response does not rule out therapeutic benefit from long-term SABA use (Marín et al, 2014).
NICE (2018) and GOLD (2018) guidelines advocate performing spirometry after administering a bronchodilator to diagnose COPD. Both suggest a FEV1/FVC of <70% in a person with respiratory symptoms supports a diagnosis of COPD, and both grade the severity of the condition using the predicted FEV1. Ms Parker’s spirometry results showed an FEV1/FVC of 56% and a predicted FEV1 of 57%, with no significant improvement in these values with a reversibility test.
GOLD (2018) guidance is widely accepted and used internationally. However, it was developed by medical practitioners with a medicalised approach, so there is potential for a bias towards pharmacological management of COPD. NICE (2018) guidance may be more useful for practice nurses, as it was developed by a multidisciplinary team using evidence from systematic reviews or meta-analyses of randomised controlled trials, providing a holistic approach. NICE guidance may be outdated on publication, but regular reviews are performed and published online.
NHS England (2016) holds a national register of all health professionals certified in spirometry. It was set up to raise spirometry standards across the country.
Assessment and management
The goals of assessing and managing Ms Parker’s COPD are to:
- Review and determine the level of airflow obstruction;
- Assess the disease’s impact on her life;
- Risk assess future disease progression and exacerbations;
- Recommend pharmacological and therapeutic management.
GOLD’s (2018) ABCD assessment tool (Fig 1) grades COPD severity using spirometry results, number of exacerbations, CAT score and mMRC score, and can be used to support evidence-based pharmacological management of COPD.

When Ms Parker was diagnosed, her predicted FEV1 of 57% categorised her as GOLD grade 2, and her mMRC score, CAT score and exacerbation history placed her in group D. The mMRC scale only measures breathlessness, but the CAT also assesses the impact COPD has on her life, meaning consecutive CAT scores can be compared, providing valuable information for follow-up and management (Zhao, et al, 2014).
After assessing the level of disease burden, Ms Parker was then provided with education for self-management and lifestyle interventions.
Lifestyle interventions
Smoking cessation.
Cessation of smoking alongside support and pharmacotherapy is the second-most cost-effective intervention for COPD, when compared with most other pharmacological interventions (BTS and PCRS UK, 2012). Smoking cessation:
- Slows the progression of COPD;
- Improves lung function;
- Improves survival rates;
- Reduces the risk of lung cancer;
- Reduces the risk of coronary heart disease risk (Qureshi et al, 2014).
Ms Parker accepted a referral to an All Wales Smoking Cessation Service adviser based at her GP surgery. The adviser used the internationally accepted ‘five As’ approach:
- Ask – record the number of cigarettes the individual smokes per day or week, and the year they started smoking;
- Advise – urge them to quit. Advice should be clear and personalised;
- Assess – determine their willingness and confidence to attempt to quit. Note the state of change;
- Assist – help them to quit. Provide behavioural support and recommend or prescribe pharmacological aids. If they are not ready to quit, promote motivation for a future attempt;
- Arrange – book a follow-up appointment within one week or, if appropriate, refer them to a specialist cessation service for intensive support. Document the intervention.
NICE (2013) guidance recommends that this be used at every opportunity. Stead et al (2016) suggested that a combination of counselling and pharmacotherapy have proven to be the most effective strategy.
Pulmonary rehabilitation
Ms Parker’s positive response to smoking cessation provided an ideal opportunity to offer her pulmonary rehabilitation (PR) – as indicated by Johnson et al (2014), changing one behaviour significantly increases a person’s chance of changing another.
PR – a supervised programme including exercise training, health education and breathing techniques – is an evidence-based, comprehensive, multidisciplinary intervention that:
- Improves exercise tolerance;
- Reduces dyspnoea;
- Promotes weight loss (Bolton et al, 2013).
These improvements often lead to an improved quality of life (Sciriha et al, 2015).
Most relevant for Ms Parker, PR has been shown to reduce anxiety and depression, which are linked to an increased risk of exacerbations and poorer health status (Miller and Davenport, 2015). People most at risk of future exacerbations are those who already experience them (Agusti et al, 2010), as in Ms Parker’s case. Patients who have frequent exacerbations have a lower quality of life, quicker progression of disease, reduced mobility and more-rapid decline in lung function than those who do not (Donaldson et al, 2002).
“COPD is a major public-health challenge; nurses can be pivotal in early identification, assessment and management”
Pharmacological interventions
Ms Parker has been prescribed inhaled salbutamol as required; this is a SABA that mediates the increase of cyclic adenosine monophosphate in airway smooth-muscle cells, leading to muscle relaxation and bronchodilation. SABAs facilitate lung emptying by dilatating the small airways, reversing dynamic hyperinflation of the lungs (Thomas et al, 2013). Ms Parker also uses a long-acting muscarinic antagonist (LAMA) inhaler, which works by blocking the bronchoconstrictor effects of acetylcholine on M3 muscarinic receptors in airway smooth muscle; release of acetylcholine by the parasympathetic nerves in the airways results in increased airway tone with reduced diameter.
At a routine review, Ms Parker admitted to only using the SABA and LAMA inhalers, despite also being prescribed a combined inhaled corticosteroid and long-acting beta 2 -agonist (ICS/LABA) inhaler. She was unaware that ICS/LABA inhalers are preferred over SABA inhalers, as they:
- Last for 12 hours;
- Improve the symptoms of breathlessness;
- Increase exercise tolerance;
- Can reduce the frequency of exacerbations (Agusti et al, 2010).
However, moderate-quality evidence shows that ICS/LABA combinations, particularly fluticasone, cause an increased risk of pneumonia (Suissa et al, 2013; Nannini et al, 2007). Inhaler choice should, therefore, be individualised, based on symptoms, delivery technique, patient education and compliance.
It is essential to teach and assess inhaler technique at every review (NICE, 2011). Ms Parker uses both a metered-dose inhaler and a dry-powder inhaler; an in-check device is used to assess her inspiratory effort, as different inhaler types require different inhalation speeds. Braido et al (2016) estimated that 50% of patients have poor inhaler technique, which may be due to health professionals lacking the confidence and capability to teach and assess their use.
Patients may also not have the dexterity, capacity to learn or vision required to use the inhaler. Online resources are available from, for example, RightBreathe (rightbreathe.com), British Lung Foundation (blf.org.uk). Ms Parker’s adherence could be improved through once-daily inhalers, as indicated by results from a study by Lipson et al (2017). Any change in her inhaler would be monitored as per local policy.
Vaccinations
Ms Parker keeps up to date with her seasonal influenza and pneumococcus vaccinations. This is in line with the low-cost, highest-benefit strategy identified by the British Thoracic Society and Primary Care Respiratory Society UK’s (2012) study, which was conducted to inform interventions for patients with COPD and their relative quality-adjusted life years. Influenza vaccinations have been shown to decrease the risk of lower respiratory tract infections and concurrent COPD exacerbations (Walters et al, 2017; Department of Health, 2011; Poole et al, 2006).
Self-management
Ms Parker was given a self-management plan that included:
- Information on how to monitor her symptoms;
- A rescue pack of antibiotics, steroids and salbutamol;
- A traffic-light system demonstrating when, and how, to commence treatment or seek medical help.
Self-management plans and rescue packs have been shown to reduce symptoms of an exacerbation (Baxter et al, 2016), allowing patients to be cared for in the community rather than in a hospital setting and increasing patient satisfaction (Fletcher and Dahl, 2013).
Improving Ms Parker’s adherence to once-daily inhalers and supporting her to self-manage and make the necessary lifestyle changes, should improve her symptoms and result in fewer exacerbations.
The earlier a diagnosis of COPD is made, the greater the chances of reducing lung damage through interventions such as smoking cessation, lifestyle modifications and treatment, if required (Price et al, 2011).
- Chronic obstructive pulmonary disease is a progressive respiratory condition, projected to become the third leading cause of death globally
- Diagnosis involves taking a patient history and performing spirometry testing
- Spirometry identifies airflow obstruction by measuring the volume of air that can be exhaled
- Chronic obstructive pulmonary disease is managed with lifestyle and pharmacological interventions, as well as self-management
Related files
200506 diagnosis and management of copd – a case study.
- Add to Bookmarks
Related articles

Nurse-led cognitive behavioural therapy for respiratory patients
Anxiety and depression are common comorbidities of chronic obstructive pulmonary disease. This…

Issues of home-based non-invasive ventilation
Non-invasive ventilation is increasingly used to manage patients with COPD at home,…

Improving outcomes with online COPD self-care
An innovative approach to the self-management of chronic obstructive pulmonary disease is…

An audit of care provided to patients with COPD
Nationwide audit of COPD care reveals many aspects of provision have improved,…
Have your say
Sign in or Register a new account to join the discussion.
Chronic Obstructive Pulmonary Disease (COPD)
Learn about the nursing care management of patients with chronic obstructive pulmonary disease in this study guide .
Table of Contents
- What is Chronic Obstructive Pulmonary Disease?
Chronic Bronchitis
Pathophysiology, epidemiology, clinical manifestations, complications, assessment and diagnostic findings, pharmacologic therapy, management of exacerbations, surgical management, nursing assessment, planning & goals, nursing priorities, nursing interventions, discharge and home care guidelines, documentation guidelines, what is chronic obstructive pulmonary disease.
Nurses care for patients with COPD across the spectrum of care, from outpatient to home care to emergency department, critical care, and hospice settings.
- Chronic Obstructive Pulmonary Disease (COPD) is a condition of chronic dyspnea with expiratory airflow limitation that does not significantly fluctuate.
- Chronic Obstructive Pulmonary Disease has been defined by The Global Initiative for Chronic Obstructive Lung Disease as “a preventable and treatable disease with some significant extrapulmonary effects that may contribute to the severity in individual patients.”
- This updated definition is a broad description of COPD and its signs and symptoms.
Classification
There are two classifications of COPD: chronic bronchitis and emphysema. These two types of COPD can be sometimes confusing because there are patients who have overlapping signs and symptoms of these two distinct disease processes.
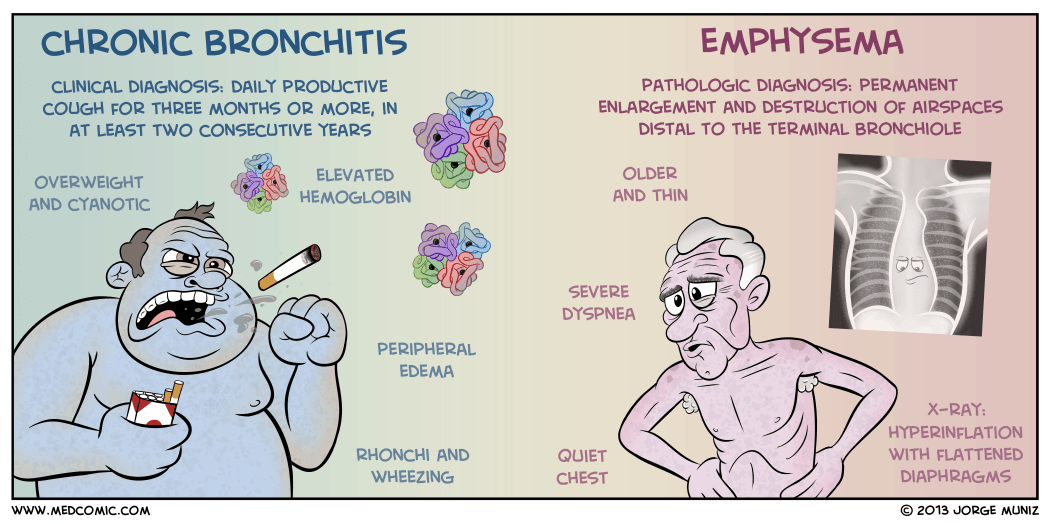
- Chronic bronchitis is a disease of the airways and is defined as the presence of cough and sputum production for at least 3 months in each of 2 consecutive years .
- Chronic bronchitis is also termed as “blue bloaters” .
- Pollutants or allergens irritate the airways and leads to the production of sputum by the mucus-secreting glands and goblet cells.
- A wide range of viral, bacterial, and mycoplasmal infections can produce acute episodes of bronchitis.
- Pulmonary Emphysema is a pathologic term that describes an abnormal distention of airspaces beyond the terminal bronchioles and destruction of the walls of the alveoli.
- People with emphysema are also called “pink puffers”.
- There is impaired carbon dioxide and oxygen exchange, and the exchange results from the destruction of the walls of overdistended alveoli.
- In panlobular , there is destruction of the respiratory bronchiole, alveolar duct, and alveolus.
- All spaces in the lobule are enlarged.
- In centrilobular , pathologic changes occur mainly in the center of the secondary lobule.
In COPD, the airflow limitation is both progressive and associated with an abnormal inflammatory response of the lungs to noxious gases or particles.
- An inflammatory response occurs throughout the proximal and peripheral airways, lung parenchyma, and pulmonary vasculature.
- Due to the chronic inflammation, changes and narrowing occur in the airways.
- There is an increase in the number of goblet cells and enlarged submucosal glands leading to hypersecretion of mucus.
- Scar formation. This can cause scar formation in the long term and narrowing of the airway lumen.
- Wall destruction . Alveolar wall destruction leads to loss of alveolar attachments and a decrease in elastic recoil.
- The chronic inflammatory process affects the pulmonary vasculature and causes thickening of the vessel lining and hypertrophy of smooth muscle .
Mortality for COPD has been increasing ever since while other diseases have decreasing mortalities.
- COPD is the fourth leading cause of death in the United States.
- COPD also account for the death of 125, 000 Americans every year.
- Mortality from COPD among women has increased, and in 2005, more women than men died of COPD.
- Approximately 12 million Americans live with a diagnosis of COPD.
- An additional 2 million may have COPD but remain undiagnosed.
- The annual cost of COPD is approximately $42.6 billion with overall healthcare expenditures of $26.7 billion.
Causes of COPD includes environmental factors and host factors. These includes:
- Smoking depresses the activity of scavenger cells and affects the respiratory tract’s ciliary cleansing mechanism.
- Occupational exposure. Prolonged and intense exposure to occupational dust and chemicals, indoor air pollution, and outdoor air pollution all contribute to the development of COPD.
- Genetic abnormalities . The well-documented genetic risk factor is a deficiency of alpha1- antitrypsin, an enzyme inhibitor that protects the lung parenchyma from injury .
The natural history of COPD is variable but is a generally progressive disease.
- Chronic cough . Chronic cough is one of the primary symptoms of COPD.
- Sputum production . There is a hyperstimulation of the goblet cells and the mucus-secreting gland leading to overproduction of sputum.
- Dyspnea on exertion . Dyspnea is usually progressive, persistent, and worsens with exercise.
- Dyspnea at rest . As COPD progress, dyspnea at rest may occur.
- Weight loss . Dyspnea interferes with eating and the work of breathing is energy depleting.
- Barrel chest . In patients with emphysema, barrel chest thorax configuration results from a more fixed position of the ribs in the inspiratory position and from loss of elasticity.
Prevention of COPD is never impossible. Discipline and consistency are the keys to achieving freedom from chronic pulmonary diseases.
- Smoking cessation . This is the single most cost-effective intervention to reduce the risk of developing COPD and to stop its progression.
- Healthcare providers should promote cessation by explaining the risks of smoking and personalizing the “at-risk” message to the patient.
There are two major life-threatening complications of COPD: respiratory insufficiency and failure.
- Respiratory failure . The acuity and the onset of respiratory failure depend on baseline pulmonary function, pulse oximetry or arterial blood gas values, comorbid conditions, and the severity of other complications of COPD.
- Respiratory insufficiency . This can be acute or chronic, and may necessitate ventilator support until other acute complications can be treated.
Diagnosis and assessment of COPD must be done carefully since the three main symptoms are common among chronic pulmonary disorders.
- Health history . The nurse should obtain a thorough health history from patients with known or potential COPD.
- Pulmonary function studies . Pulmonary function studies are used to help confirm the diagnosis of COPD, determine disease severity, and monitor disease progression.
- Spirometry . Spirometry is used to evaluate airway obstruction , which is determined by the ratio of FEV1 to forced vital capacity.
- ABG . Arterial blood gas measurement is used to assess baseline oxygenation and gas exchange and is especially important in advanced COPD.
- Chest x-ray . A chest x-ray may be obtained to exclude alternative diagnoses.
- CT scan . Computed tomography chest scan may help in the differential diagnosis.
- Screening for alpha1-antitrypsin deficiency . Screening can be performed for patients younger than 45 years old and for those with a strong family history of COPD.
- Chest x-ray: May reveal hyperinflation of lungs, flattened diaphragm , increased retrosternal air space, decreased vascular markings/bullae (emphysema), increased bronchovascular markings (bronchitis), normal findings during periods of remission ( asthma ).
- Pulmonary function tests: Done to determine cause of dyspnea, whether functional abnormality is obstructive or restrictive, to estimate degree of dysfunction and to evaluate effects of therapy, e.g., bronchodilators . Exercise pulmonary function studies may also be done to evaluate activity tolerance in those with known pulmonary impairment/progression of disease.
- The forced expiratory volume over 1 second (FEV 1 ): Reduced FEV 1 not only is the standard way of assessing the clinical course and degree of reversibility in response to therapy, but also is an important predictor of prognosis.
- Total lung capacity (TLC), functional residual capacity (FRC), and residual volume (RV): May be increased, indicating air-trapping. In obstructive lung disease, the RV will make up the greater portion of the TLC.
- Arterial blood gases ( ABGs ): Determines degree and severity of disease process, e.g., most often Pao 2 is decreased, and Paco 2 is normal or increased in chronic bronchitis and emphysema , but is often decreased in asthma ; pH normal or acidotic, mild respiratory alkalosis secondary to hyperventilation (moderate emphysema or asthma ).
- D L CO test: Assesses diffusion in lungs. Carbon monoxide is used to measure gas diffusion across the alveocapillary membrane. Because carbon monoxide combines with hemoglobin 200 times more easily than oxygen, it easily affects the alveoli and small airways where gas exchange occurs. Emphysema is the only obstructive disease that causes diffusion dysfunction.
- Bronchogram: Can show cylindrical dilation of bronchi on inspiration; bronchial collapse on forced expiration ( emphysema ); enlarged mucous ducts (bronchitis).
- Lung scan: Perfusion/ ventilation studies may be done to differentiate between the various pulmonary diseases. COPD is characterized by a mismatch of perfusion and ventilation (i.e., areas of abnormal ventilation in area of perfusion defect).
- Complete blood count (CBC) and differential: Increased hemoglobin (advanced emphysema ), increased eosinophils (asthma).
- Blood chemistry: alpha 1 -antitrypsin is measured to verify deficiency and diagnosis of primary emphysema .
- Sputum culture: Determines presence of infection , identifies pathogen.
- Cytologic examination: Rules out underlying malignancy or allergic disorder.
- Electrocardiogram ( ECG ): Right axis deviation, peaked P waves (severe asthma); atrial dysrhythmias (bronchitis), tall, peaked P waves in leads II, III, AVF (bronchitis, emphysema ); vertical QRS axis (emphysema).
- Exercise ECG , stress test: Helps in assessing degree of pulmonary dysfunction, evaluating effectiveness of bronchodilator therapy, planning /evaluating exercise program.
Medical Management
Healthcare providers perform medical management by considering the assessment data first and matching the appropriate intervention to the existing manifestation.
- Bronchodilators . Bronchodilators relieve bronchospasm by altering the smooth muscle tone and reduce airway obstruction by allowing increased oxygen distribution throughout the lungs and improving alveolar ventilation.
- Corticosteroids . A short trial course of oral corticosteroids may be prescribed for patients to determine whether pulmonary function improves and symptoms decrease.
- Other medications . Other pharmacologic treatments that may be used in COPD include alpha1-antitrypsin augmentation therapy, antibiotic agents, mucolytic agents, antitussive agents, vasodilators , and narcotics .
- Optimization of bronchodilator medications is first-line therapy and involves identifying the best medications or combinations of medications taken on a regular schedule for a specific patient.
- Hospitalization . Indications for hospitalization for acute exacerbation of COPD include severe dyspnea that does not respond to initial therapy, confusion or lethargy , respiratory muscle fatigue , paradoxical chest wall movement , and peripheral edema .
- Oxygen therapy . Upon arrival of the patient in the emergency room, supplemental oxygen therapy is administered and rapid assessment is performed to determine if the exacerbation is life-threatening.
- Antibiotics . Antibiotics have been shown to be of some benefit to patients with increased dyspnea, increased sputum production, and increased sputum purulence.
Patients with COPD also have options for surgery to improve their condition.
- Bullectomy . Bullectomy is a surgical option for select patients with bullous emphysema and can help reduce dyspnea and improve lung function.
- Lung Volume Reduction Surgery . Lung volume reduction surgery is a palliative surgery in patients with homogenous disease or disease that is focused in one area and not widespread throughout the lungs.
- Lung Transplantation . Lung transplantation is a viable option for definitive surgical treatment of end-stage emphysema.
Nursing Management
Management of patients with COPD should be incorporated with teaching and improving the respiratory status of the patient. Learn about the nursing care management of patients with Chronic Obstructive Pulmonary Disease using the nursing process in this guide.
SEE ALSO: 8 Chronic Obstructive Pulmonary Disease (COPD) Nursing Care Plans for a comprehensive nursing care plan and management guide
Assessment of the respiratory system should be done rapidly yet accurately.
- Assess patient’s exposure to risk factors.
- Assess the patient’s past and present medical history .
- Assess the signs and symptoms of COPD and their severity.
- Assess the patient’s knowledge of the disease.
- Assess the patient’s vital signs.
- Assess breath sounds and pattern.
Diagnosis of COPD would mainly depend on the assessment data gathered by the healthcare team members.
- Impaired gas exchange due to chronic inhalation of toxins.
- Ineffective airway clearance related to bronchoconstriction, increased mucus production, ineffective cough, and other complications.
- Ineffective breathing pattern related to shortness of breath , mucus, bronchoconstriction, and airway irritants.
- Self-care deficit related to fatigue .
- Activity intolerance related to hypoxemia and ineffective breathing patterns.
Goals to achieve in patients with COPD include:
- Improvement in gas exchange.
- Achievement of airway clearance.
- Improvement in breathing pattern.
- Independence in self-care activities.
- Improvement in activity intolerance .
- Ventilation/ oxygenation adequate to meet self-care needs.
- Nutritional intake meeting caloric needs.
- Infection treated/prevented.
- Disease process/prognosis and therapeutic regimen understood.
- Plan in place to meet needs after discharge.
- Maintain airway patency .
- Assist with measures to facilitate gas exchange.
- Enhance nutritional intake.
- Prevent complications, slow progression of condition.
- Provide information about disease process/prognosis and treatment regimen.
Patient and family teaching is an important nursing intervention to enhance self-management in patients with any chronic pulmonary disorder.
To achieve airway clearance:
- The nurse must appropriately administer bronchodilators and corticosteroids and become alert for potential side effects.
- Direct or controlled coughing . The nurse instructs the patient in direct or controlled coughing, which is more effective and reduces fatigue associated with undirected forceful coughing.
To improve breathing pattern:
- Inspiratory muscle training . This may help improve the breathing pattern.
- Diaphragmatic breathing . Diaphragmatic breathing reduces respiratory rate, increases alveolar ventilation, and sometimes helps expel as much air as possible during expiration.
- Pursed lip breathing . Pursed lip breathing helps slow expiration, prevents collapse of small airways, and control the rate and depth of respiration.
To improve activity intolerance :
- Manage daily activities . Daily activities must be paced throughout the day and support devices can be also used to decrease energy expenditure.
- Exercise training . Exercise training can help strengthen muscles of the upper and lower extremities and improve exercise tolerance and endurance.
- Walking aids . Use of walking aids may be recommended to improve activity levels and ambulation .
To monitor and manage potential complications:
- Monitor cognitive changes . The nurse should monitor for cognitive changes such as personality and behavior changes and memory impairment .
- Monitor pulse oximetry values . Pulse oximetry values are used to assess the patient’s need for oxygen and administer supplemental oxygen as prescribed.
- Prevent infection . The nurse should encourage the patient to be immunized against influenza and S. pneumonia because the patient is prone to respiratory infection.
During evaluation , the effectiveness of the care plan would be measured if goals were achieved in the end and the patient:
- Identifies the hazards of cigarette smoking.
- Identifies resources for smoking cessation.
- Enrolls in smoking cessation program.
- Minimizes or eliminates exposures.
- Verbalizes the need for fluids.
- Is free of infection.
- Practices breathing techniques.
- Performs activities with less shortness of breath .
It is important for the nurse to assess the knowledge of patient and family members about self-care and the therapeutic regimen .
- Setting goals. If the COPD is mild, the objectives of the treatment are to increase exercise tolerance and prevent further loss of pulmonary function, while if COPD is severe, these objectives are to preserve current pulmonary function and relieve symptoms as much as possible.
- Temperature control. The nurse should instruct the patient to avoid extremes of heat and cold because heat increases the temperature and thereby raising oxygen requirements and high altitudes increase hypoxemia .
- Activity moderation. The patient should adapt a lifestyle of moderate activity and should avoid emotional disturbances and stressful situations that might trigger a coughing episode.
- Breathing retraining. The home care nurse must provide the education and breathing retraining necessary to optimize the patient’s functional status.
Documentation is an essential part of the patient’s chart because the interventions and medications given and done are reflected on this part.
- Document assessment findings including respiratory rate, character of breath sounds; frequency, amount and appearance of secretions laboratory findings and mentation level.
- Document conditions that interfere with oxygen supply.
- Document plan of care and specific interventions.
- Document liters of supplemental oxygen.
- Document client’s responses to treatment, teaching, and actions performed.
- Document teaching plan.
- Document modifications to plan of care.
- Document attainment or progress towards goals.
See also: Respiratory System NCLEX Practice Questions and Reviewer (220 Questions)
6 thoughts on “Chronic Obstructive Pulmonary Disease (COPD)”
This article is very helpful with nursing plans with first semester nursing students. Thank you.
VERY HELPFUL WITH NURSING CARE PLAN. THANK YOU
Full care plan send sir
VERY INFORMATIVE…
Hey Suzanne, Thanks a lot! 😊 Glad you found it helpful.
Very helpful for work use and outside of work use
Leave a Comment Cancel reply

COPD Case Study: Patient Diagnosis and Treatment (2024)
by John Landry, BS, RRT | Updated: May 16, 2024
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease that affects millions of people around the world. It is primarily caused by smoking and is characterized by a persistent obstruction of airflow that worsens over time.
COPD can lead to a range of symptoms, including coughing, wheezing, shortness of breath, and chest tightness, which can significantly impact a person’s quality of life.
This case study will review the diagnosis and treatment of an adult patient who presented with signs and symptoms of this condition.
25+ RRT Cheat Sheets and Quizzes
Get access to 25+ premium quizzes, mini-courses, and downloadable cheat sheets for FREE.
COPD Clinical Scenario
A 56-year-old male patient is in the ER with increased work of breathing. He felt mildly short of breath after waking this morning but became extremely dyspneic after climbing a few flights of stairs. He is even too short of breath to finish full sentences. His wife is present in the room and revealed that the patient has a history of liver failure, is allergic to penicillin, and has a 15-pack-year smoking history. She also stated that he builds cabinets for a living and is constantly required to work around a lot of fine dust and debris.

Physical Findings
On physical examination, the patient showed the following signs and symptoms:
- His pupils are equal and reactive to light.
- He is alert and oriented.
- He is breathing through pursed lips.
- His trachea is positioned in the midline, and no jugular venous distention is present.
Vital Signs
- Heart rate: 92 beats/min
- Respiratory rate: 22 breaths/min
Chest Assessment
- He has a larger-than-normal anterior-posterior chest diameter.
- He demonstrates bilateral chest expansion.
- He demonstrates a prolonged expiratory phase and diminished breath sounds during auscultation.
- He is showing signs of subcostal retractions.
- Chest palpation reveals no tactile fremitus.
- Chest percussion reveals increased resonance.
- His abdomen is soft and tender.
- No distention is present.
Extremities
- His capillary refill time is two seconds.
- Digital clubbing is present in his fingertips.
- There are no signs of pedal edema.
- His skin appears to have a yellow tint.
Lab and Radiology Results
- ABG results: pH 7.35 mmHg, PaCO2 59 mmHg, HCO3 30 mEq/L, and PaO2 64 mmHg.
- Chest x-ray: Flat diaphragm, increased retrosternal space, dark lung fields, slight hypertrophy of the right ventricle, and a narrow heart.
- Blood work: RBC 6.5 mill/m3, Hb 19 g/100 mL, and Hct 57%.
Based on the information given, the patient likely has chronic obstructive pulmonary disease (COPD) .
The key findings that point to this diagnosis include:
- Barrel chest
- A long expiratory time
- Diminished breath sounds
- Use of accessory muscles while breathing
- Digital clubbing
- Pursed lip breathing
- History of smoking
- Exposure to dust from work
What Findings are Relevant to the Patient’s COPD Diagnosis?
The patient’s chest x-ray showed classic signs of chronic COPD, which include hyperexpansion, dark lung fields, and a narrow heart.
This patient does not have a history of cor pulmonale ; however, the findings revealed hypertrophy of the right ventricle. This is something that should be further investigated as right-sided heart failure is common in patients with COPD.
The lab values that suggest the patient has COPD include increased RBC, Hct, and Hb levels, which are signs of chronic hypoxemia.
Furthermore, the patient’s ABG results indicate COPD is present because the interpretation reveals compensated respiratory acidosis with mild hypoxemia. Compensated blood gases indicate an issue that has been present for an extended period of time.
What Tests Could Further Support This Diagnosis?
A series of pulmonary function tests (PFT) would be useful for assessing the patient’s lung volumes and capacities. This would help confirm the diagnosis of COPD and inform you of the severity.
Note: COPD patients typically have an FEV1/FVC ratio of < 70%, with an FEV1 that is < 80%.
The initial treatment for this patient should involve the administration of low-flow oxygen to treat or prevent hypoxemia .
It’s acceptable to start with a nasal cannula at 1-2 L/min. However, it’s often recommended to use an air-entrainment mask on COPD patients in order to provide an exact FiO2.
Either way, you should start with the lowest possible FiO2 that can maintain adequate oxygenation and titrate based on the patient’s response.
Example: Let’s say you start the patient with an FiO2 of 28% via air-entrainment mask but increase it to 32% due to no improvement. The SpO2 originally was 84% but now has decreased to 80%, and his retractions are worsening. This patient is sitting in the tripod position and continues to demonstrate pursed-lip breathing. Another blood gas was collected, and the results show a PaCO2 of 65 mmHg and a PaO2 of 59 mmHg.
What Do You Recommend?
The patient has an increased work of breathing, and their condition is clearly getting worse. The latest ABG results confirmed this with an increased PaCO2 and a PaO2 that is decreasing.
This indicates that the patient needs further assistance with both ventilation and oxygenation .
Note: In general, mechanical ventilation should be avoided in patients with COPD (if possible) because they are often difficult to wean from the machine.
Therefore, at this time, the most appropriate treatment method is noninvasive ventilation (e.g., BiPAP).
Initial BiPAP Settings
In general, the most commonly recommended initial BiPAP settings for an adult patient include this following:
- IPAP: 8–12 cmH2O
- EPAP: 5–8 cmH2O
- Rate: 10–12 breaths/min
- FiO2: Whatever they were previously on
For example, let’s say you initiate BiPAP with an IPAP of 10 cmH20, an EPAP of 5 cmH2O, a rate of 12, and an FiO2 of 32% (since that is what he was previously getting).
After 30 minutes on the machine, the physician requested another ABG to be drawn, which revealed acute respiratory acidosis with mild hypoxemia.
What Adjustments to BiPAP Settings Would You Recommend?
The latest ABG results indicate that two parameters must be corrected:
- Increased PaCO2
- Decreased PaO2
You can address the PaO2 by increasing either the FiO2 or EPAP setting. EPAP functions as PEEP, which is effective in increasing oxygenation.
The PaCO2 can be lowered by increasing the IPAP setting. By doing so, it helps to increase the patient’s tidal volume, which increased their expired CO2.
Note: In general, when making adjustments to a patient’s BiPAP settings, it’s acceptable to increase the pressure in increments of 2 cmH2O and the FiO2 setting in 5% increments.
Oxygenation
To improve the patient’s oxygenation , you can increase the EPAP setting to 7 cmH2O. This would decrease the pressure support by 2 cmH2O because it’s essentially the difference between the IPAP and EPAP.
Therefore, if you increase the EPAP, you must also increase the IPAP by the same amount to maintain the same pressure support level.
Ventilation
However, this patient also has an increased PaCO2 , which means that you must increase the IPAP setting to blow off more CO2. Therefore, you can adjust the pressure settings on the machine as follows:
- IPAP: 14 cmH2O
- EPAP: 7 cmH2O
After making these changes and performing an assessment , you can see that the patient’s condition is improving.
Two days later, the patient has been successfully weaned off the BiPAP machine and no longer needs oxygen support. He is now ready to be discharged.
The doctor wants you to recommend home therapy and treatment modalities that could benefit this patient.
What Home Therapy Would You Recommend?
You can recommend home oxygen therapy if the patient’s PaO2 drops below 55 mmHg or their SpO2 drops below 88% more than twice in a three-week period.
Remember: You must use a conservative approach when administering oxygen to a patient with COPD.
Pharmacology
You may also consider the following pharmacological agents:
- Short-acting bronchodilators (e.g., Albuterol)
- Long-acting bronchodilators (e.g., Formoterol)
- Anticholinergic agents (e.g., Ipratropium bromide)
- Inhaled corticosteroids (e.g., Budesonide)
- Methylxanthine agents (e.g., Theophylline)
In addition, education on smoking cessation is also important for patients who smoke. Nicotine replacement therapy may also be indicated.
In some cases, bronchial hygiene therapy should be recommended to help with secretion clearance (e.g., positive expiratory pressure (PEP) therapy).
It’s also important to instruct the patient to stay active, maintain a healthy diet, avoid infections, and get an annual flu vaccine. Lastly, some COPD patients may benefit from cardiopulmonary rehabilitation .
By taking all of these factors into consideration, you can better manage this patient’s COPD and improve their quality of life.
Final Thoughts
There are two key points to remember when treating a patient with COPD. First, you must always be mindful of the amount of oxygen being delivered to keep the FiO2 as low as possible.
Second, you should use noninvasive ventilation, if possible, before performing intubation and conventional mechanical ventilation . Too much oxygen can knock out the patient’s drive to breathe, and once intubated, these patients can be difficult to wean from the ventilator .
Furthermore, once the patient is ready to be discharged, you must ensure that you are sending them home with the proper medications and home treatments to avoid readmission.

Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
- Faarc, Kacmarek Robert PhD Rrt, et al. Egan’s Fundamentals of Respiratory Care. 12th ed., Mosby, 2020.
- Chang, David. Clinical Application of Mechanical Ventilation . 4th ed., Cengage Learning, 2013.
- Rrt, Cairo J. PhD. Pilbeam’s Mechanical Ventilation: Physiological and Clinical Applications. 7th ed., Mosby, 2019.
- Faarc, Gardenhire Douglas EdD Rrt-Nps. Rau’s Respiratory Care Pharmacology. 10th ed., Mosby, 2019.
- Faarc, Heuer Al PhD Mba Rrt Rpft. Wilkins’ Clinical Assessment in Respiratory Care. 8th ed., Mosby, 2017.
- Rrt, Des Terry Jardins MEd, and Burton George Md Facp Fccp Faarc. Clinical Manifestations and Assessment of Respiratory Disease. 8th ed., Mosby, 2019.
Recommended Reading
How to prepare for the clinical simulations exam (cse), faqs about the clinical simulation exam (cse), 7+ mistakes to avoid on the clinical simulation exam (cse), copd exacerbation: chronic obstructive pulmonary disease, epiglottitis scenario: clinical simulation exam (practice problem), guillain barré syndrome case study: clinical simulation scenario, drugs and medications to avoid if you have copd, the pros and cons of the zephyr valve procedure, the 50+ diseases to learn for the clinical sims exam (cse).
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Mr. Jake Dogson is a 62 year old male with a history of chronic obstructive pulmonary disease (COPD), hypertension, and hyperlipidemia. He was a previous smoker for forty years; he quit when he was diagnosed with COPD 10 years ago. His home medications include ipratroprium via nebulizer once a day, albuterol quick-relief inhaler, metoprolol, lisinopril, hydrochlorothiazide, and atorvastatin. He is up to date on his annual pneumococcal and influenza vaccinations, recommended for individuals with COPD (Holmes & Scullion, 2015). Family history for Mr. Dogson includes his father dying of a heart attack at age 72.
Jake Dogson was at home watching the food network learning a recipe to surprise his wife for his anniversary dinner. He had been at work the whole day, repairing arcade machines at the local theme park. His wife was teaching her water aerobics class at the gym. Mr. Dogson prepared the ingredients and began to cook his meal. While cooking, he left the kitchen for a moment and mistakenly left a towel on one of the over burners, which soon caught fire. He attempted to smother the fire with his apron which also caught fire. Smoke soon swarmed around him, forcing him to leave his home, running outside in a panic. A neighbor witnessed the scene and called 911. The fire department arrived at 18:00 to find him lying on the lawn with shallow breathing, wheezing, and a respiratory rate of 33, heart rate 116, blood pressure 140/90, and oxygen saturation at 88%. They transported him to St. Medical Hospital in Tuscaloosa, Alabama.
On arrival to the emergency department, nurses immediately took Mr. Dogson’s vitals (Appendix B). Upon assessment, Mr. Dogson was found to have barrel chest, bilateral wheezes, dyspnea, moderate intercostal retractions, cough with yellow-brown sputum, and hoarseness. Neurologically, Mr. Dogson was alert and oriented to person, place, time, and situation. He had S1S2 heart sounds and he presented with tachycardia and hypertension. Capillary refill was 3 seconds. He had bowel sounds in all four quadrants with a soft, nontender abdomen. The physician orders included oxygen to keep O2 above 90%, continuous pulse oximetry, STAT chest x-ray, basic metabolic panel, ABGs STAT, vitals every 30 minutes, albuterol 2.5 mg inhaled via nebulizer, a continuous EKG due to tachycardia and hypertension, and pulmonary function tests. The x-ray revealed lung hyperinflation and a flattened diaphragm due to his COPD. Arterial blood gases are listed in Appendix B. ECG revealed sinus tachycardia without signs of right ventricular hypertrophy or ischemia. Labs revealed increased hematocrit, BUN of 22, Creatinine 1.21, and elevated PaCO2 and carboxylhemoglobin from smoke inhalation (Demling, 2008). All other laboratory findings were within normal range. Pulmonary function tests revealed an FEV1/PVC ration of 0.55 which is indicative of airway obstruction (Cornforth, 2012). He was diagnosed with acute COPD exacerbation from smoke inhalation due to assessment and lab findings.
He was kept overnight for observation based on the continued symptoms, dyspnea and low oxygen saturation in the ER. The respiratory therapist administered two albuterol treatments in the ED. However, upon 05:00 assessment, Mr. Dogson showed dyspnea, increased wheezes, cyanosis of the lips, agitation, and confusion. His oxygen saturation was 77 and his respiratory rate increased to 36/minute. The nurse immediately began ventilating the patient with a bag valve mask at 15L/min and called a rapid response. The rapid response team intubated Mr. Dogson and transported him to the ICU at 06:30. He had an 18 gauge IV placed in his right upper arm with normal saline running at 75 ml/hour and a Foley catheter inserted.
In the ICU, physician orders included vitals every 30 minutes, ABGs every 4 hours, a chest x-ray to confirm tube placement, a CT scan to evaluate for hypoxic brain injury, a bronchoscopy to visualize the small airways, intake and output record, and a lactate level for to evaluate for lactic acidosis (Medscape 2017). Medication orders included albuterol, ipratroprium bromide, and methylprednisolone for bronchodilation and COPD management; famotidine for prevention of gastric reflux; lovenox for prevention of deep vein thrombosis; and labetalol and enalapril for hypertension (Medscape 2017).
By 14:00 on the first day in the ICU, Mr. Dogson’s vitals stabilized (Appendix A) however his ABGs still showed respiratory acidosis (Appendix B). Nursing care for the day included suctioning and oral care every 2 hours to prevent aspiration, sequential compression device applied to the legs, turning every two hours for skin precautions, and hourly assessment. Upon assessment the first day, Mr. Dogson consistently showed restlessness, bilateral faint wheezes, and diminished lower lobes due to COPD and airway injury (Dewar, et al. 2016).
ABGs following intubation showed improvement the next morning, and Mr. Dogson was no longer in respiratory acidosis. Therefore during rounds the physician decided to wean Mr. Dogson off the ventilator on synchronized intermittent mandatory ventilation (SIMV) and titrate sedation down. Upon spontaneous breathing trial (SBT) Mr. Dogson was found to be protecting his airway, he had an intact cough and gag reflex, he had decreased wheezing on auscultation and overall better lung sounds as he was responding well to the bronchodilators, steroid, and oxygen therapy.
The following day he was transferred to the med-surg unit. The nurse put him on an oxygen trial and was able to maintain an oxygen saturation of 90% on 2L nasal cannula (85% without oxygen therapy). Assessment findings were alert and oriented to person, place, time and situation, heart sounds S1S2 normal sinus rhythm, capillary refill 3 seconds, lung sounds clear with distant sounds in the lower lobes, and integument warm and dry. Mr. Dogson was discharged the next day with a prescription for home oxygen therapy.
During his stay at the hospital discharge planning, beginning on admission, case management aided Mr. and Mrs. Dogson with housing, support groups, grief counseling, and financial issues. The case manager ordered a home oxygen for Mr. Dogson, and requested an evaluation for and dispensing of a lightweight portable oxygen system and conserving device. He also received education regarding the use of his prescribed medications, encouraged a physical activity regimen, and prevention of future exacerbations of COPD.
Case management assisted in finding temporary housing at Mrs. Dogson’s sisters home after assisting in filing a claim with the Dogson’s homeowner’s insurance company. Case management also assisted in finding a local food bank near Mrs. Dogson’s sisters house to cope with living expenses and set up deliveries to the home once a week. Financial issues were important to consider as Mr. Dogson is a theme park worker and does not make much money and his wife only works part-time.
The case manager also provided Mr. Dogson with contact information for COPD support group one mile away from the home, as well as grief counseling for Mr. and Mrs. Dogson for loss of home, important documents, family photos, and personal belongings.
American Association for Clinical Chemistry. (2017). Lab Tests Online. Retrieved from www.labtestonline.org
Blair, K. A., & Evelo, A. J. (2014). Risk Factors for COPD: What do NPs know?. Journal Of The American Association Of Nurse Practitioners, 26(3), 123-130. doi: 10.1002/2327-6924.12032
Cleveland Clinic. (2017). Nutritional guidelines for people with COPD. Retrieved from http://myclevelandclinic.org/health/articles/nutritional-guidelines-for-people-with-copd
Cornforth, A. (2012). Diagnosis and management of COPD. Nurse Prescribing, 10(2), 65-71.
Demling, R. H. (2008). Smoke Inhalation Lung Injury: An Update. Eplasty , 8, e27.
Hanlon, P. (2017). Asthma/COPD: Diagnosis and Management with Spirometry. RT: The Journal For Respiratory Care Practitioners, 30(1), 22-26
Holmes, S., & Scullion, J. (2015). A changing landscape: diagnosis and management of COPD… Chronic obstructive pulmonary disease. British Journal Of Nursing, 24(8), 432-440. doi: 10.12968/bjon.2015.24.8.432
Marvin Dewar, M.D., J.D., and R. Whit Curry, JR., M.D., University of Florida College of Medicine, Gainesville, Florida. Am Fam Physician. 2006 Feb 15;73(4): 669-676
Medscape (2017). Lactic acidosis. http://emedicine.medscape.com/article/167027-overview
Mitchell, J. (2015). Pathophysiology of COPD: Part 1. Practice Nursing, 26(4), 172-178.
Reddy, R. M., & Guntupalli, K. K. (2007). Review of ventilatory techniques to optimize mechanical ventilation in acute exacerbation of chronic obstructive pulmonary disease. International Journal of Chronic Obstructive Pulmonary Disease, 2(4), 441-452.
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 07 May 2015
Four patients with a history of acute exacerbations of COPD: implementing the CHEST/Canadian Thoracic Society guidelines for preventing exacerbations
- Ioanna Tsiligianni 1 , 2 ,
- Donna Goodridge 3 ,
- Darcy Marciniuk 4 ,
- Sally Hull 5 &
- Jean Bourbeau 6
npj Primary Care Respiratory Medicine volume 25 , Article number: 15023 ( 2015 ) Cite this article
60k Accesses
12 Altmetric
Metrics details
- Respiratory tract diseases
The American College of Chest Physicians and Canadian Thoracic Society have jointly produced evidence-based guidelines for the prevention of exacerbations in chronic obstructive pulmonary disease (COPD). This educational article gives four perspectives on how these guidelines apply to the practical management of people with COPD. A current smoker with frequent exacerbations will benefit from support to quit, and from optimisation of his inhaled treatment. For a man with very severe COPD and multiple co-morbidities living in a remote community, tele-health care may enable provision of multidisciplinary care. A woman who is admitted for the third time in a year needs a structured assessment of her care with a view to stepping up pharmacological and non-pharmacological treatment as required. The overlap between asthma and COPD challenges both diagnostic and management strategies for a lady smoker with a history of asthma since childhood. Common threads in all these cases are the importance of advising on smoking cessation, offering (and encouraging people to attend) pulmonary rehabilitation, and the importance of self-management, including an action plan supported by multidisciplinary teams.
Similar content being viewed by others

Diagnostic spirometry in COPD is increasing, a comparison of two Swedish cohorts
Phenotype and management of chronic obstructive pulmonary disease patients in general population in China: a nationally cross-sectional study

Cardiovascular predictors of mortality and exacerbations in patients with COPD
Case study 1: a 63-year-old man with moderate/severe copd and a chest infection.
A 63-year-old self-employed plumber makes a same-day appointment for another ‘chest infection’. He caught an upper respiratory tract infection from his grandchildren 10 days ago, and he now has a productive cough with green sputum, and his breathlessness and fatigue has forced him to take time off work.
He has visited his general practitioner with similar symptoms two or three times every year in the last decade. A diagnosis of COPD was confirmed 6 years ago, and he was started on a short-acting β 2 -agonist. This helped with his day-to-day symptoms, although recently the symptoms of breathlessness have been interfering with his work and he has to pace himself to get through the day. Recovering from exacerbations takes longer than it used to—it is often 2 weeks before he is able to get back to work—and he feels bad about letting down customers. He cannot afford to retire, but is thinking about reducing his workload.
He last attended a COPD review 6 months ago when his FEV 1 was 52% predicted. He was advised to stop smoking and given a prescription for varenicline, but he relapsed after a few days and did not return for the follow-up appointment. He attends each year for his ‘flu vaccination’. His only other medication is an ACE inhibitor for hypertension.
Managing the presenting problem. Is it a COPD exacerbation?
A COPD exacerbation is defined as ‘an acute event characterised by a worsening of the patient’s respiratory symptoms that is beyond normal day-to-day variation and leads to change in medications’. 1 , 2 The worsening symptoms are usually increased dyspnoea, increased sputum volume and increased sputum purulence. 1 , 2 All these symptoms are present in our patient who experiences an exacerbation triggered by a viral upper respiratory tract infection—the most common cause of COPD exacerbations. Apart from the management of the acute exacerbation that could include antibiotics, oral steroids and increased use of short-acting bronchodilators, special attention should be given to his on-going treatment to prevent future exacerbations. 2 Short-term use of systemic corticosteroids and a course of antibiotics can shorten recovery time, improve lung function (forced expiratory volume in one second (FEV 1 )) and arterial hypoxaemia and reduce the risk of early relapse, treatment failure and length of hospital stay. 1 , 2 Short-acting inhaled β 2 -agonists with or without short-acting anti-muscarinics are usually the preferred bronchodilators for the treatment of an acute exacerbation. 1
Reviewing his routine treatment
One of the concerns about this patient is that his COPD is inadequately treated. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) suggests that COPD management be based on a combined assessment of symptoms, GOLD classification of airflow limitation, and exacerbation rate. 1 The modified Medical Research Council (mMRC) dyspnoea score 3 or the COPD Assessment Tool (CAT) 4 could be used to evaluate the symptoms/health status. History suggests that his breathlessness has begun to interfere with his lifestyle, but this has not been formally asssessed since the diagnosis 6 years ago. Therefore, one would like to be certain that these elements are taken into consideration in future management by involving other members of the health care team. The fact that he had two to three exacerbations per year puts the patient into GOLD category C–D (see Figure 1 ) despite the moderate airflow limitation. 1 , 5 Our patient is only being treated with short-acting bronchodilators; however, this is only appropriate for patients who belong to category A. Treatment options for patients in category C or D should include long-acting muscarinic antagonists (LAMAs) or long-acting β 2 -agonists (LABAs), which will not only improve his symptoms but also help prevent future exacerbations. 2 Used in combination with LABA or LAMA, inhaled corticosteroids also contribute to preventing exacerbations. 2
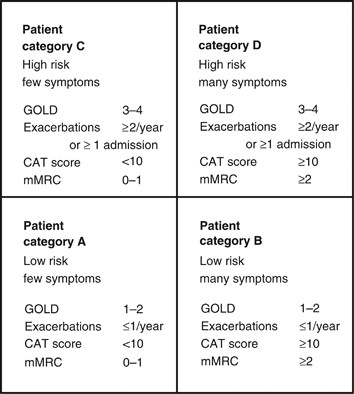
The four categories of COPD based on assessment of symptoms and future risk of exacerbations (adapted by Gruffydd-Jones, 5 from the Global Strategy for Diagnosis, Management and Prevention of COPD). 1 CAT, COPD Assessment Tool; COPD, chronic obstructive pulmonary disease; mMRC, modified Medical Research Council Dyspnoea Scale.
Prevention of future exacerbations
Exacerbations should be prevented as they have a negative impact on the quality of life; they adversely affect symptoms and lung function, increase economic cost, increase mortality and accelerate lung function decline. 1 , 2 Figure 2 summarises the recommendations and suggestions of the joint American College of Chest Physicians and Canadian Thoracic Society (CHEST/CTS) Guidelines for the prevention of exacerbations in COPD. 2 The grades of recommendation from the CHEST/CTS guidelines are explained in Table 1 .

Decision tree for prevention of acute exacerbations of COPD (reproduced with permission from the CHEST/CTS Guidelines for the prevention of exacerbations in COPD). 2 This decision tree for prevention of acute exacerbations of COPD is arranged according to three key clinical questions using the PICO format: non-pharmacologic therapies, inhaled therapies and oral therapies. The wording used is ‘Recommended or Not recommended’ when the evidence was strong (Level 1) or ‘Suggested or Not suggested’ when the evidence was weak (Level 2). CHEST/CTS, American College of Chest Physicians and Canadian Thoracic Society; COPD, chronic obstructive pulmonary disease; FEV 1 , forced expiratory volume in one second; FVC, forced vital capacity; LABA, long-acting β-agonist; LAMA, long-acting muscarinic antagonist; ICS, inhaled corticosteroids; SAMA, short-acting muscarinic antagonist; SABA, short-acting β-agonist; SM, self-management.
Pharmacological approach
In patients with moderate-to-severe COPD, the use of LABA or LAMA compared with placebo or short-acting bronchodilators is recommended to prevent acute exacerbations (Grades 1B and 1A, respectively). 2 , 6 , 7 LAMAs are associated with a lower rate of exacerbations compared with LABAs (Grade 1C). 2 , 6 The inhaler technique needs to be checked and a suitable device selected. If our patient does not respond to optimizing inhaled medication and continues to have two to three exacerbations per year, there are additional options that offer pulmonary rehabilitation and other forms of pharmacological therapy, such as a macrolide, theophylline, phosphodieseterase (PDE4) inhibitor or N -acetylocysteine/carbocysteine, 2 although there is no information about their relative effectiveness and the order in which they should be prescribed. The choice of prescription should be guided by the risk/benefit for a given individual, and drug availability and/or cost within the health care system.
Non-pharmacological approach
A comprehensive patient-centred approach based on the chronic care model could be of great value. 2 , 8
This should include the following elements
Vaccinations: the 23-valent pneumococcal vaccine and annual influenza vaccine are suggested as part of the overall medical management in patients with COPD. 2 Although there is no clear COPD-specific evidence for the pneumococcal vaccine and the evidence is modest for influenza, the CHEST/CTS Guidelines concur with advice of the World Health Organization (WHO) 9 and national advisory bodies, 10 – 12 and supports their use in COPD patients who are at risk for serious infections. 2
Smoking cessation (including counselling and treatment) has low evidence for preventing exacerbations (Grade 2C). 2 However, the benefits from smoking cessation are outstanding as it improves COPD prognosis, slows lung function decline and improves the quality of life and symptoms. 1 , 2 , 13 , 14 Our patient has struggled to quit in the past; assessing current readiness to quit, and encouraging and supporting a future attempt is a priority in his care.
Pulmonary rehabilitation (based on exercise training, education and behaviour change) in people with moderate-to-very-severe COPD, provided within 4 weeks of an exacerbation, can prevent acute exacerbations (Grade 1C). 2 Pulmonary rehabilitation is also an effective strategy to improve symptoms, the quality of life and exercise tolerance, 15 , 16 and our patient should be encouraged to attend a course.
Self-management education with a written action plan and supported by case management providing regular direct access to a health care specialist reduces hospitalisations and prevents severe acute exacerbations (Grade 2C). 2 Some patients with good professional support can have an emergency course of steroids and antibiotics to start at the onset of an exacerbation in accordance with their plan.
Finally, close follow-up is needed for our patient as he was inadequately treated, relapsed from smoking cessation after a few days despite varenicline, and missed his follow-up appointment. A more alert health care team may have been able to identify these issues, avoid his relapse and take a timely approach to introducing additional measures to prevent his recurrent acute exacerbations.
Case study 2: A 74-year-old man with very severe COPD living alone in a remote community
A 74-year-old man has a routine telephone consultation with the respiratory team. He has very severe COPD (his FEV 1 2 years ago was 24% of predicted) and he copes with the help of his daughter who lives in the same remote community. He quit smoking the previous year after an admission to the hospital 50 miles away, which he found very stressful. He and his family managed another four exacerbations at home with courses of steroids and antibiotics, which he commenced in accordance with a self-management plan provided by the respiratory team.
His usual therapy consists of regular long-acting β 2 -agonist/inhaled steroid combination and a long-acting anti-muscarinic. He has a number of other health problems, including coronary heart disease and osteoarthritis and, in recent times, his daughter has become concerned that he is becoming forgetful. He manages at home by himself, steadfastly refusing social help and adamant that he does not want to move from the home he has lived in for 55 years.
This is a common clinical scenario, and a number of important issues require attention, with a view to optimising the management of this 74-year-old man suffering from COPD. He has very severe obstruction, is experiencing frequent acute flare-ups, is dependent and isolated and has a number of co-morbidities. To work towards preventing future exacerbations in this patient, a comprehensive plan addressing key medical and self-care issues needs to be developed that accounts for his particular context.
Optimising medical management
According to the CHEST/CTS Guidelines for prevention of acute exacerbations of COPD, 2 this patient should receive an annual influenza vaccination and may benefit from a 23-valent pneumococcal vaccine (Grades 1B and 2C, respectively). Influenza infection is associated with greater risk of mortality in COPD, as well as increased risk of hospitalisation and disease progression. 1 A diagnosis of COPD also increases the risk for pneumococcal disease and related complications, with hospitalisation rates for patients with COPD being higher than that in the general population. 10 , 17 Although existing evidence does not support the use of this vaccine specifically to prevent exacerbations of COPD, 1 administration of the 23-valent pneumococcal vaccine is recommended as a component of overall medical management. 9 – 12
Long-term oxygen therapy has been demonstrated to improve survival in people with chronic hypoxaemia; 18 it would be helpful to obtain oxygen saturation levels and consider whether long-term oxygen therapy would be of benefit to this patient.
Even though this patient is on effective medications, further optimisation of pharmacologic therapy should be undertaken, including reviewing administration technique for the different inhaler devices. 19 Maintenance PDE4 inhibitors, such as roflumilast or theophyllines, long-term macrolides (i.e., azithromycin) or oral N -acetylcysteine are potential considerations. Each of these therapeutic options has demonstrated efficacy in preventing future acute exacerbations, although they should be used with caution in this frail elderly man. 2 This patient would benefit from a review of co-morbidities, including a chest X-ray, electrocardiogram, memory assessment and blood tests including haemoglobin, glucose, thyroid and renal function assessments.
Pulmonary rehabilitation, supported self-management and tele-health care
Pulmonary rehabilitation for patients who have recently experienced an exacerbation of COPD (initiated <4 weeks following the exacerbation) has been demonstrated to prevent subsequent exacerbations (Grade 1C). 2 Existing evidence suggests that pulmonary rehabilitation does not reduce future exacerbations when the index exacerbation has occurred more than 4 weeks earlier; 2 however, its usefulness is evident in other important patient-centred outcomes such as improved activity, walking distance and quality of life, as well as by reduced shortness of breath. It would be appropriate to discuss this and enable our patient to enrol in pulmonary rehabilitation.
The patient’s access to pulmonary rehabilitation in his remote location, however, is likely to be limited. Several reports have noted that only one to two percent of people with COPD are able to access pulmonary rehabilitation programmes within Canada, 20 the United States 21 and the United Kingdom. 22 Alternatives to hospital-based pulmonary rehabilitation programmes, such as home-based programmes or programmes offered via tele-health, may be options for this patient. 23 Home-based pulmonary rehabilitation programmes have been found to improve exercise tolerance, symptom burden and quality of life. 24 – 27 Outcomes of a pulmonary rehabilitation programme offered via tele-health have also been found to be comparable to those of a hospital-based programme, 28 and may be worth exploring.
Written self-management (action) plans, together with education and case management, are suggested in the CHEST/CTS guidelines as a strategy to reduce hospitalisation and emergency department visits attributable to exacerbations of COPD (Grade 2B). 2 Our patient has an existing action plan, which has enabled him and his family to manage some exacerbations at home. Although the patient has likely had some education on COPD and its management in the past, on-going reinforcement of key principles may be helpful in preventing future exacerbations.
The self-management plan should be reviewed regularly to ensure the advice remains current. The patient’s ability to use the self-management plan safely also needs to be assessed, given his daughter’s recent observation of forgetfulness and his living alone. Cognitive impairment is being increasingly recognised as a significant co-morbidity of COPD. 29 , 30 Patients who were awaiting discharge from hospital following an exacerbation of COPD were found to perform significantly worse on a range of cognitive functional measures than a matched group with stable COPD, a finding that persisted 3 months later. 29 Cognitive impairment may contribute independently to the risk for future exacerbations by increasing the likelihood of incorrect inhaler device use and failure to adhere to recommended treatments. 29
Given that this patient resides in a remote location, access to case management services that assist in preventing future exacerbations may be difficult or impossible to arrange. Although there is currently insufficient evidence that in general the use of telemonitoring contributes to the prevention of exacerbations of COPD, 2 tele-health care for this remotely located patient has potential to allow for case management at a distance, with minimal risk to the patient. Further study is needed to address this potential benefit.
Assessing for and managing frailty
Recognising this patient’s co-morbid diagnoses of coronary heart disease and osteoarthritis, careful assessment of functional and self-care abilities would be appropriate. Almost 60% of older adults with COPD meet the criteria for frailty. 31 Frailty is defined as a dynamic state associated with decline of physiologic reserves in multiple systems and inability to respond to stressful insults. 32 Frailty is associated with an increased risk for institutionalisation and mortality. 33 , 34 Given the complex needs of those who are frail, screening this patient for frailty would constitute patient-centred and cost-effective care. Frailty assessment tools, such as the seven-point Clinical Frailty Index, 35 may provide structure to this assessment.
Admission to a hospital 50 miles away from our patient’s home last year for an exacerbation was stressful. Since his hospitalisation, this patient has experienced four additional exacerbations that have been managed at home in his remote community. It would be appropriate to explore the patient’s treatment wishes and determine whether the patient has chosen to refuse further hospitalisations. Our patient’s risk of dying is significant, with risk factors increasing the risk of short-term mortality following an exacerbation of COPD (GOLD Stage 4, age, male sex, confusion). 36 Mortality rates between 22 and 36% have been documented in the first and second years, respectively, following an exacerbation, 37 , 38 which also increase with the frequency and severity of hospitalisations. 39
Our patient has refused social help and does not want to be relocated from his home. Ageing in their own home is a key goal of many older adults. 40 , 41 Efforts to ensure that adequate resources to support the patient are available (and to support the daughter who is currently providing a lot of his care) will form an important part of the plan of care.

Case study 3: A 62-year-old woman with severe COPD admitted with an exacerbation
A 62-year-old lady is admitted for the third time this year with an acute exacerbation of her severe COPD. Her FEV 1 was 35% predicted at the recent outpatient visit. She retired from her job as a shop assistant 5 years ago because of her breathlessness and now devotes her time to her grandchildren who ‘exhaust her’ but give her a lot of pleasure.
She quit smoking 5 years ago. Over the years, her medication has increased, as nothing seemed to relieve her uncomfortable breathlessness, and, in addition to inhaled long-acting β 2 -agonist/ inhaled steroid combination and a long-acting anti-muscarinic, she is taking theophylline and carbocysteine, although she is not convinced of their beneficial effect. Oral steroid courses help her dyspnoea and she has taken at least six courses this year: she has an action plan and keeps an emergency supply of medication at home.
A secondary care perspective on the management strategy for this woman
Acute exacerbations of COPD have serious negative consequences for health care systems and patients. The risk of future events and complications, such as hospital admission and poor patient outcomes (disability and reduced health status), can be improved through a combination of non-pharmacological and pharmacological therapies. 2
Evaluation of the patient, risk assessment and adherence to medication
The essential first step in the management of this lady (as for any patient) includes a detailed medical evaluation. Our patient has a well-established diagnosis of COPD with severe airflow obstruction (GOLD grade 3), significant breathlessness that resulted in her retiring from her job, and recurrent exacerbations. She does not have significant co-morbidity, although this requires to be confirmed. Further to the medical evaluation, it is important to assess her actual disease management (medication and proper use) as well as making sure she has adopted a healthy lifestyle (smoking cessation, physical activities and exercise). Does she live in a smoke-free environment? Effect of and evidence for smoking cessation in the prevention of acute exacerbations of COPD is low, but evidence exists for a reduction in cough and phlegm after smoking cessation and less lung function decline upon sustained cessation. With respect to the medication, never assume that it is taken as prescribed. When asking the patient, use open questions such as ‘I would like to hear how you take your medication on a typical day?’ instead of ‘Did you take the medication as prescribed’. Open questions tend to elicit more useful and pertinent information, and invite collaboration. Asking the patient to demonstrate her inhalation technique shows you the way she uses her different inhalation devices.
Optimising the pharmacological therapy
The second step is to assess whether the patient is on optimal treatment to prevent exacerbations. In other words, can we do better helping the patient manage her disease and improving her well-being. As in the previous cases, vaccination, in particular, annual administration of the influenza vaccine, should be prescribed for this lady. We should evaluate other alternatives of pharmacological therapy that could improve symptoms, prevent exacerbations and reduce the use of repeated systemic corticosteroids with their important adverse effects (such as osteoporosis, cataracts, diabetes). Prescribing a PDE4 inhibitor (Grade 2A) or a long-term macrolide (Grade 2A) once a day would be a consideration for this lady. 2 As there is no superiority trial comparing these two medications, our preference will be based on potential side effects, as well as cost and access to treatment. For PDE4 inhibitors, there are limited data on supplemental effectiveness in patients with COPD and chronic bronchitis concurrently using inhaled therapies, and they potentially have side effects such as diarrhoea, nausea, headache and weight loss. The side effects tend to diminish over time, but some patients may have to discontinue the therapy. Long-term macrolides have been studied in COPD patients already treated with inhaled therapies and shown to be effective, although clinicians need to consider in their individual patients the potential for harm, such as prolongation of the QT interval, hearing loss and bacterial resistance. Furthermore, the duration (beyond 1 year) and exact dosage of macrolide therapy (for example, once daily versus three times per week) are unknown.
Making non-pharmacological therapy an essential part of the management
The third step, often neglected in the management of COPD patients, is non-pharmacological therapy. For this lady, we suggest self-management education with a written action plan and case management to improve how she deals with exacerbations (Grade 2B). 2 The expectation will not be to reduce exacerbations but to prevent emergency department visits and hospital admissions. However, despite general evidence of efficacy, 42 not all self-management interventions have been shown to be effective or to benefit all COPD patients 43 , 44 (some have been shown to be potentially harmful 44 ). The effectiveness of any complex intervention such as self-management in COPD critically depends on the health care professionals who deliver the intervention, as well on the patient and the health care system. The patient may not have the motivation or desire to change or to commit to an intensive programme. The individual patient’s needs, preferences and personal goals should inform the design of any intervention with a behavioural component. For this lady, it is essential to apply integrated disease management and to refer the patient to a pulmonary rehabilitation programme. Pulmonary rehabilitation has high value, including reducing the risk for hospitalisation in COPD patients with recent exacerbations (Grade 1C). 2 The most important benefits our patient can expect from participating in structured supervised exercise within pulmonary rehabilitation are improved health status, exercise tolerance and a reduction in dyspnoea (Grade 1A). 2 , 15 Pulmonary rehabilitation programmes provide clinicians with an opportunity to deliver education and self-management skills to patients with COPD, and are well established as a means of enhancing standard therapy to control and alleviate symptoms, optimise functional capacity and improve health-related quality of life.
Case study 4: A 52-year-old lady with moderate COPD—and possibly asthma
A 52-year-old lady attends to discuss her COPD and specifically the problem she is having with exacerbations and time ‘off sick’. She is a heavy smoker, and her progressively deteriorating lung function suggests that she has moderate COPD, although she also has a history of childhood asthma, and had allergic rhinitis as a teenager. Recent spirometry showed a typical COPD flow-volume loop, although she had some reversibility (250 ml and 20%) with a post-bronchodilator FEV 1 of 60% predicted.
She has a sedentary office job and, although she is breathless on exertion, this generally does not interfere with her lifestyle. The relatively frequent exacerbations are more troublesome. They are usually triggered by an upper respiratory infection and can take a couple of weeks to recover. She has had three exacerbations this winter, and as a result her employer is not happy with her sickness absence record and has asked her to seek advice from her general practitioner.
She has a short-acting β 2 -agonist, although she rarely uses it except during exacerbations. In the past, she has used an inhaled steroid, but stopped that some time ago as she was not convinced it was helping.
It is a welcome opportunity when a patient comes to discuss her COPD with a particular issue to address. With a history of childhood asthma, and serial COPD lung function tests, she has probably been offered many components of good primary care for COPD, but has not yet fully engaged with her management. We know that ~40% of people with COPD continue to smoke, and many are intermittent users of inhaled medications. 45 It is easy to ignore breathlessness when both job and lifestyle are sedentary.
Understanding her diagnosis and setting goals
Her readiness to engage can be supported by a move to structured collaborative care, enabling the patient to have the knowledge, resources and support to make the necessary changes. Much of this can be done by the primary care COPD team, including the pharmacist. Regular recall to maintain engagement is essential.
The combination of childhood asthma, rhinitis and a long history of smoking requires diagnostic review. This might include serial peak flows over 2 weeks to look for variability, and a chest X-ray, if not done recently, to rule out lung cancer as a reason for recent exacerbations. Her spirometry suggests moderate COPD, 1 , 46 but she also has some reversibility, not enough to place her in the asthma camp but, combined with her past medical history, being enough to explore an asthma COPD overlap syndrome. This is important to consider as it may guide decisions on inhaled medication, and there is evidence that lung function deteriorates faster in this group. 47 It is estimated that up to 20% of patients have overlap diagnoses, although the exact prevalence depends on the definition. 48
Reducing the frequency of exacerbations
Exacerbations in COPD are debilitating, often trigger hospital admission and hasten a progressive decline in pulmonary function. 2 Written information on interventions that can slow down the course of COPD and reduce the frequency and impact of exacerbations will help to support progressive changes in management.
Smoking cessation
Few people are unaware that cessation of smoking is the key intervention for COPD. Reducing further decline in lung function will slow down the severity of exacerbations. Finding a smoking cessation programme that suits her working life, exploring previous attempts at cessation, offering pharmacotherapy and a non-judgemental approach to further attempts at stopping are crucial.
Immunisations
Many, but not all, exacerbations of COPD are triggered by viral upper respiratory tract infections. Annual flu immunisation is a part of regular COPD care and reduces exacerbations and hospitalisation when flu is circulating (Grade 1B). Pneumococcal immunisation should be offered, although evidence for reducing exacerbations is weak; those with COPD will be at greater risk for pneumococcal infection. 2
Pulmonary rehabilitation
Pulmonary rehabilitation improves symptoms, quality of life and reduces hospital admission. 49 It is most efficacious in patients who are symptomatic (MRC dyspnoea scale 3 and above) and in terms of reducing exacerbations is most effective when delivered early after an exacerbation (Grade 1C). 2 The major hurdle is encouraging patients to attend, with most programmes showing an attrition rate of 30% before the first appointment, and high rates of non-completion. 45 , 50 Effective programmes that maintain the gains from aerobic exercise are more cost-effective than some of the inhaled medications in use (see Figure 3 ). 50
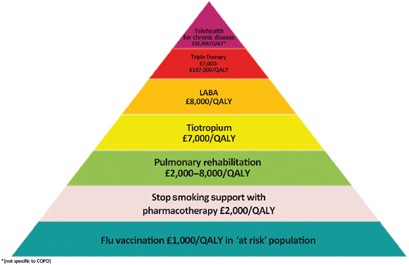
The COPD value pyramid (developed by the London Respiratory Network with The London School of Economics and reproduced with permission from the London Respiratory Team report 2013). 48 This 'value' pyramid reflects what we currently know about the cost per QALY of some of the commonest interventions in COPD. It was devised as a tool for health care organisations to use to promote audit and to ensure adequate commissioning of non-pharmacological interventions. COPD, chronic obstructive pulmonary disease; LABA, long-acting β-agonist; QALY, quality-adjusted life-year.
Inhaled medication is likely to improve our patient’s breathlessness and contribute to a reduction in exacerbation frequency. Currently, she uses only a short-acting β 2 -agonist. One wonders if she has a spacer? How much of the medicine is reaching her lungs? Repeated observation and training in inhaler use is essential if patients are to benefit from expensive medications.
With her history of asthma and evidence of some reversibility, the best choice of regular medication may be a combination of inhaled corticosteroid and a LABA. Guidelines suggest the asthma component in asthma COPD overlap syndrome should be the initial treatment target, 48 and a LABA alone should be avoided. Warn about oral thrush, and the increased risk for pneumonia. 46 If she chooses not to use an inhaled steroid, then a trial of a LAMA is indicated. Both drugs reduce exacerbation rates. 2 , 51
Finally, ensuring early treatment of exacerbations speeds up recovery. 52 Prescribe rescue medication (a 5–7-day course of oral steroids and antibiotic) to be started when symptomatic, and encourage attendance at a post-exacerbation review.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. Updated 2014. http://www.goldcopd.org. Accessed January 2015.
Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P et al. Prevention of acute exacerbations of chronic obstructive pulmonary disease: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest 2015; 147 : 894–942.
Article Google Scholar
Fletcher CM . Standardised questionnaire on respiratory symptoms: a statement prepared and approved by the MRC Committee on the Aetiology of Chronic Bronchitis (MRC breathlessness score). BMJ 1960; 2 : 1665.
Google Scholar
Jones PW, Harding G, Berry P, Wiklund I, Chen W-H, Leidy NK . Development and first validation of the COPD Assessment Test. Eur Respir J 2009; 34 : 648–654.
Article CAS Google Scholar
Gruffydd-Jones K . GOLD guidelines 2011: what are the implications for primary care? Prim Care Respir J 2012; 21 : 437–441.
Chong J, Karner C, Poole P . Tiotropium versus long-acting beta-agonists for stable chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2012; 9 : CD009157.
Cheyne L, Irvin-Sellers MJ, White J . Tiotropium versus ipratropium bromide for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2013; 9 : CD009552.
Bodenheimer T, Wagner EH, Grumbach K . Improving primary care for patients with chronic illness. JAMA 2002; 288 : 1775–1779.
World Health Organization. 23-valent pneumococcal polysaccharide vaccine. WHO position paper. Wkly Epidemiol Rec 2008; 83 : 373–384.
Center for Disease Control and Prevention Pneumococcal vaccination. http://www.cdc.gov/vaccines/vpd-vac/pneumo/ . Accessed January 2015.
Public Health England (2014a) Immunisation against infectious disease - "The Green Book". Chapter 19 - Influenza. https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book . Accessed January 2015.
Public Health Agency of Canada. Canadian immunization guide: Pneumococcal vaccine, 2014. http://www.phac-aspc.gc.ca/publicat/cig-gci/p04-pneu-eng.php . Accessed January 2015.
Fletcher C, Peto R . The natural history of chronic airflow obstruction. Br Med J 1977; 1 : 1645–1648.
Hersh CP, DeMeo DL, Al-Ansari E, Carey VJ, Reilly JJ, Ginns LC et al. Predictors of survival in severe, early onset COPD. Chest 2004; 126 : 1443–1451.
Lacasse Y, Goldstein R, Lasserson TJ, Martin S . Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006; (4): CD003793.
Lacasse Y, Wong E, Guyatt GH, King D, Cook DJ, Goldstein RS . Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. Lancet 1996; 348 : 1115–1119.
Lee T, Weaver F, Weiss K . Impact of pneumococcal vaccination on pneumonia rates in patients with COPD and asthma. J Gen Intern Med 2007; 22 : 62–67.
Crockett AJ, Cranston JM, Moss JR, Allpers JH . A review of long-term oxygen therapy for chronic obstructive pulmonary disease. Respir Med 2001; 95 : 437–443.
Newman SP . Inhaler treatment options in COPD. Eur Respir Rev 2005; 96 : 102–108.
Brooks D, Sottana R, Bell B, Hanna M, Laframboise L, Selvanayagarajah S et al. Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J 2007; 14 : 87–92.
Bickford LS, Hodgkin JE, McInturff SL . National pulmonary rehabilitation survey. Update. J Cardiopulm Rehabil 1995; 15 : 406–411.
Yohannes AM, Connolly MJ . Pulmonary rehabilitation programmes in the UK: a national representative survey. Clin Rehabil 2004; 18 : 444–449.
Marciniuk DD, Brooks D, Butcher S, Debigare R, Dechman G, Ford G et al. Optimizing pulmonary rehabilitation in chronic obstructive pulmonary disease – practical issues: a Canadian Thoracic Society Clinical Practice Guideline. Can Respir J 2010; 17 : 159–168.
Guell M, De-Lucas P, Galdiz J, Montemayor T, Rodriguez Gonzalez-Moro J, Gorostiza A . Home vs hospital-based pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: disease: a Spanish multicentre trial. Arch Bronconeumol 2008; 44 : 512–518.
Maltais F, Bourbeau J, Shapiro S, Lacasse Y, Perrault H, Baltzan M . Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2008; 149 : 869–878.
Puente-Maestu L, Sanz M, Sanz P, Cubillo J, Mayol J, Casaburi R . Comparison of effects of supervised versus self-monitored training programmes in patients with chronic obstructive pulmonary disease. Eur Respir J 2000; 15 : 517–525.
Strijbos J, Postma D, Van-Altena R, Gimeno F, Koeter G . A comparison between an outpatient hospital-based pulmonary rehabilitation program and a home-care pulmonary rehabilitation program in patients with COPD. A follow-up of 18 months. Chest 1996; 109 : 366–372.
Stickland M, Jourdain T, Wong EY, Rodgers WM, Jendzjowsky NG, MacDonald GF . Using Telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Can Respir J 2011; 18 : 216–220.
Dodd JW, Getov SV, Jones PW . Cognitive function in COPD. Eur Respir J 2010; 35 : 913–922.
Cleutjens FA, Spruit MA, Ponds RW, Dijkstra JB, Franssen FM, Wouters EF et al. Cognitive functioning in obstructive lung disease: results from the United Kingdom biobank. J Am Med Dir Assoc 2014; 15 : 214–219.
Park SK, Richardson CR, Holleman RG, Larson JL . Frailty in people with COPD, using the National Health and Nutrition Evaluation Survey dataset (2003-2006). Heart Lung 2013; 42 : 163–170.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G . Untangling the concepts of disability, frailty and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004; 59 : 255–263.
Lahousse L, Maes B, Ziere G, Loth DW, Verlinden VJ, Zillikens MC et al. Adverse outcome of frailty in the elderly: the Rotterdam Study. Eur J Epidemiol 2014; 29 : 419–427.
Rockwood K, Howlett SE, MacKnight C, Beattie BL, Bergman H, Hebert R et al. Prevalence, attributes and outcomes of fitness and frailty in community-dwelling older adults: report from the Canadian study of health and aging. J Gerontol A Biol Sci Med Sci 2004; 59 : 1310–1317.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005; 173 : 489–495.
Singanayagam A, Schembri S, Chalmers JD . Predictors or mortality in hospitalized adults with acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc 2013; 10 : 81–89.
Almagro P, Calbo E, Ochoa de Echaguen A, Barreiro B, Quintana S, Heredia JL et al. Mortality after hospitalization for COPD. Chest 2002; 121 : 1441–1448.
Groenewegen KH, Schols AM, Wouters EF . Mortality and mortality-related factors after hospitalization for acute exacerbation of COPD. Chest 2003; 124 : 459–467.
Soler-Cataluna JJ, Martinez-Garcia MA, Sanchez PR, Salcedo E, Navarro M, Ochando R . Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 2005; 60 : 925–931.
Ball MM, Perkins MM, Whittington FJ, Connell BR, Hollingsworth C, King SV et al. Managing decline in assisted living: the key to aging in place. J Gerontol B Psychol Sci Soc Sci 2004; 59 : S202–S212.
Pynoos J, Caraviello R, Cicero C . Lifelong housing: the anchor in aging-friendly communities. Generations 2009; 33 : 26–32.
Zwerink M, Brusse-Keizer M, van der Valk PD, Zielhuis GA, Monninkhof EM, van der Palen J et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014; 3 : CD002990.
Bucknall CE, Miller G, Lloyd SM, Cleland J, McCluskey S, Cotton M et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ 2012; 344 : e1060.
Fan VS, Gaziano JM, Lew R, Bourbeau J, Adams SG, Leatherman S et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med 2012; 156 : 673–683.
Hull S, Mathur R, Lloyd-Owen S, Round T, Robson J . Improving outcomes for people with COPD by developing networks of general practices: evaluation of a quality improvement project in east London. NPJ Prim Care Respir Med 2014; 24 : 14082.
National Institute of Health and Clinical Excellence. Management of chronic obstructive pulmonary disease in adults in primary and secondary care. Updated 2010. NICE CG101. http://www.nice.org.uk/ . Accessed January 2015.
Gibson PG, Simpson JL . The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax 2009; 64 : 728–735.
Global INitiative for Asthma. Asthma, COPD and asthma-COPD overlap syndromes (ACOS). GINA 2014. http://www.ginasthma.org/documents/14 . Accessed January 2015.
Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA et al. Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines. Chest 2007; 131 (5 Suppl): 4S–42S.
London Respiratory Team. Take a breath in, keep it in and now try to breathe again. NHS England, 2013. http://www.networks.nhs.uk/nhs-networks/london-respiratory-network . Accessed January 2015.
Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American College of Chest Physicians task force. Chest 2006; 129 : 174–181.
Wilkinson TM, Donaldson GC, Hurst JR, Seemungal TA, Wedzicha JA . Early therapy improves outcomes of exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004; 169 : 1298–1303.
Download references
Acknowledgements
The authors declare that no funding was received.
Author information
Authors and affiliations.
Agia Barbara Health Care Center, Heraklion, Crete, Greece
Ioanna Tsiligianni
Department of Thoracic Medicine, Clinic of Social and Family Medicine, University of Crete, Heraklion, Crete, Greece
Department of Medicine, College of Medicine, University of Saskatchewan, Saskatoon, SK, Canada
Donna Goodridge
Division of Respirology, Critical Care and Sleep Medicine, University of Saskatchewan, Saskatoon, SK, Canada
Darcy Marciniuk
Centre for Primary Care and Public Health, Blizard Institute, Queen Mary University of London, London, UK
Respiratory Epidemiology and Clinical Research Unit, Montreal Chest Institute, McGill University Health Centre, Montréal, QC, Canada
Jean Bourbeau
You can also search for this author in PubMed Google Scholar
Contributions
IT, DG and DM, JB, SH wrote the perspectives on case studies 1, 2, 3 and 4, respectively. The handling editor (Hilary Pinnock) collated and edited the individual sections.
Corresponding author
Correspondence to Jean Bourbeau .
Ethics declarations
Competing interests.
JB declares peer reviewed government grants (for conducting research in COPD self-management 'Living Well with COPD' and the longitudinal population-based Canadian Cohort Obstructive Lung Disease (CanCOLD) study) from Canadian Institute of Health Research Rx&D collaborative programme (Astra Zeneca, Boehringer- Ingelheim, GlaxoSmithKline, Merck, Nycomed, Novartis), Canadian Respiratory Research Network (CRRN), Respiratory Health Network of the FRQS and Research Institute of the MUHC. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
Reprints and permissions
About this article
Cite this article.
Tsiligianni, I., Goodridge, D., Marciniuk, D. et al. Four patients with a history of acute exacerbations of COPD: implementing the CHEST/Canadian Thoracic Society guidelines for preventing exacerbations. npj Prim Care Resp Med 25 , 15023 (2015). https://doi.org/10.1038/npjpcrm.2015.23
Download citation
Received : 22 February 2015
Accepted : 24 February 2015
Published : 07 May 2015
DOI : https://doi.org/10.1038/npjpcrm.2015.23
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
It takes my breath away: end-stage COPD. Part 1: a case study and an overview of COPD
Affiliation.
- 1 Palliative Care Service, Massachusetts General Hospital, Boston, MA 02115, USA. [email protected]
- PMID: 16531775
- DOI: 10.1097/00004045-200603000-00006
End-stage chronic obstructive pulmonary disease (COPD) is a progressive illness without a cure. Because of its unpredictable trajectory, prognosis is difficult as, even in end-stage disease, patients may experience exacerbations and stabilization. There are many symptoms to manage until ultimately, respiratory function is severely compromised. Home care nurses provide much of the care at home and can make a difference in promoting advanced care planning and optimal comfort. This article reviews COPD, the management of subsequent symptoms, and the role of the home care nurse.
PubMed Disclaimer
Similar articles
- It takes my breath away end-stage COPD. Part 2: pharmacologic and nonpharmacologic management of dyspnea and other symptoms. Dahlin C. Dahlin C. Home Healthc Nurse. 2006 Apr;24(4):218-24; quiz 225-6. doi: 10.1097/00004045-200604000-00008. Home Healthc Nurse. 2006. PMID: 16680051 Review. No abstract available.
- Rehabilitation for the home care patient with COPD. Cigna JA, Turner-Cigna LM. Cigna JA, et al. Home Healthc Nurse. 2005 Sep;23(9):578-84; quiz 585-6. doi: 10.1097/00004045-200509000-00009. Home Healthc Nurse. 2005. PMID: 16160553 Review.
- COPD and coping with breathlessness at home: a review of the literature. Harris S. Harris S. Br J Community Nurs. 2007 Sep;12(9):411-5. doi: 10.12968/bjcn.2007.12.9.27234. Br J Community Nurs. 2007. PMID: 18026004 Review.
- Promoting quality of life for patients with moderate to severe COPD. Tinker R, While A. Tinker R, et al. Br J Community Nurs. 2006 Jul;11(7):278-84. doi: 10.12968/bjcn.2006.11.7.21442. Br J Community Nurs. 2006. PMID: 16926707 Review.
- [Chronic obstructive lung disease and home care nurses, from preventive care to palliative care]. Hesnart N. Hesnart N. Soins. 2006 Nov;(710):47. Soins. 2006. PMID: 17225766 French. No abstract available.
- Manoeuvring along the edge of breathlessness: an ethnographic case study of two nurses. Jellington MO, Overgaard D, Sørensen EE. Jellington MO, et al. BMC Nurs. 2016 Apr 27;15:27. doi: 10.1186/s12912-016-0148-4. eCollection 2016. BMC Nurs. 2016. PMID: 27127418 Free PMC article.
Publication types
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
- Wolters Kluwer
Other Literature Sources
- The Lens - Patent Citations
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->
| | | |

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Art & Science Previous Next
Managing a patient with copd and comorbidities: a case study, rachel lucy mitten community matron, peninsula community health community matron service, newquay hospital, newquay, cornwall, england.
This case study provides a critical analysis of the management of a patient with long-term conditions in a community matron service. Particular attention is given to the effect of chronic obstructive pulmonary disease (COPD). The effect of COPD on health and wellbeing, quality of life and hospital admissions is examined, and outcomes are detailed that resulted from the implementation of evidence-based interventions and a case management approach.
Nursing Standard . 30, 13, 46-51. doi: 10.7748/ns.30.13.46.s46
All articles are subject to external double-blind peer review and checked for plagiarism using automated software.
Received: 13 February 2015
Accepted: 29 May 2015
case study - chronic obstructive pulmonary disease - community matron service - comorbidities - complex care - COPD - long-term conditions
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

25 November 2015 / Vol 30 issue 13
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Managing a patient with COPD and comorbidities: a case study
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Chronic Obstructive Pulmonary Disease (COPD) Case Study (60 min)
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mr. Whaley is a 65-year-old man with a history of COPD who presents to his primary care provider’s (PCP) office complaining of a productive cough off and on for 2 years and shortness of breath for the last 3 days. He reports that he has had several chest colds in the last few years, but this time it won’t go away. His wife says he has been feverish for a few days, but doesn’t have a specific temperature to report. He reports smoking a pack of cigarettes a day for 25 years plus the occasional cigar.
What nursing assessments should be performed at this time for Mr. Whaley?
- Full set of vital signs, including SpO2
- Heart and Lung sounds
- Gather any further details of illness or medical history, including allergies
Upon further assessment, Mr. Whaley has crackles throughout the lower lobes of his lungs, with occasional expiratory wheezes throughout the lung fields. His vital signs are as follows:
BP 142/86 mmHg HR 102 bpm
RR 32 bpm Temp 38.8°C
SpO 2 86% on room air
The nurse locates a portable oxygen tank and places the patient on 2 lpm oxygen via nasal cannula. Based on these findings, Mr. Whaley’s PCP decides to call an ambulance to send Mr. Whaley to the Emergency Department (ED). While waiting for the ambulance, the nurse repeats the SpO 2 and finds Mr. Whaley’s SpO 2 is only 89%. She increases his oxygen to 4 lpm, rechecks and notes an SpO 2 of 95%. The ambulance crew arrives, the nurse reports to them that the patient was short of breath and hypoxic, but sats are now 95% and he is resting. Per EMS, he is alert and oriented x 3.
What is going on with Mr. Whaley, physiologically?
- Mr. Whaley may have a lung infection, as evidenced by his fever and productive cough. This is causing a COPD exacerbation. COPD makes gas exchange difficult, which is why his SpO2 levels are low.
What would you have done differently? Why?
- Because of his COPD, Mr. Whaley should not have been placed on more than 2 lpm of supplemental O2 because it would decrease his respiratory drive and lead to CO2 toxicity.
- When Mr. Whaley’s sats didn’t improve, should have notified provider before adding more supplemental oxygen
Upon arrival to the ED, the RN finds Mr. Whaley is somnolent and difficult to arouse. He takes a set of vital signs and finds the following:
BP 138/78 mmHg HR 96 bpm
RR 16 bpm Temp 38.4°C
SpO 2 96% on 4 lpm nasal cannula
What is the possible cause of Mr. Whaley’s somnolence?
- His COPD makes gas exchange difficult, therefore he retains CO2. This means his respiratory drive to breathe is low O2 instead of high CO2. When the nurse gave too much supplemental oxygen, Mr. Whaley lost some of his respiratory drive. This is why his respiratory rate is so low.
- This can lead to CO2 toxicity, which presents as a decreased LOC and decreased respiratory rate, and can lead to the patient not protecting their airway and going into respiratory arrest
What orders do you expect from the ED provider?
- To remove the supplemental oxygen and only keep SpO2 between 88-92% to avoid over-oxygenating and CO2 toxicity
- Chest X-ray
- Blood Cultures, Sputum Cultures, CBC, BMP, ABG
- Bronchodilators, Corticosteroids, Breathing treatments from Respiratory Therapy
The provider writes the following orders:
Keep sats 88-92%
Labs: ABG, CBC, BMP
Insert peripheral IV
Albuterol nebulizer 2.5mg
Budesonide-formoterol 160/4.5 mcg
The nurse immediately removes the supplemental oxygen from Mr. Whaley and attempts to stimulate him awake. Mr. Whaley is still quite drowsy, but is able to awake long enough to state his full name. The nurse inserts a peripheral IV and draws the CBC and BMP, while the Respiratory Therapist (RT) draws an arterial blood gas (ABG). Blood gas results are as follows:
pCO 2 58 mmHg
HCO 3 – 30 mEq/L
pO 2 50 mmHg
Mr. Whaley’s chest x-ray shows consolidation in bilateral lower lobes.
Interpret the ABG. Explain.
- This is respiratory acidosis with partial compensation
- The ABG also shows hypoxemia
- Mr. Whaley retains CO2 chronically and his kidneys have tried to compensate (as evidenced by the HCO3- of 30 mEq/L). They weren’t able to fully compensate, though, so his pH is still acidic because of the high CO2
Which medication should be administered first? Why?
- Albuterol – because it is a bronchodilator and should always be administered before corticosteroids
Mr. Whaley’s condition improves after a bronchodilator and corticosteroid breathing treatment. His SpO 2 remains 90% on room air and his shortness of breath has significantly decreased. He is still running a fever of 38.3°C. The ED provider orders broad spectrum antibiotics for a likely pneumonia, which may have caused this COPD exacerbation. The provider also orders two inhalers for Mr. Whaley, one bronchodilator and one corticosteroid. Satisfied with his quick improvement, the provider decides it is safe for Mr. Whaley to recover at home with proper instructions for his medications and follow up from his PCP.
What are priority discharge teaching topics for Mr. Whaley?
- Mr. Whaley NEEDS to stop smoking!!!
- Proper use of inhalers, new medication instructions
- Reporting s/s respiratory infection to PCP sooner
- Pursed lip breathing and small, frequent meals to prevent shortness of breath
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies
Chronic obstructive pulmonary disease (COPD)
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Case history
Case history #1.
A 66-year-old man with a smoking history of one pack per day for the past 47 years presents with progressive shortness of breath and chronic cough, productive of yellowish sputum, for the past 2 years. On examination he appears cachectic and in moderate respiratory distress, especially after walking to the examination room, and has pursed-lip breathing. His neck veins are mildly distended. Lung examination reveals a barrel chest and poor air entry bilaterally, with moderate inspiratory and expiratory wheezing. Heart and abdominal examination are within normal limits. Lower extremities exhibit scant pitting oedema.
Case history #2
A 56-year-old woman with a history of smoking presents to her primary care physician with shortness of breath and cough for several days. Her symptoms began 3 days ago with rhinorrhoea. She reports a chronic morning cough productive of white sputum, which has increased over the past 2 days. She has had similar episodes each winter for the past 4 years. She has smoked 1 to 2 packs of cigarettes per day for 40 years and continues to smoke. She denies haemoptysis, chills, or weight loss and has not received any relief from over-the-counter cough preparations.
Other presentations
Some patients report chest tightness, which often follows exertion and may arise from intercostal muscle contraction. Weight loss, muscle loss, and anorexia are common in patients with severe and very severe COPD. [1] Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. 2024 [internet publication]. https://goldcopd.org/2024-gold-report Other presentations include fatigue, haemoptysis, cyanosis, and morning headaches secondary to hypercapnia. Chest pain and haemoptysis are uncommon symptoms of COPD and raise the possibility of alternative diagnoses. [2] National Institute for Health and Care Excellence. Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Jul 2019 [internet publication]. https://www.nice.org.uk/guidance/ng115
Physical examination may demonstrate hypoxia, use of accessory muscles, paradoxical rib movements, distant heart sounds, lower-extremity oedema and hepatomegaly secondary to cor pulmonale, and asterixis secondary to hypercapnia.
Patients may also present with signs and symptoms of COPD complications. These include severe shortness of breath, severely decreased air entry, and chest pain secondary to an acute COPD exacerbation or spontaneous pneumothorax. [1] Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. 2024 [internet publication]. https://goldcopd.org/2024-gold-report [3] Garcia-Pachon E. Paradoxical movement of the lateral rib margin (Hoover sign) for detecting obstructive airway disease. Chest. 2002 Aug;122(2):651-5. http://www.ncbi.nlm.nih.gov/pubmed/12171846?tool=bestpractice.com Patients with COPD often have other comorbidities, including cardiovascular disease, skeletal muscle dysfunction, metabolic syndrome and diabetes, osteoporosis, depression, anxiety, lung cancer, gastro-oesophageal reflux disease, bronchiectasis, obstructive sleep apnoea, and cognitive impairment. [1] Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2024 report. 2024 [internet publication]. https://goldcopd.org/2024-gold-report [4] Morgan AD, Rothnie KJ, Bhaskaran K, et al. Chronic obstructive pulmonary disease and the risk of 12 cardiovascular diseases: a population-based study using UK primary care data. Thorax. 2018 Sep;73(9):877-9. http://www.ncbi.nlm.nih.gov/pubmed/29438071?tool=bestpractice.com [5] Maltais F, Decramer M, Casaburi R, et al; ATS/ERS Ad Hoc Committee on Limb Muscle Dysfunction in COPD. An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014 May 1;189(9):e15-62. https://www.atsjournals.org/doi/10.1164/rccm.201402-0373ST http://www.ncbi.nlm.nih.gov/pubmed/24787074?tool=bestpractice.com
One UK study found that 14.5% of patients with COPD had a concomitant diagnosis of asthma, whereas a global meta-analysis estimated the pooled prevalence of asthma in patients with COPD to be 29.6% (range: 12.6% to 55.5%). [6] Nissen F, Morales DR, Mullerova H, et al. Concomitant diagnosis of asthma and COPD: a quantitative study in UK primary care. Br J Gen Pract. 2018 Nov;68(676):e775-82. https://bjgp.org/content/68/676/e775 http://www.ncbi.nlm.nih.gov/pubmed/30249612?tool=bestpractice.com [7] Hosseini M, Almasi-Hashiani A, Sepidarkish M, et al. Global prevalence of asthma-COPD overlap (ACO) in the general population: a systematic review and meta-analysis. Respir Res. 2019 Oct 23;20(1):229. https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-019-1198-4 http://www.ncbi.nlm.nih.gov/pubmed/31647021?tool=bestpractice.com
Use of this content is subject to our disclaimer
Log in or subscribe to access all of BMJ Best Practice
Log in to access all of bmj best practice, help us improve bmj best practice.
Please complete all fields.
I have some feedback on:
We will respond to all feedback.
For any urgent enquiries please contact our customer services team who are ready to help with any problems.
Phone: +44 (0) 207 111 1105
Email: [email protected]
Your feedback has been submitted successfully.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Respir Med Case Rep
Early COPD diagnosis and treatment: A case report
Associated data.
Not applicable.
Chronic obstructive pulmonary disease (COPD) refers to a group of widely diffuse diseases that cause airflow blockage characterized by persistent respiratory symptoms such as dyspnea, chronic cough, recurrent wheezing, chronic sputum production, and progressive restricted airflow associated with exacerbations. COPD is the third leading cause of death worldwide and can only be treated not cured.
Pulmonary function tests do not permit the identification of initial obstructive airways disease. Forced expiratory flow (FEF 25-75 ), which calculates obstruction severity at small and medium bronchial airways levels, allows an early COPD diagnosis.
We report a 72-year-old ex-smoker male not exposed to occupational risk with symptoms suggesting early COPD. Baseline pulmonary function tests were normal, except FEF 25-75 . The patient did not respond to the first 6 months of treatment with long-acting muscarinic antagonist (LAMA), whereas he showed a clear clinical and FEF 25-75 response to 1-year treatment with LAMA associated with long-acting β2 agonist (LABA).
This clinical case report highlights the usefulness of FEF 25-75 evaluation in early COPD diagnosis and monitoring and confirms the efficacy of LAMA–LABA association for small airways obstruction treatment.
1. Introduction
Chronic obstructive pulmonary disease (COPD) refers to a group of widely diffuse diseases, including emphysema and chronic bronchitis, that cause airflow blockage. It is characterized by persistent respiratory symptoms such as dyspnea, chronic cough, chronic production of sputum, recurrent wheezing, and restricted airflow [ 1 ]. COPD is characterized by airflow limitation that is not fully reversible. Airflow limitation is progressive and associated with abnormal inflammatory response of the lungs, particularly caused by cigarette smoking [ 2 ].
COPD is the third leading cause of death worldwide because of associated comorbidities such as smoking, environmental pollution, and occupational risk [ 3 ]. Despite accurate studies and clinical trials analyzing COPD etiology and phenotypes, currently it can only be treated not cured.
Although COPD affects the lungs, it causes systemic damages with heart involvement developing pulmonary hypertension and cor pulmonale [ 4 ].
The importance of exacerbations is closely related to COPD clinical course, and their reduction increases the outcome and improves the quality of life (QOL). Exacerbations are events requiring therapy with antibiotics, systemic steroids, or both. The severity of exacerbations is defined by the location of care such as home and emergency room or hospital. Mild exacerbations involve upper airways and are treated with adjustments in bronchodilator or inhaled corticosteroid therapy, and moderate exacerbations involve lower respiratory tracts and are treated with antibiotics and systemic corticosteroids. Based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines [ 1 ], the COPD classification of airflow limitation severity is defined as follows: (i) mild forced expiratory volume in 1 second (FEV 1 ) ≥ 80% predicted; (ii) moderate 50% ≤ FEV 1 < 80% predicted; (iii) severe 30% ≤ FEV 1 <50% predicted; and (iv) very severe FEV 1 <30% predicted. An additional sensitive parameter to evaluate early airflow obstruction in peripheral airways is forced expiratory flow (FEF) rate between 25% and 75% of forced vital capacity (FVC). The normal value of FEF 25–75% depends on age and height, and the results of FEF 25–75% are little effort-dependent and representative of air movement through small airways [ 5 , 6 ].
The aim of this clinical case is to highlight the usefulness of pulmonary function tests and particularly FEF 25–75% in early COPD diagnosis to improve therapeutic approach, reduce acute exacerbations, QOL, and disease outcome.
2. Case report
A 72-year-old ex-smoker male, 5 pack-years, was admitted with exertional dyspnea lasting 6 months and productive cough lasting 3 months suggesting early COPD. The patient was not exposed to occupational risk and was neither affected by allergy nor other relevant comorbidities. Physical chest examination showed fine rhonchi without wheezing and crackling sounds. Cyanosis was absent, and pulse oximetry was 96% in room air. No signs of cardiovascular failure were detected.
Pulmonary function tests at baseline, including FEV 1 and FEV 1 /FVC ratio, were in the normal range and did not suggest an initial obstructive airways disease. Note that the FEF 25-75 values were suggestive of moderate small airways obstruction ( Table 1 ). The patient was first treated with long-acting muscarinic antagonist (LAMA – umeclidinium bromide 65 mcg/daily). However, dyspnea and cough did not ameliorate, and the patient suffered from exacerbation responsive to antibiotics. Spirometry after 6 months of LAMA therapy showed a decrease of FEF 25-75 , especially of FEF 25 from 59% to 50%. Then, the treatment was modified using the association of LAMA with long-acting β2 agonist (LABA – vilanterol 22 mcg/daily) according to GOLD guidelines. Patient evaluation after 12 months of LAMA–LABA therapy revealed excellent response with decreased dyspnea and cough and absence of exacerbations. Spirometry showed clear regression of small airways obstructive parameters. Notably FEF 25 increased from 50% to 62% ( Table 1 and Fig. 1 ).
FEF 25-75 values before and after treatment.
| Baseline | After 6 months of LAMA therapy | After 1 year of LAMA–LABA therapy | |
|---|---|---|---|
| 59 | 50 | 62 | |
| 42 | 41 | 42 | |
| 43 | 43 | 47 |
FEF: forced expiratory flow; LAMA: long-acting muscarinic antagonist; LABA: long-acting β2 agonist.

FEF 25-75 behavior during LAMA and LAMA–LABA treatment.
3. Discussion
In the reported case, the patient's symptoms such as productive cough associated with dyspnea under exertion worsened and were poorly controlled, particularly in the course of an exacerbation occurring during 6-month LAMA therapy. The persistent symptoms required more effective treatment and led, according to GOLD guidelines, to a therapeutic change replacing LAMA alone with LAMA–LABA association [ 7 ] ( Fig. 2 ).

Efficacy of LAMA–LABA therapy in COPD.
The efficacy of umeclidinium plus vilanterol led to an evident reduction in symptoms avoiding COPD exacerbations at 6, 12, and 18 months of follow-up. The therapeutic benefit was confirmed by spirometry, particularly by FEF 25-75 increase. These findings confirm the usefulness of the association of antimuscarinic agent with LABA in COPD treatment [ 1 ].
Finding normal parameters in pulmonary function tests does not permit, as in this case, to identify an initial obstructive airways disease. Only FEF 25-75, which calculates obstruction severity at several small and medium bronchial airways levels, allows an early COPD diagnosis.
Recently, Kwon Sun et al. [ 5 ] confirmed that FEF 25-75 is reduced in early COPD and associated with small airway disease . Interestingly, the previously performed Boston early-onset COPD study identified FEF 25-75 as a potential indicator of genetic susceptibility to develop COPD. However, the same authors suggested that this measure does not provide information beyond FEV 1 /FVC for demonstrating small airways disease [ 8 ] .
Note that many clinical trials assessing COPD diagnosis and treatment used only FVC and FEV 1 to evaluate the severity of airways obstruction and therapeutic response [ 3 , [9] , [10] , [11] , [12] , [13] , [14] ].
The hallmarks of the present case are that it (i) underlines that FEF 25-75 decrease is the earliest and sensitive pulmonary function test parameter suggesting COPD diagnosis; (ii) FEF 25-75 decrease reflects the loss of elastic recoil and air trapping from emphysema and COPD small airways; and (iii) highlights that lower FEF 25-75 is closely associated with an increase in COPD severity, providing new knowledge of pathophysiological and anatomical mechanisms that lead to clinical outcomes in COPD [ 6 ].
Authors’ contributions
RGC and GB: conceptualization and investigation. FP: reviewing and editing.
Ethics approval
Consent to publication, availability of data and material.
University of Genoa Grant n.:100007-2020-SD-FRA_001.
Declaration of competing interest
The Authors do not have any conflict of interest.
Handling Editor: DR AC Amit Chopra
Abbreviations
This site is intended for health professionals only

- Newsletter sign up
- Nursing in Practice 365
CPD: Case by case – measles and whooping cough

- The characteristic presenting symptoms of measles and whooping cough in children and adults, and how to distinguish them from other potential infectious diseases
- How cases should be diagnosed and managed in primary care, including appropriate treatment for suspected or confirmed cases
- Appropriate public health measures to take if suspected cases of measles or whooping cough present to you, including infection and prevention control measures and how to notify appropriate bodies
- Prevention of measles and whooping cough through vaccination; why and when vaccinations are recommended and how to advise patients who have missed their vaccinations

See how our symptom tool can help you make better sense of patient presentations Click here to search a symptom

Receive the latest news, clinical updates and case studies straight to your inbox.
SIGN UP TODAY
Related articles

Most Popular
1 Supporting lung cancer screening in the community
2 Another baby dies from whooping cough as cases surpass 10,000
3 Festival nursing: ‘You can have so much fun doing something you love’
4 Use school nurses to deliver immunisations, think-tank report urges

IMPORTANT LINKS
- Subscribe to newsletters
- Privacy policy
- Terms and conditions
- Yellow Card reporting
MORE FROM COGORA
- Pulse Today
- The Pharmacist
- Management in Practice
- Healthcare Leader
- Hospital Healthcare Europe
- Hospital Pharmacy Europe
© Cogora 2024 Cogora Limited. 1 Giltspur Street, London EC1A 9DD Registered in the United Kingdom. Reg. No. 2147432
Nursing in Practice newsletters
Sign up today to receive the latest news, business insight, blogs and case studies via newsletters as it happens.

IMAGES
VIDEO
COMMENTS
Diagnosis involves taking a patient history and performing spirometry testing. Spirometry identifies airflow obstruction by measuring the volume of air that can be exhaled. Chronic obstructive pulmonary disease is managed with lifestyle and pharmacological interventions, as well as self-management. Abstract This article uses a case study to ...
Nurse Seema works on a medical-surgical unit and is caring for Richard, a 75-year-old male with a history of smoking, who was admitted for an acute exacerbation of chronic obstructive pulmonary disease, or COPD. After settling Richard in his room, Nurse Seema goes through the steps of the Clinical Judgment Measurement Model to make clinical ...
On examination, the temperature was 37.9°C, the blood pressure 157/95 mm Hg, the pulse 112 beats per minute, the respiratory rate 30 breaths per minute, and the oxygen saturation 91% while the ...
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
COPD: a case study Authors Debbie Price is lead practice nurse, Llandrindod Wells Medical Practice; Nikki Williams is associate professor of respiratory and sleep physiology, Swansea University. Abstract This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient's
SpO286% on room air. The nurse locates a portable oxygen tank and places the patient on 2 lpm oxygen via nasal cannula. Based on these findings, Mr. Whaley's PCP decides to call an ambulance to send Mr. Whaley to the Emergency Department (ED). While waiting for the ambulance, the nurse repeats the SpO2 and finds Mr. Whaley's SpO2 is only 89%.
Patient and family teaching is an important nursing intervention to enhance self-management in patients with any chronic pulmonary disorder. To achieve airway clearance: The nurse must appropriately administer bronchodilators and corticosteroids and become alert for potential side effects. Direct or controlled coughing.
1. INTRODUCTION. Chronic obstructive pulmonary disease (COPD) is a global problem and a major cause of chronic morbidity and mortality (Global initiative for chronic obstructive lung disease, GOLD 2016).In Sweden, approximately 500,000 people are expected to suffer from COPD and over 2,000 lose their lives every year because of the disease (Swedish Pulmonary Organization 2017).
Background. Chronic obstructive pulmonary disease (COPD) is a disease with a significant morbidity and mortality worldwide. 1 It is characterised by progressive airflow limitation that is not fully reversible and is caused by pathophysiological processes including the destruction of the alveolar walls which leads to the development of bullous emphysema. 2 Acute exacerbations are common among ...
Pulse oximetry is used to determine arterial oxygen saturation and need for supplemental oxygen. It should be used in patients with clinical signs of acute respiratory failure. If peripheral arterial oxygen saturation is less than 92%, ABGs should be assessed. 24,25. Exercise testing and physical activity assessment.
Based on the information given, the patient likely has chronic obstructive pulmonary disease (COPD). The key findings that point to this diagnosis include: Barrel chest. Tachypnea. A long expiratory time. Diminished breath sounds. Use of accessory muscles while breathing. Digital clubbing. Pursed lip breathing.
41. Mr. Jake Dogson is a 62 year old male with a history of chronic obstructive pulmonary disease (COPD), hypertension, and hyperlipidemia. He was a previous smoker for forty years; he quit when he was diagnosed with COPD 10 years ago. His home medications include ipratroprium via nebulizer once a day, albuterol quick-relief inhaler, metoprolol ...
Case study 1: A 63-year-old man with moderate/severe COPD and a chest infection A 63-year-old self-employed plumber makes a same-day appointment for another 'chest infection'.
This page titled 2: Case Study #1- Chronic Obstructive Pulmonary Disease (COPD) is shared under a CC BY-SA 4.0 license and was authored, remixed, and/or curated by Glynda Rees, Rob Kruger, and Janet Morrison via source content that was edited to the style and standards of the LibreTexts platform.
The inclusion criteria were: (a) observational studies (case-control, cohort and cross-sectional) or intervention study (randomized or non-randomized); (b) manuscripts that analyzed patients who had COPD or diseases characterized by airflow limitation of a progressive and not easily reversible nature; (c) studies in which nursing-led ...
End-stage chronic obstructive pulmonary disease (COPD) is a progressive illness without a cure. Because of its unpredictable trajectory, prognosis is difficult as, even in end-stage disease, patients may experience exacerbations and stabilization. There are many symptoms to manage until ultimately, respiratory function is severely compromised.
This case sudy aims to demonstrate the care given to a patient who when attending for a new patient check was found to have Chronic Obstructive Pulmonary Disease (COPD). It shows the nurses involvement in the primary care setting in recognizing COPD and how valuable structured assessment can be in helping patients with this distressing condition.
The effect of COPD on health and wellbeing, quality of life and hospital admissions is examined, and outcomes are detailed that resulted from the implementation of evidence-based interventions and a case management approach. Nursing Standard . 30, 13, 46-51. doi: 10.7748/ns.30.13.46.s46. [email protected].
Nursing case study on COPD & learn everything you will need to about to ace your NCLEX questions. View the online lesson today! Chronic Obstructive Pulmonary Disease (COPD) Case Study (60 min) ... Mr. Whaley is a 65-year-old man with a history of COPD who presents to his primary care provider's (PCP) office complaining of a productive cough ...
Case history #1. A 66-year-old man with a smoking history of one pack per day for the past 47 years presents with progressive shortness of breath and chronic cough, productive of yellowish sputum, for the past 2 years. On examination he appears cachectic and in moderate respiratory distress, especially after walking to the examination room, and ...
COPD case study copd is chronic inflammation of the airways, which leads to structural changes in the lungs. in response to inhaled irritants the immune system. ... Nursing Management Of Adult With Acute/Chronic Health Problems ( NUR 0082) 17 Documents. Students shared 17 documents in this course. University
This clinical case report highlights the usefulness of FEF 25-75 evaluation in early COPD diagnosis and monitoring and confirms the efficacy of LAMA-LABA association for small airways obstruction treatment. Keywords: COPD, LAMA, LABA, FEF25-75, Treatment. Abbreviations: COPD, chronic obstructive pulmonary disease; LAMA, long acting muscarinic ...
Joan Walker is an 84-year-old female who has had a productive cough of green phlegm that started four days ago that continues to persist. She was started three days ago on prednisone 40 mg PO daily and azithromycin (Zithromax) 250 mg PO x5 days by her clinic physician. Though she has had intermittent chills, she had a fever last night of 102 F ...
In this case-based module, Dr Toni Hazell discusses the diagnosis, treatment and prevention of measles and whooping cough, including how to identify and manage suspected cases, what appropriate treatment should be given in primary care and how to support improved uptake of vaccination against these serious infectious diseases. Learning objectives With the concerns about ongoing outbreaks of ...
These case studies served as focal points for methodological reflections within our QLR design. We have intertwined experiences from diverse research projects to underscore shared learnings, while also preserving the unique nuances of each case study. ... For example, in the studies on experiences of COPD (study 3) and knee joint replacement ...